As an intraocular implant, the Light Adjustable Lens™ (LAL®) from RxSight® stands alone. The LAL is the first and only lens that can be customized after cataract surgery, a significant improvement from relying on preoperative predictions to achieve the best possible refractive outcomes.
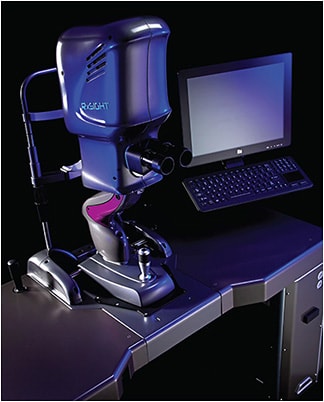
Following implantation of the LAL (which is made of photo-sensitive macromers) and time for healing, patients live with their new lenses in the real world for a predetermined period. At a series of follow-up appointments, they convey their visual preferences to their eyecare provider based on this “test driving.” The doctor adjusts the shape and focusing characteristics of the lens accordingly through a series of in-office, noninvasive UV treatments delivered with RxSight’s proprietary Light Delivery Device™ (LDD™).
Recently, we invited some early adopters of the LAL to discuss its impact on their patients and their practices.
VERSATILITY & RELIABILITY
John Doane, MD: In your experience with the Light Adjustable Lens, did you have an “aha!” moment about the outcomes you were achieving or the technology’s impact on the growth of your practice and your premium IOL channel?
John Vukich, MD: I knew we were on to something when patients, including septuagenarians and octogenarians, were seeing 20/15 and 20/12 uncorrected at the end of their treatment. That was just not happening with any other advanced-technology IOL (ATIOL). With the LAL, we’re delivering consistent and reliable results. From a quality of vision standpoint, this is better than any ATIOL I’ve ever used.
Deborah Ristvedt, DO: The past 10 years have really been a journey as we tried to determine the best IOL technology for each patient and how we could truly individualize care. My “aha!” moment was when I realized the true joy the LAL brings to our practice. The patients, staff, and surgeons are all so excited about the results. We even ring a little bell to celebrate after a patient has the final light treatment that locks in the vision results.
It’s also exciting that the LAL is technically monofocal, so we have much less risk of glare and halo than with other advanced IOL technologies. However, as reported in a paper presented by Dr. Kerry Solomon at the 2022 ASCRS meeting, the lens has been found to have a broadened defocus curve in addition to providing precise distance vision.1
Dr. Doane: How do the ATIOLs you had used previously compare to the LAL, particularly on delivering the desired refractive outcome and the need for laser vision enhancement or IOL exchange?
Dr. Ristvedt: With previous advanced IOL technology, our options were more limited. Patients with ocular pathology, for example, would not be good candidates for earlier advanced lenses. The LAL increased my capture rate with advanced IOL technology because of its versatility and adjustability. Prior to the LAL, we had evolving technologies that were good but more difficult to individualize as much as we would have liked. We would try our best to provide the desired refractive outcome, but sometimes still not deliver and have to fine-tune with a laser treatment.
Dr. Vukich: Yes, many of us have had great success with other advanced-technology lenses, whether they were extended depth of focus (EDOF) or multifocal, but the reality is we also sometimes had unhappy patients. The occasional refractive miss was inevitable. We had an accumulation of patients who required an enhancement, and some who still felt dissatisfied or disappointed post-enhancement. I track my premium conversions every month, and the barrier to performance consistency with prior IOL technologies was causing my conversion rate to stall. I just don’t have that barrier with the LAL. It’s such a relief now to accumulate happy patients. That aspect of the LAL is what’s driving my enthusiasm and, quite frankly, my practice.
Dr. Doane: How do you leverage the advantages the LAL has over other advanced-technology lenses?
Dr. Ristvedt: The LAL is versatile. I use it in patients who may not be good candidates for a multifocal lens that splits or shifts light, and patients who want precise distance vision or precise monovision. I’ve also had success using the LAL for patients who have early drusen or mild glaucoma, such as an early nasal step where contrast sensitivity is a concern.
I’ve had success, too, in patients who had been unhappy with cataract surgery in the past. The LAL’s reliability allows me to be more creative in achieving vision goals.
Dr. Doane: Speaking of monovision, do you feel that we tend to recommend a bifocal, multifocal, or trifocal IOL even when a patient had done very well with monovision contact lenses? Sometimes they find their near vision with those technologies is not as good as it was. I think monovision in that scenario is a great place for the LAL.
