Creating an affordable community health screening provides the opportunity to identify, educate, diagnose and promote the treatment of eye diseases in communities both inside and outside of a formal health-care setting. Early detection and treatment can help reduce the cost of care as well as improve patient outcomes through the promotion of health literacy and preventative health-care services. Additionally, affordable screenings allow ophthalmologists and allied health professionals to reach more patients and broaden access to care.
This is evident in prior community glaucoma screenings, such as the Los Angeles Latino Eye Study that surveyed more than 6,000 participants,1 and, more recently, the Michigan Screening and Intervention for Glaucoma and Eye Health Through Telemedicine (MI-SIGHT) program that has screened more than 3,000 participants.2 By working closely with members of the community and educating office staff and key team members, more insight may be provided into the ocular conditions affecting the community.
In this article, we will discuss several steps for creating a simple successful glaucoma health screening program.
DEFINE YOUR PURPOSE AND IDENTIFY GAPS IN CARE
In creating a community screening program, it is important to understand the needs of the population being served, particularly its language, culture and local presence. Although most vision screenings at community health fairs test visual field and visual acuity, new, less time-consuming and more affordable techniques are now available to help screen for glaucoma both within the community and in office settings at no cost to the patient.
Detecting glaucoma is especially important for individuals over the age of 40 who may be asymptomatic and/or unaware of their diagnosis. Additionally, people may be unaware of the risk factors that increase their susceptibility to glaucoma or may lack access to treatment. This is especially true in areas with significant diversity in age, race, ethnicity and access to care. Our team in New York identified this gap in care and created an affordable, effective solution for reaching patients through community glaucoma screenings.
We located screening sites by reaching out and partnering with local community leaders, especially those associated with churches, government, senior centers or local events. In doing so, we requested the entity provide a table and chairs for setup. We were responsible for bringing our screening equipment, which included hand-held tonometers, pachymeters, pens, forms, alcohol swabs and information to hand out to the community. As a result of our outreach, our sites varied and included indoor venues, such as the Jamaica Center for Arts & Learning and Allen Community Senior Citizens Center, as well as outdoor events such as a community fair outside of Morning Star Missionary Baptist Church. Through our interactions with community members, these screenings were also a great opportunity to educate people about obtaining routine medical examinations.
SELECT SCREENING TOOLS
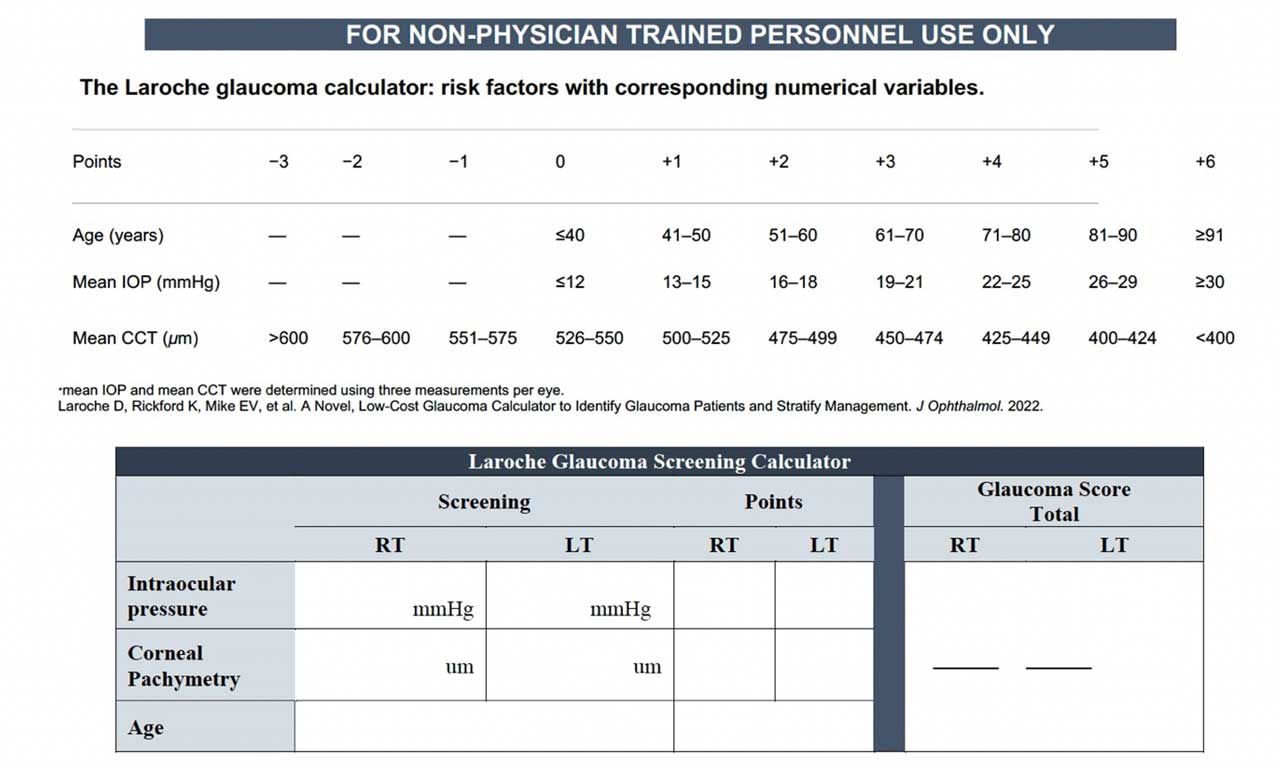
To best serve each community, our team chose to focus on promoting the early detection of glaucoma by using the Laroche Glaucoma Risk Calculator, as shown in Figure 1.3 This calculator uses patient age, IOP and corneal thickness to assess glaucoma risk and provide these patients with education, additional testing and subsequent referral for care and monitoring. Preliminary findings using this calculator demonstrated high sensitivity (93%), which is of utmost importance in a screening tool.3 This does not require more expensive ophthalmoscopy, visual field or fundus photos for the screening.
