This article was originally published in a sponsored newsletter.
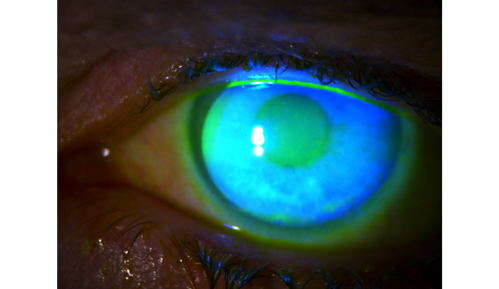
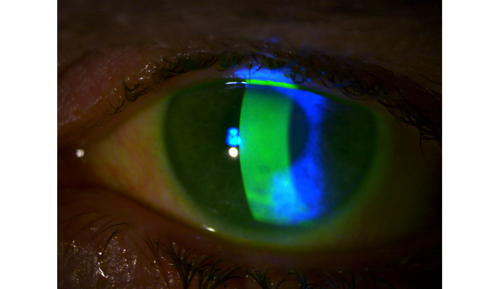
Most cornea, cataract and comprehensive ophthalmologists will encounter patients with mild to moderate glaucoma. If their disease is stable and their intraocular pressure (IOP) is well controlled on topical drop therapy, they can be managed comfortably by a glaucoma, cornea or comprehensive ophthalmologist. However, many of these patients will develop ocular surface disease (OSD) or toxicity and exacerbation of dry eye syndrome (DES) from preservatives in their glaucoma drops (see Figures 1 and 2).1,2
Clinical trials demonstrate that few patients must be taken off their glaucoma drops due to adverse effects on the ocular surface, but that is not real-world experience. Patients in the real world often take multiple drops concurrently during their lifetime, rather than for the 6- to 12-month duration of a clinical trial. Many patients also have comorbid conditions such as existing dry eye, blepharitis and ocular rosacea, which are often excluded from clinical trials. In the real world as well, the prevalence of OSD is much higher than reported in clinical trials: At least half of glaucoma patients report OSD, but signs of OSD can be found in almost 80% of patients.3
The main culprit, benzalkonium chloride (BAK), causes irritation and inflammation, and magnifies the symptoms of existing DES. Despite its effects, BAK continues to be found in many generic glaucoma medications. All ophthalmologists managing OSD and DES in glaucoma should seek to reduce patient exposure to this preservative, starting with the strategies outlined here.
1. Manage co-morbid conditions
Initially, physicians should investigate common causes for dry eye with a detailed history, especially if patients have been on glaucoma drops without issue for many years. Blepharitis, meibomian gland dysfunction (MGD), eyelid issues such as floppy eyelids and lagophthalmos, rosacea and chronic allergy can be treated to reduce symptoms. Treatment of dry eye with artificial tears, topical cyclosporine (Restasis, AbbVie; Cequa, Sun Ophthalmics) and lifitegrast (Xiidra, Bausch + Lomb) is recommended. While punctal occlusion lubricates the ocular surface, it may cause retention of more IOP-lowering drugs and amplify side effects.1
2. Transition to alternative preservatives or preservative-free formulations
Several BAK-alternative or preservative-free glaucoma drops are available. For example, alternative preservatives are used in formulations of brimonidine and tafluprost, while timolol, latanoprost, tafluprost and dorzolamide-timolol have preservative-free formulations.
3. Reduce drop burden
OSD is compounded in patients who take more than one drop to control their IOP. Overtreatment and overdiagnosis of glaucoma occurs worldwide and is evident in population-based studies.4 A close examination of testing to determine if patients truly have glaucomatous disease and require treatment is a straightforward way to reduce drop burden. Selective laser trabeculoplasty, alternative drug delivery (bimatoprost intracameral implant, Durysta, AbbVie and travoprost intracameral implant, iDose TR, Glaukos), minimally invasive glaucoma surgery (MIGS) or traditional glaucoma surgery will also lower IOP to decrease drops.
References:
- Kolko M, Gazzard G, Baudouin C, et al. Impact of glaucoma medications on the ocular surface and how ocular surface disease can influence glaucoma treatment. Ocul Surf. 2023 Jul;29:456-468. doi:10.1016/j.jtos.2023.05.012
- Stewart WC, Stewart JA, Nelson LA. Ocular surface disease in patients with ocular hypertension and glaucoma. Curr Eye Res. 2011 May;36(5):391-398. doi:10.3109/02713683.2011.562340
- Leung EW, Medeiros FA, Weinreb RN. Prevalence of ocular surface disease in glaucoma patients. J Glaucoma. 2008 Aug;17(5):350-355. doi:10.1097/IJG.0b013e31815c5f4f
- Founti P, Coleman AL, Wilson MR, et al. Overdiagnosis of open-angle glaucoma in the general population: the Thessaloniki Eye Study. Acta Ophthalmol. 2018 Nov;96:e859-e864. doi:10.1111/aos.13758