Dr. Vukich: I don’t use the term “monovision” with patients. I use “blended vision,” because it is truly different. For monovision to be effective, a 1.50D or 1.75D disparity between the near eye and the distance eye is typically needed. Because the LAL has been found to have a broadened defocus curve, I often aim for a small amount of myopia in the near eye. Therefore, the eyes have binocular summation, not alternating suppression for near vs. far.
Even patients who have failed monovision in the past do well with LAL blended vision. Rather than talk about monovision and have a patient say, “Oh, no, I tried that and hated it,” I talk about blended vision.
Dr. Doane: Good point about the terminology. Also, with multifocality, the quality of the near-focused image is not the same as with blended vision and monofocal optics. Patients who were happy with image quality at near when they had monovision may find it’s just not as good if they go with a multifocal IOL. With the LAL, they like that aspect of their vision.
Dr. Vukich: Plus, a multifocal lens usually doesn’t deliver the tack-sharp distance vision that patients like. With the LAL, we can adjust to whatever distance vision patients want. Being able to make adjustments and allow patients to try the results in the real world drives satisfaction.
LASIK-LIKE OUTCOMES
Dr. Doane: Let’s talk more about the vision outcomes we’re achieving with the LAL.
Dr. Ristvedt: We’re consistently achieving LASIK-like outcomes. In the LAL commercial outcomes and usage evaluation we’re part of, 90% of LAL patients are achieving 20/20 distance visual acuity, seeing J2 at near.2 In our practice, all LAL patients measure less than 0.25D of manifest sphere, and they’re really celebrating the quality of their vision.
Key to the amazing results is that patients can “test drive” their post-op vision. It had been difficult to explain to patients what to expect from their vision with other ATIOLs. With the LAL, they can see for themselves in the real world. They decide how they want to use their vision and then we adjust the lens accordingly. It’s revolutionary. In the past, patients were understandably anxious about having surgery, and on top of that we were asking them to choose how they wanted to use their vision for the rest of their lives before they even knew what it would be like.
Dr. Doane: The results from the LAL commercial outcomes and usage evaluation are unlike any we’ve seen with an ATIOL. They look more like LASIK results. As Dr. Ristvedt noted, 90% of LAL patients are achieving 20/20 distance visual acuity and seeing J2 at near.2 Most of the patients have virgin corneas, but results are the same for eyes that don’t. LAL patients are 2x more likely to achieve 20/20 or better vision without glasses, and 93.5% are +/- 0.5D from the refractive target. Also, there have been 6x to 10x fewer outliers (20/40 or worse without glasses) than with other lenses.2
The small refractive errors that can be fixed with the LAL make all the difference for patient happiness. According to an economic study conducted by RxSight,3 the lens is definitely expanding the premium IOL channel. Data show that 40% of LAL patients would have received a monofocal IOL.3
Hunter Newsom, MD: I completely agree that results are LASIK-like. My patients’ quality of vision with the LAL is excellent. I’ve used the lens in one eye for some younger patients with early cataract, and they like their vision better than they did when they still had their natural lens. Being able to alter the shape of the IOL is an extremely powerful tool for producing the highest quality of vision.
Because of the depth of focus and quality blended vision we can achieve, we explain to patients that we use the first adjustment to fine-tune distance vision. In our practice, 98% of LAL patients have 20/20 uncorrected distance visual acuity. We also explain that subsequent adjustments can also aim for more myopia, generally in the nondominant eye. We let them know they may notice a little bit of sacrifice at distance binocularly, but generally this is small. Approximately 90% of our patients choose to have some extent of blended vision. In that group, 80% have 20/20 uncorrected binocular near vision.
Dr. Vukich: We don’t specifically talk about blended vision ahead of time with our patients. We tell them they’ll be able to try their vision on for size and we’ll adjust it until they find their happy place. We start by correcting both eyes for distance and can expect vision to be 20/20 or better. Also, we realized that if we have patients continue reading the chart at follow-up visits, rather than stopping after the 20/20 line, some see binocularly 20/15+ or 20/12.5. Many of them—for instance, pilots and golfers—love that and don’t mind using reading glasses, so we start their lock-in process right here. Approximately 30% of our patients fall into this category.
The other 70% of our patients say the distance vision is great, but they’d like some near vision.
