Vision correction surgery in patients with low amounts of myopia (in the -1.00 D to -4.00 D range) are some of the most satisfying cases refractive surgeons are privileged to perform, and continuous technological advancement in the field has provided more solutions to treat low myopia than ever before. In addition to the foundation of LASIK and PRK, procedures such as STAAR Surgical’s EVO Implantable Collamer Lens (ICL), laser-assisted lenticule extraction (LALEX; aka small incision lenticule extraction [SMILE] or smooth incision lenticular keratomileusis [SILK]), or even Intacs (Addition Technology) and/or crosslinking for those with irregular corneas can provide freedom from glasses and contact lenses. With so many procedures available now, refractive surgeons must make a concerted effort to discern the best possible vision correction procedure for every eye based on current literature and state-of-the-art practice patterns.
ICLS BREAK NEW GROUND
Refractive surgery is a field that innovates quickly, so understanding current technology and being able to offer up-to-date procedures to patients assures that you are always providing the best care. An anecdote that captures the prevalence of a fixed mindset regarding refractive surgery options is something that coauthor, Parkhurst NuVision fellow and ICL patient
Dr. Hirabayashi hears frequently when telling others about his ICLs: “Wow you must have been a -10!”
While traditional teaching has resulted in the strong association between ICLs and high myopia, the FDA approval of the EVO ICL in 2022 was for a significantly expanded indication range that make these a great solution for patients, even at lower ranges of myopia down to -3.0 D.
With five ports allowing aqueous to flow freely, the risk for IOP problems and cataract formation has essentially been eliminated in the EVO model. Additionally, the ports have allowed for greater range in vault tolerance (how far the ICL sits above the crystalline lens). And with new AI-powered solutions to sizing on the horizon such as ICL Guru (Revai), an ICL sizing calculator and VAULT (vault accuracy using deep learning technology), an image-based AI model for predicting ICL postoperative vault, surgeons are sizing ICLs with greater confidence. ICLs require no large capital or footprint investment in lasers, and they have such an excellent safety and efficacy record;1,2 every refractive surgeon should offer them as a solution to myopia, and not just high myopia, in our opinion.
Parkhurst NuVision routinely implants ICLs across their treatment range, including for low myopes, with excellent outcomes (Figure 1). Dr. Hirabayashi (who had his ICLs implanted by Dr. Parkhurst) had a prescription of around -4.50 with sufficiently thick and healthy corneas to undergo laser vision correction, so they are certainly not exclusively reserved for high myopes.

The only FDA approved method for sizing ICLs is a caliper measurement of white-to-white diameter, but many nomograms exist that make use of several diagnostic devices common to most ophthalmology practices. Examples of these include the Parkhurst, Dougherty, Russo or Reinstein nomograms. ICLs have a low barrier to entry, a reasonable learning curve due to the overlapping skill set with cataract surgery and consistently excellent outcomes.
A FIT FOR EVERY EYE
LASIK has been the cornerstone of refractive surgery for decades, and to the general public, “vision correction” and “refractive surgery” are often synonymous with LASIK. LASIK is an excellent, safe procedure that benefits from decades of research and refinement. The latest advancements, wavefront optimized and topography-guided (eg, Alcon’s Contoura Vision) provide excellent and repeatable results. At our practice, Contoura has provided superb results.
Like the general public’s perception, many refractive surgeons often consider LASIK the “default” in the decision tree.
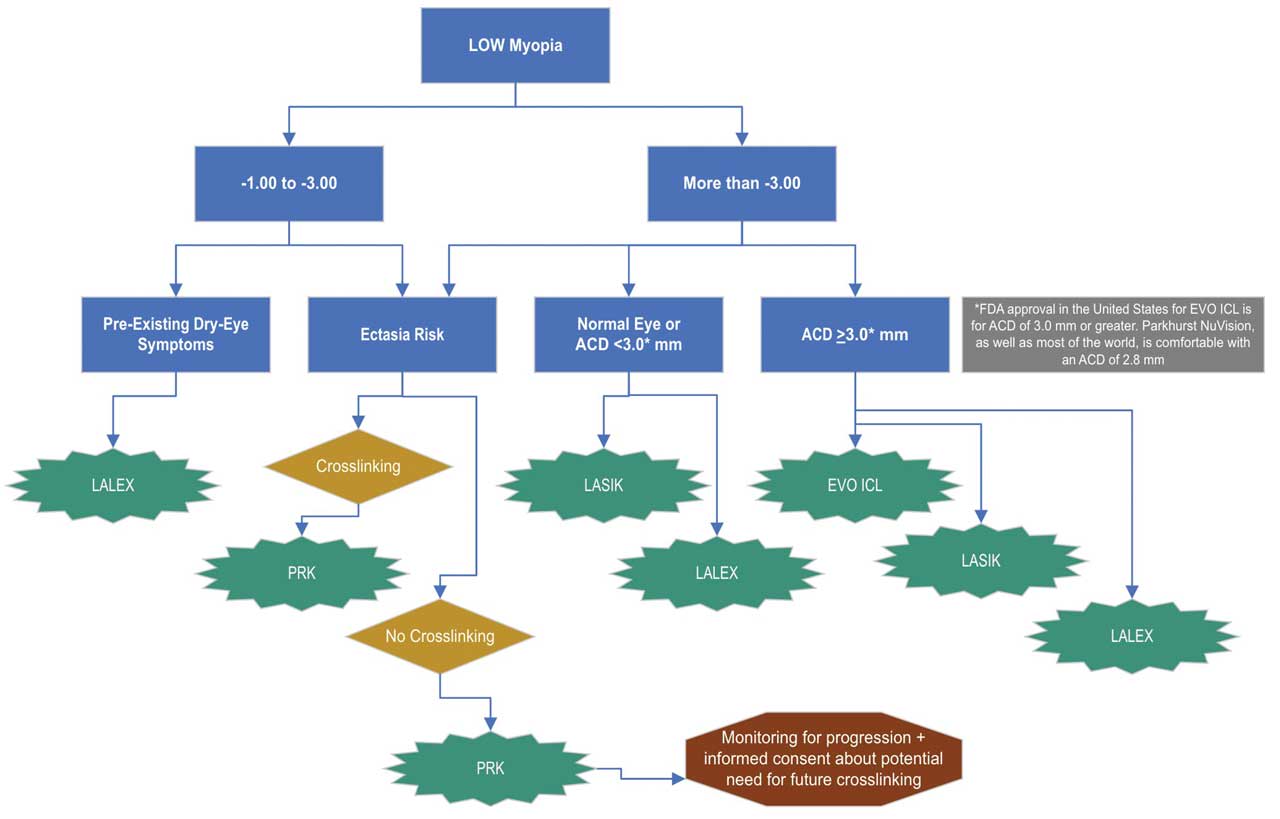
LALEX (aka SMILE or SILK) was FDA approved in 2016 with a myopic range for laser vision correction up to a spherical equivalent refractions of -11.0 D. Involving extracting a lenticule from the central cornea as opposed to creating a flap, it was initially thought to preserve more corneal structural integrity than LASIK and reduce ectasia risk, although recent literature shows they may be equally low by these metrics.3 Because the small incisions in LALEX may cause less manipulation of the corneal nerves and thus less surgical temporary ocular discomfort syndrome (STODS) compared to LASIK, LALEX might be a better consideration for some candidates with pre-existing dry eye symptoms.
