As we sat together in the preceptor room at Bellevue Hospital one Monday afternoon, I overheard my glaucoma friends mention that cornea, as a subspecialty, is becoming more and more office-based and therefore less enticing for our residents to pursue as a fellowship. Glaucoma, on the other hand, is becoming more desirable as it is quickly changing with new technologies, including micro-invasive devices, making the disease more manageable and indeed even more exciting for the cornea as we move away from topical therapies.
As the only cornea specialist in the room, I couldn’t help but quietly disagree and be proud of my subspecialty. What this meant to me is that we as cornea specialists had figured things out — in a relatively short time!
SOLVING THE CORNEA PUZZLE
As you read this issue, you will see how quickly we have evolved from penetrating keratoplasty being the standard of care for many different corneal diseases to each disease having a much more precise and less invasive treatment, many of which can be done in the office setting or may soon be able to be done outside of the OR.
This is exciting! We have broken the cornea down and solved the puzzle! Why wouldn’t I be proud of that? We have perfected our techniques to expect 20/20 vision with cataract surgery, endothelial keratoplasty, laser vision correction, and contact lens fitting for irregular but stable corneas. We have straightforward algorithms with repeatable and predictable results. We perform the most successful surgeries in the world! We can now focus on other things.
TAKING ON NEW CHALLENGES
With these advancements, we can use our skills and experience to safely delve into new areas. A perfect example is a patient of mine of 19 years who had congenital cataracts and surgery abroad as a baby. Both eyes were left aphakic, but one eye suffered complications and eventually became NLP, or no light perception. He followed with us at Coney Island Hospital as an adult, when I was a resident, where we would perform ethylenediaminetetraacetic acid, or ETDA chelation, for painful episodes of corneal epithelial breakdown from severe band keratopathy.
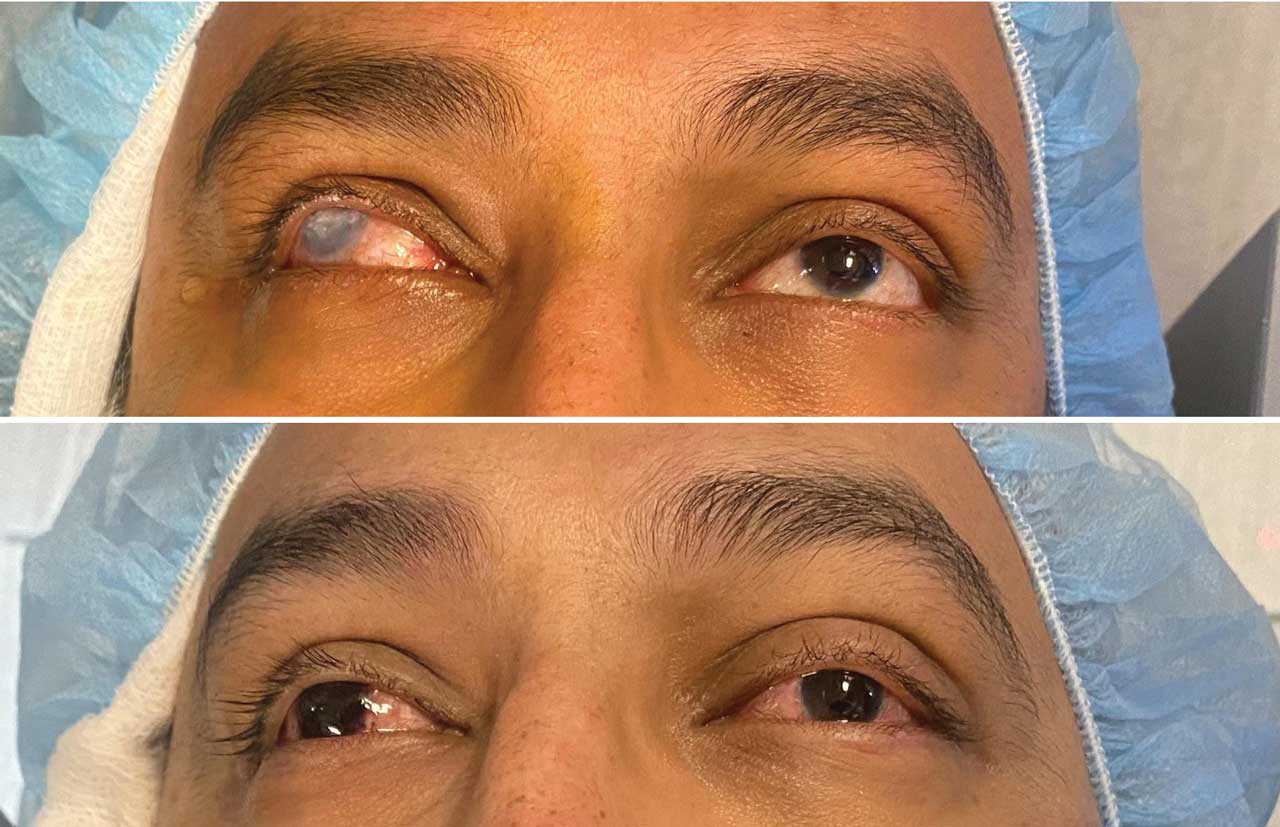
Eventually, his corneal epithelium thickened and the band keratopathy stabilized; however, he was left with a whitened cornea that bothered him cosmetically. He followed me to my practice when I became an attending, and for years we discussed different options for cosmesis. The corneal curvature was too steep and irregular to fit a cosmetic soft contact lens. And, with an aphakic refraction in the one good eye, it would be difficult for him to place any type of contact lens. We discussed the possibility of corneal tattooing for a couple of years.
MY FORAY INTO TATTOOING
In fall 2023, Dr. Roberto Paneda came to NYU Langone as a visiting professor. With his guidance and permission from our chair, Dr. Kathryn Colby, we performed the tattooing procedure on April 30. We used the FS200 (Alcon), and although the laser could not penetrate through the densest corneal scarring, we used the partial pocket and an anterior stromal puncture technique to complete the procedure.
I would like to acknowledge the great work our colleagues in Brazil are doing on this front, including Dr. Giovanni Garotti, who was honored as one of the best cornea posters submitted to ASCRS 2024. Please note that these techniques are used on blind eyes. This is a brilliant art form we can add to our skill set as corneal surgeons and artists!
Thank you all for reading this issue. Your thoughts and feedback mean the world to us, so please reach out with any questions, comments and concerns. OM