Dr. Ristvedt: I’ve changed how I approach the first adjustment based on knowing that more than 80% of my patients want some uncorrected near vision. Unless we’ve specifically determined that the best possible distance vision is the main goal, I target the first adjustment for plano in the dominant eye and aim for a small amount of myopia in the nondominant eye.
Dr. Newsom: I do the same. I find that patients at plano and a small amount of myopia are happy. They do extremely well at distance, and a large number of them read at J2. Patients don’t perceive any loss in distance vision until we further adjust the nondominant eye.
Dr. Ristvedt: Another point about quality of vision with the LAL is patients don’t seem to go through a neural adaptation period as they do with other advanced IOL technologies. They experience high-quality vision from the get-go and throughout adjustments.
Dr. Newsom: Any patient who would benefit from having the best possible refractive correction would benefit from the LAL. As far as quality of vision, it beats glasses, it beats contact lenses. I feel it beats LASIK.
Dr. Ristvedt: Even if patients don’t mind wearing glasses after cataract surgery, wearing multifocal glasses potentially increases their risk of falls.4 By using the LAL, which has been found to have a broadened defocus curve and provides high-quality vision, we may be helping more patients than we thought possible with an ATIOL.
A PRACTICE-BUILDING LENS
Dr. Vukich: If you would recommend a monofocal IOL for a patient, you can recommend the LAL. It’s not only an appropriate choice, but also a better choice. In addition, an advantage of the LAL over EDOF IOLs and multifocal IOLs is not having to screen for subtle pathology, such as mild dry macular degeneration, corneal guttata, or vitreous condensations.
Dr. Ristvedt: I completely agree. This lens is not just for tough eyes, not just for eyes that wouldn’t do well with other ATIOLs. It really is a lens for everyone. It’s versatile and it gives patients the opportunity to be less dependent on their glasses or reading glasses.
Dr. Doane: In the earliest days of the LAL, there was a sense that surgeons were using the lens as a niche technology. That has changed. Based on data from the LAL commercial outcomes and usage evaluation, the vast majority of patients had no previous ocular surgery.2
Dr. Newsom: Also, before the LAL was available, we would never recommend most ATIOLs for patients with perfectionist tendencies. We can offer them this lens.
Consider, too, the patients who may now be emmetropic, but their vision has dropped and they’re starting to get presbyopia, and they’re quite unhappy with the slight decrease in their vision. We used to wait 5, even 10, years before offering them any type of surgical correction, because we didn’t expect to achieve the precise results that these types of patients might expect. Now that we have the LAL, we can offer surgery to them sooner. We’re able to give them better binocular vision and make them happy again. It’s a significant practice-builder to have these two groups of patients as candidates for an ATIOL.
Dr. Ristvedt: The LAL has benefits related to astigmatism as well. Because it corrects down to 0.50D of cylinder, I can avoid relaxing incisions in more cases. Of course, it also addresses higher levels of astigmatism, which is helpful for precisely hitting the refractive target.
Dr. Doane: Right. It’s difficult to know whether to use a toric lens for a patient with 0.75D of corneal astigmatism. The LAL takes away that dilemma, because we can address after the fact whatever low level of astigmatism remains. We can also precisely address not only the magnitude but also the orientation.
Dr. Newsom: Yes, the issue with 0.50D to 0.75D of astigmatism is what axis to correct. I recently had a patient with 0.50D to 0.75D of cylinder at six different axes. For a patient like that, the LAL should be the standard of care.
Dr. Doane: As we discussed, it’s crucial to patient satisfaction to achieve 20/20 or better distance vision. If patients have 0.50D of residual astigmatism and aren’t plano sphere, they won’t be happy. They’ll say they’re unhappy because they can’t see road signs, the scroller on TV, names and numbers on jerseys on TV, etc. It’s a game-changer in outcomes when we can consistently achieve plano sphere for distance.
Dr. Vukich: Also, on the topic of practice-building, in less than 2 years, LAL has grown to 30% of the total number of cases in my cataract surgical practice. Contributing to that growth are more referrals from optometrists whose patients didn’t always have good experiences with EDOF IOLs or multifocal IOLs. They had to spend time talking about neural adaptation or urging patience with rings around lights. Now they’re sending me their patients because the LAL eliminates those issues.
There’s no question this has expanded my referral network. The LAL is considered state-of-the-art because it is, but it’s also known as trouble-free because we send ecstatic patients back to their primary eye doctors.