PRK, in which the surgeon manipulates only the most anterior cornea and avoids creating flaps altogether, may be a fantastic option for some patients. At Parkhurst NuVision, about 5% of laser vision correction procedures are PRK and produce great results for patients. With less risk of ectasia compared to LASIK or LALEX, it can be a suitable procedure for low myopes with asymmetric or truncated astigmatism when the anterior chamber isn’t sufficiently deep for an ICL.
While all these options have their place, we believe that whenever possible — that is with myopia of >-3.00 D and an internal ACD of >3.0 mm — ICLs should at least be part of the discussion. Intraocular surgery may seem intimidating compared to the surface-based procedures, but the total reversibility of ICLs actually makes them less invasive from the perspective of many of our patients. The EVO model of ICL has reduced the risk of IOP, cataract or sizing problems so substantially that all refractive surgeons should feel confident offering this procedure to their patients.4
One limitation of ICLs is that they often cost significantly more than laser vision correction at most practices. The fact that laser vision correction has not kept up with inflation and frequently remains at the same price point it was 20 years ago, however, is an entirely separate discussion.
NEW PARADIGM
In general, for myopia from around -1.00 to -3.00, LASIK or LALEX will provide an exceptional patient experience. For patients who have existing difficulty with dry eye symptoms, LALEX might be favored. For corneas that are at somewhat increased risk for postoperative ectasia, PRK may be a great option and can be a rewarding experience for patients with the appropriate counseling (ie, the expectation of discomfort is appropriately set).
As soon as patients are in range of the EVO ICL (around -3.00 D) and their anterior chamber can accommodate the lens (with an internal ACD of 3.0 mm or greater) it should certainly be a consideration. Many surgeons have a “line in the sand” of -6.00 D that is supported by literature, after which point EVO ICL results in superior visual outcomes compared to the other options due to the proximity of the optic to the null point of the eye.5
See our (very simplified) flowchart of one way to think about matching the correct vision correction procedure to each eye (Figure 2).
CONCLUSION
Most refractive surgeons are drawn to this field because the focus is on optimizing vision and providing the best outcomes for patients. This is only possible by staying up to date with current technology and treating each eye (and each patient) individually when deciding on a procedure.
With LASIK, LALEX, PRK and ICLs available for the treatment of low myopia, we believe surgeons should be comfortable with each of these procedures and the clinical scenarios when each will provide the best possible outcome. Summing up:
- LASIK provides a great patient experience and has a wide range of indications
- Always consider ICLs when possible (myopia >-3.00 D and internal ACD >3.0 mm)
- For significant pre-existing dry eye symptoms, consider ICLs or LALEX
- For corneas with ectasia risk, consider ICLs or PRK. OM
References
1. Albo C, Nasser T, Szynkarski DT, et al. EVO/EVO+ Implantable Collamer Lens: Evaluating refractive outcomes in the largest single center study of ICL patients in the United States. Clin Ophthalmol. 2024 Jan 9:18:69-78.
2. Chen X, Li L, Rao J, et al. Long-term observation on safety and visual quality of implantable collamer lens V4c implantation for myopia correction: a 5-year follow-up. Int J Ophthalmol. 2023 Jul 18;16:1123-1129.
3. Randleman JB. Ectasia after SMILE, revisited. J Refract Surg. 2021 Dec; 37:798-799.
4. Packer M. The Implantable Collamer Lens with a central port: review of the literature. Clin Ophthalmol. 2018 Nov 27:12:2427-2438.
5. Perez-Vives C, Domingo-Vicent A, Garcia-Lazaro S, et al. Optical and visual quality comparison of implantable Collamer lens and laser in situ keratomileusis for myopia using an adaptive optics visual simulator. Eur J ophthalmol. 2012 Jul 30:0. Online ahead of print.