When selecting screening tools, it is also important to be mindful of the time it takes to screen the patient. Our screenings lasted approximately 10 to 15 minutes per participant, including consent and patient education. Another community glaucoma screening program, known as the Philadelphia Telemedicine Glaucoma Detection and Follow-up Study (PTGDFS),4 demonstrated a mean vision screening time of 22.7 minutes, which was still less than the standard out-patient ophthalmology clinic visits that last closer to 40 minutes.5
In screenings, the tools should be quick and effective in collecting information. Hand-held tonometry and pachymetry machines provide mobile, affordable options for screenings. We use the Tono-Pen Handheld Tonometer (Reichert) and Pachmate 2 pachymeter (DGH). In addition to community settings, ophthalmic technicians can be trained to offer free screenings during patient downtime in medical offices if permissible.
Patients identified by the calculator as “high-risk” at our screenings are referred for a comprehensive ophthalmic exam. Our own research showed the calculator was 91% accurate and 93% sensitive in correctly identifying patients with glaucoma and glaucoma suspects following our screening and complete ophthalmic examination of 403 eligible community members.
CULTIVATE A RELIABLE TEAM
Community and in-office free health screenings serve as an opportunity for trained medical personnel to apply their skills to improve the health of community members under the supervision of a trained physician.

Our team consists of highly motivated medical students and in-office health-care technicians trained by Dr. Laroche to use the hand-held tonometer and pachymeter (Figure 2). Following a detailed training session, each medical student volunteers to conduct glaucoma screenings, which includes interviewing and educating patients, as well as coordinating event logistics.
Many medical students and health-care technicians who seek opportunities to learn about ophthalmology can apply their skills under physician supervision and are an excellent addition to community health screenings both in and out of the office. Engaging these candidates also offers an opportunity to increase workforce diversity by training personnel from different cultures to assist in emphasizing the importance of screenings to their respective communities in their shared language.
IMPROVE PATIENT AND PROVIDER KNOWLEDGE
Although community members may have heard of glaucoma, many do not understand how this condition can lead to asymptomatic vision loss. We utilize carbon transfer paper in our screenings, which creates multiple copies of inscribed information. By doing so, we are able to collect data from the screening for research purposes while providing patients with a copy of information to take home and to any subsequent in-office visits. Community members are provided two documents, which includes a copy of the consent form, their risk score from the Laroche Glaucoma Risk Calculator (Figure 3), literature regarding glaucoma with contact information to schedule follow-up.