Dr. Newsom: We’re in a very competitive co-management market, and I’ve been talking about the LAL for several years. As soon as we began offering it, doctors who had never referred to us before began sending patients our way.
Dr. Doane: What has been your experience with return on investment (ROI) since you incorporated the LAL into your practice?
Dr. Vukich: As with any new technology, the investment needs to be considered. The Light Delivery Device (LDD), which adjusts and locks in the lens, is a capital expenditure. We decided it was important to acquire this cutting-edge technology and were willing to accept it might take time to earn back our spend. In reality, within 3 months the LDD had paid for itself. It quickly became a significant profit center.
Obviously, ROI depends on how many patients you convert, but it’s self-fulfilling. It’s easy to tell patients they’ll get the best possible outcome with this lens, and it organically starts to take over. Adopting the LAL is one of the best investments I’ve ever made as far as ROI.
Dr. Doane: The growth strategies for the LAL and what we’re able to achieve in our patient population are going to be very close to what we do with laser vision correction. It’s a practice change for the better that gives us a long glide path of 5 to 10 years growth. Everybody benefits: the doctors, the practice, but most importantly, the patients benefit from awesome vision results.
Dr. Newsom: Practices should compare the monthly revenue-generating potential of the LDD with the potential of any other fixed device they use, such as a perimeter or an OCT instrument. Viewed in that context, you can’t afford not to have this technology. We now have five LDDs in our practice.
Dr. Doane: Good point. In general, we can’t bill for using an autorefractor or a topographer. We obtain diagnostic information from them but aren’t able to pay for the device by billing for procedures. However, each time we use an LAL and the LDD, revenue comes into the practice. According to the RxSight economic study I mentioned previously, the average time to the break-even point is 6 to 9 months.3 For many practices the time is less.
THE HAPPY FACTOR
Dr. Doane: How quickly did your staff members adapt to the LAL and the associated workflow changes?
Dr. Vukich: The post-op visits require chair time because we refract, dilate, and deliver the light adjustments. Patients are in the office for approximately an hour, and additional office space is consumed. The most challenging part is figuring out the best way to schedule.
Yet staff buy-in is easy, organic. Once patients come back to the office after their first adjustment and they’re effusive about their vision, the staff understands the value of the technology. They know when the time comes, they’ll choose the LAL for themselves and that it’s the right lens for their parents.
Dr. Doane: I find the amount of labor associated with the LAL and with multifocal IOLs to be similar. The difference is where the labor is directed. When we’re dealing with multifocal technology, most of the labor is on the front end. We’re explaining potential postoperative vision disturbances, potential reduction in contrast sensitivity, etc. That’s quite a bit of work. Then, on the back end, we may be spending chair time handholding and explaining why patients’ vision—even if it’s 20/20 and J1—isn’t exactly what they expected.
With the LAL, the front-end work is so much easier, and the LAL work on the back end is happy work. Patients are happy, staff members are happy, and we’re not dealing with unwanted outcomes.
Dr. Newsom: It’s good chair time vs. bad chair time. The LAL chair time is good because we’re sharing with patients the success of the adjustments as we go through the process.
Dr. Ristvedt: When we brought in the LAL, we tried to simplify the process for the technicians. We include a dilated pupil measurement in every cataract evaluation. That way, if a patient wants an LAL, we already know whether the extent of dilation will be sufficient. We use the FORD method (Family, Occupation, Recreation, Dreams) to get a solid understanding of what each patient does on a day-to-day basis. The technicians document that information for every patient. After surgery, the technicians go through the history of present illness with patients to learn what they wish they could be doing more of without glasses. These steps set us up nicely to understand how patients are seeing and what they want as they go through this journey.
Additionally, using pledgets for dilation has helped with efficiency. We insert pledgets, then send patients out to the waiting room or for a cup of coffee for a half hour. That saves us from having to administer more drops for slow dilators, and patients feel as if they’re getting a break in the process.
Dr. Doane: Dr. Newsom, you were involved in the FDA studies that led to approval of the LAL, which was before the introduction of the ActivShield™ technology. How has ActivShield affected the surgeon, patient, and practice experience?
Dr. Newsom: ActivShield is an update to the LAL. It’s a UV-protection layer built into the lens. Before this was available, the only way to prevent ambient UV light from altering the shape of the lens in unwanted ways was patient compliance with instructions to wear the UV-blocking glasses. If a patient came in with a vision complaint, we had to worry that the UV glasses weren’t being used. We did have a few patients who admitted to not wearing the glasses, and we had to explant their LALs. Since ActivShield was introduced, the concern about having an abnormal change in lens shape has gone away.
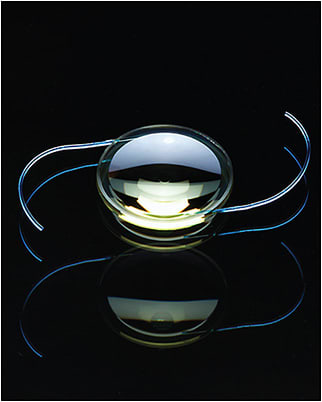
ActivShield is a built-in UV-blocking layer that, along with protective glasses, keeps ambient light from altering the lens shape between in-office adjustments.
Dr. Doane: ActivShield has been anxiety-relieving for patients as well. They don’t have to think things like, “What if I take my protective glasses off while I shower? Will I ruin my lens?”
Dr. Ristvedt: It gives us peace of mind when we want to wait longer to start optimizing the LAL and perhaps even longer before we lock in the prescription to make sure nothing is fluctuating.
Dr. Doane: What would you say to surgeons who aren’t interested in the LAL because their outcomes are already good?
Dr. Newsom: I’d say that if surgeons were to compare their current results with the results being achieved with the LAL, they would clearly see the LAL is better by far. We’ve been involved with the most popular multifocal IOLs, and about 40% of our patients have 20/20 uncorrected distance and 20/20 uncorrected near vision with those fixed-shape lenses. In contrast, we’ve reached 20/20 uncorrected distance and near vision in 80% of our LAL patients who chose some extent of blended vision.
I’ve also heard more than one lecturer say that most great cataract surgeons have 80% of their postoperative patients within 0.50D of the refractive target. They proceed to say that 90% is the “holy grail.” Well, the LAL is already there.
Dr. Doane: I agree wholeheartedly. The LAL has made it obvious that hoping to achieve plano by basing cataract surgery on preoperative data is not ideal. For LAL patients, we adjust the postoperative refraction, and we’ve never seen results as good.
Dr. Doane: Why is it wise to invest in the LAL right now?
Dr. Ristvedt: It’s time to involve patients in their vision journey. They’re living longer, are more active, and want to be less dependent on glasses. It’s time to invest in technology that empowers them to say, “Yes, this is the vision I want.”
Dr. Vukich: We’re past the point of early adoption for the LAL now. This is not a fad. Practices that don’t participate will be left behind. If you want to have a thriving practice that offers the best technology, you simply have to offer this.
Dr. Doane: If you want to have happy patients, work with the LAL. The happy factor is incredible. The number of patients referring friends and family for this technology far exceeds anything I’ve ever seen. There’s no comparison, in my experience.
Dr. Newsom: Reimbursement for just about everything we do in ophthalmology is being cut. We need to succeed in the refractive market to survive and thrive. As we discussed previously, the current multifocal/diffractive IOL sector has been stuck for a long time at around 10% of the market.5 The only way to get past that is to offer the IOL with the highest quality over a range of correction, which is the LAL.
Dr. Doane: A doctor who recently visited me asked, “What about the next multifocal?” My answer: The next multifocal will give the same type of results as the prior eight multifocals. It’s inherent in bending light. At the end of the day, quality of vision is the winner. I’d venture to say that the only way to take acceptance of ATIOLs past its current 10% of market share is the LAL.5
Dr. Newsom: I say with confidence that adjustability will become the standard of care for every IOL.
REFERENCES
- Solomon KD, Potvin RJ, Sandoval, HP. Visual Outcomes of Patients Bilaterally Implanted with the Light Adjustable Lens™ (LAL). Paper presented at ASCRS 2022 April 23, 2022.
- Vukich, J. Multicenter Study: Visual Outcomes in Patients Bilaterally Implanted with the Post-Op Customizable Light Adjustable Lens (LAL). Paper presented at ASCRS 2023 May 7, 2023.
- Haffey & Co; 2022 Economic Survey of LAL Customers.
- Lord SR, Dayhew J, Howland A. Multifocal glasses impair edge-contrast sensitivity and depth perception and increase the risk of falls in older people. J Am Geriatr Soc. 2002 Nov;50(11):1760-1766.
- 2023 IOL Market Report: Global Analysis for 2022 to 2028, April, 2023.