The medical team can also take advantage of health screenings to learn more about the community, such as understanding barriers to care that its members may face. For example, we learned that although 85% of community members that completed the glaucoma screening had a general medical exam in the past 12 months, fewer than 70% have ever had an eye exam.

PROMOTE CARE-SEEKING BEHAVIOR
Many community members shared plans of bringing their personal copies of their eye health data obtained from the glaucoma screening to the ophthalmologist, which suggested a tangible next step in their plan of care. Of the 525 patients that completed glaucoma screenings, 403 (77%) followed up — walk-in persons who had an appointment for a free screening had the highest rate of follow-up.
To improve the probability of follow-up, the participants’ phone numbers were voluntarily collected during screening to provide reminders to seek care — a place to include phone numbers was included on the consent form. Participants could voluntarily enter this information, although it was not required to take part in the screening. Additionally, we notified members of the community about two locations for follow-up to reduce barriers in access to care.
Our team was strategic in choosing which community events to conduct screenings to give our participants the best chance of accessing follow-up care. This included screening in locations that were located within a 10-mile radius of the follow-up appointment, which often included Harlem and Queens. Additionally, most screened participants were able to interact with the ophthalmologist that would complete their follow-up care, helping to build patient-physician trust before the complete ophthalmic examination.
We used handouts to educate participants on how to access insurance and follow-up for care. These included information on glaucoma and instructions on how to access ophthalmic care. Supplementary information on acquiring insurance was provided in the medical office setting.
The last step of following up connects members of the community to a formal health-care setting where they can have a comprehensive eye exam and receive personalized recommendations that exceed what can be completed at a health screening. Many patients at the community glaucoma screenings expressed concerns about the diagnosis of other eye conditions in addition to glaucoma, which was demonstrative of knowledge-seeking behavior.
Other studies, including the PTGDFS, showed a high rate of ocular pathology identified on complete ophthalmic examination following failed vision screenings.6 It is important for health-care providers to encourage patients to seek individualized care to have these questions answered.
Currently, many patients with glaucoma in the United States do not know they have the disease. Targeted glaucoma screenings in higher risk populations (ie, those with age over 50 years and Black and Latino communities) with the Laroche Glaucoma Calculator can play an important role in reaching those who are unaware of their disease. This is an effective way to educate people and empower them to educate their family members to get routine eye and medical checkups. OM
REFERENCES
1. Varma R, Ying-Lai M, Francis BA, et al. Prevalence of open-angle glaucoma and ocular hypertension in Latinos: the Los Angeles Latino Eye Study. Ophthalmology. 2004;111(8):1439-1448.
2. Newman-Casey PA, Musch DC, Niziol LM, et al. Michigan Screening and Intervention for Glaucoma and Eye Health Through Telemedicine (MI-SIGHT): Baseline Methodology for Implementing and Assessing a Community-based Program. J Glaucoma. 2021;30(5):380-387.
3. Laroche D, Rickford K, Mike EV, et al. A Novel, Low-Cost Glaucoma Calculator to Identify Glaucoma Patients and Stratify Management. J Ophthalmol. 2022;2022:5288726. Published 2022 Jul 31.
4. Hark LA, Myers JS, Ines A, et al. Philadelphia Telemedicine Glaucoma Detection and Follow-up Study: confirmation between eye screening and comprehensive eye examination diagnoses. British Journal of Ophthalmology. 2019;103(12):1820-1826.
5. Arias López MC, Lanuza García A, García García N, Ramos Martí F. [Evaluation of the work time used in outpatient ophthalmology techniques]. Arch Soc Esp Oftalmol. 2001;76(3):159-163.
6. Hark LA, Katz LJ, Myers JS, et al. Philadelphia Telemedicine Glaucoma Detection and Follow-up Study: Methods and Screening Results. Am J Ophthalmol. 2017;181:114-124.