Traditionally, many refractive surgery practices have centered their model around laser vision correction (LVC) offerings that the average patient is familiar with, including LASIK. Typically, these practices will offer photorefractive keratectomy (PRK) if patients are not an ideal candidate for LASIK, and a growing number of them are utilizing small incision lenticule extraction (SMILE), otherwise referred to as laser-assisted lenticule extraction (LALEX). However, there is another option outside of cornea-based procedures that the growing refractive surgeon can incorporate into their portfolio: implantable collamer lenses (ICLs).
As a cataract surgeon, it has been straightforward to implement ICL into clinical practice. But, from a business perspective, marketing this technology and educating patients on its role has taken a learning curve. My hope is to share my experiences and outline how to effectively utilize ICLs to grow your refractive practice.
Take-home points
- Sharing my journey of having ICL placement in my eyes with my patients helps when discussing ICL with them, because I can provide them comfort that their surgeon had the same procedure performed on his eyes.
- It’s important to discuss with the patient the pertinent risks of intraocular surgery, such as infection and the possibility of premature cataract formation.
- When explaining ICL as an option, I have found it effective to not mention price and only focus on visual recovery, the surgical experience and the safety profile.
- ICL can be positioned as a practice builder as an alternative to PRK — given that PRK has more discomfort and a slower recovery period, it has less of a “wow” factor.
- When incorporating ICL into your workflow, the essential workup a technician needs to perform for an LVC patient and an ICL patient is almost identical. The only additional steps we have our techs perform for an ICL patient is to obtain biometry and to make sure digital calipers are available for the surgeon to obtain a manual white-to-white measurement at the slit lamp.
- Technicians can show a patient diagrams/brochures and even ICL models while they are waiting for their consultation with the surgeon.
- An ophthalmologist who is looking to incorporate ICLs into their practice can also look towards their colleagues to see how they have succeeded with this technology.
HOW TO DISCUSS ICLS
When first discussing the use of ICLs as a refractive option, many ophthalmologists gravitate to their use in scenarios where LVC is deemed a contraindication. This is an accurate notion; I do believe there are many patients who would not be a good candidate for LVC and instead would be a great candidate for ICL. These patients may be those that have very high refractive error, thin corneas, excessive dry eyes or are at risk for ectasia (concerning posterior float on corneal tomography, suspicion for keratoconus or pellucid marginal degeneration among others). When consulting with these patients, it is easier to discuss ICL from the perspective of safety and risk reduction. For these patients, who are motivated to be eyeglasses or contact lens independent, ICL then becomes a “surgery of necessity.”
However, there is another way to position ICL in your practice, and this is what I will refer to as a “surgery of choice” for your refractive patients. For patients who have typical refractive error (moderate myopia, with or without astigmatism) and average/thick pachymetry with normal topography, they essentially have the entire refractive spectrum (LASIK, PRK, LALEX, ICL, refractive lens exchange) all open to them. At this point, I think it is important not to make value judgements for the patient. I focus the discussion on their goals and consider their age and hobbies/lifestyle. For our practice, our standard criteria to include ICL into the discussion is if the patient has an anterior chamber depth (ACD) (using a Pentacam [Oculus]) minimum of 2.7 mm and spherical equivalent of -6.50 or higher. At this point, I offer ICL alongside with LVC and mention the following key points:
- With ICL, I am not altering your cornea (I use the phrase “futureproofing”). This gives you more room for an LVC enhancement in the future. This also leaves you open to all possible IOL options when you have your cataract surgery in the future.
- ICLs are removable. This gives you flexibility in case new technology comes out that you wish to take advantage of.
- There is less prevalence of dry eye disease after ICL when compared to LVC.1
STRATEGIES AND EXAMPLES
Drawing on my personal journey
To elaborate on the point of offering ICL as a “surgery of choice,” I like to mention two cases that help illustrate how we utilize ICLs.
The first case centers around my own eyes. My MRx was -6.00-1.75x030 and -6.00-1.75x160 for right and left eyes, respectively. My pachymetry was 585/580, ACD by Pentacam was 3.19 mm and 3.12 mm. With these parameters, I essentially had any refractive surgery option available to me. However, with the understanding that I may need an enhancement in the future, and the desire to preserve my cornea for the time of cataract surgery, I elected for ICL placement in my eyes. Now I have an uncorrected acuity of 20/15 in both eyes, and I am thrilled with my vision.
Sharing this personal experience with my patients helps when discussing ICL with them because I can provide them comfort that their surgeon had the same procedure performed on his eyes.
Compare to other options
The second case was a 28-year-old woman who had an MRx of -2.50-0.75x170 and -2.50-0.75x002 in right and left eyes, respectively. However, her corneal thickness was 479 and 475, and her ACD was 3.54 mm and 3.52 mm. She was told she could get PRK, and after extensive research she decided to move forward with the surgery but wanted a second opinion.
I had a detailed pre-operative consultation with her and found out she is a nurse practitioner who was getting married in the next month. She said she would really like to have excellent vision as soon as possible, both for her job as well as in preparation for her wedding. She was very averse to dry eyes and worried about having to wear bandage contact lenses after PRK. ICL would improve her vision more rapidly than PRK and not result in further thinning to her already thin cornea. We also discussed pertinent risks of intraocular surgery including, but not limited to, infection and the possibility of premature cataract formation, and after answering her questions she was eager to have ICL performed instead of PRK.
The entire discussion did not mention price once and only focused on visual recovery, the surgical experience, and the safety profile. Historically, these low myope patients may not have discussed ICL with their surgeon, but given the right clinical scenario they may be good candidates for the procedure. In this case, it was an ideal blend of “surgery of necessity” and “surgery of choice.”
HOW TO POSITION ICLS
Building on that previous case, I believe that ICL can also be positioned as a practice builder as an alternative to PRK. Given that PRK has more discomfort and a slower recovery period, it has less of a “wow” factor. Patients are not impressed on post-op day one and thus are less likely to tell their friends and family about their experience. Some patients may even dissuade others from having refractive surgery based on their recovery. This reduction in word-of-mouth is a disaster to a growing refractive surgery practice. Consider a happy postoperative day one LASIK/LALEX or ICL patient who can bring in three to four more patients who feed into the pipeline and thus help provide for healthy growth of the practice. This reality is all the truer with social media and instant posting of one’s opinions on Instagram or TikTok.
With this view, I would argue that a successful practice should offer ICL to these formerly “PRK-only” patients. If they choose to go elsewhere to have PRK, from a business standpoint, it can still be considered a wise approach.
HOW TO INCORPORATE INTO YOUR WORKFLOW
Another aspect of incorporating ICL into your practice is the workflow with your current staff and technicians. Fortunately, the essential workup a technician needs to perform for an LVC patient and an ICL patient is almost identical. The only additional steps we have our techs perform for an ICL patient is to obtain biometry (we use a Zeiss IOL Master) and to make sure digital calipers are available for the surgeon to obtain a manual white-to-white measurement at the slit lamp. As far as discussion points for the techs, STAAR Surgical has done a wonderful job of marketing the EVO ICL. There are good diagrams/brochures and even ICL models that a technician can show a patient while they are waiting for their consultation with the surgeon. Celebrities like singer Joe Jonas and athletes like Max Strus are walking billboards for this technology, having chosen the EVO ICL
Furthermore, our practice has two surgeons with ICLs in their eyes that technicians can point to when illustrating the prevalence of ICLs. I know of other ophthalmology colleagues who have performed ICL surgery on local optometrists who then are able to talk to their patients and share their experiences.
CONCLUSION
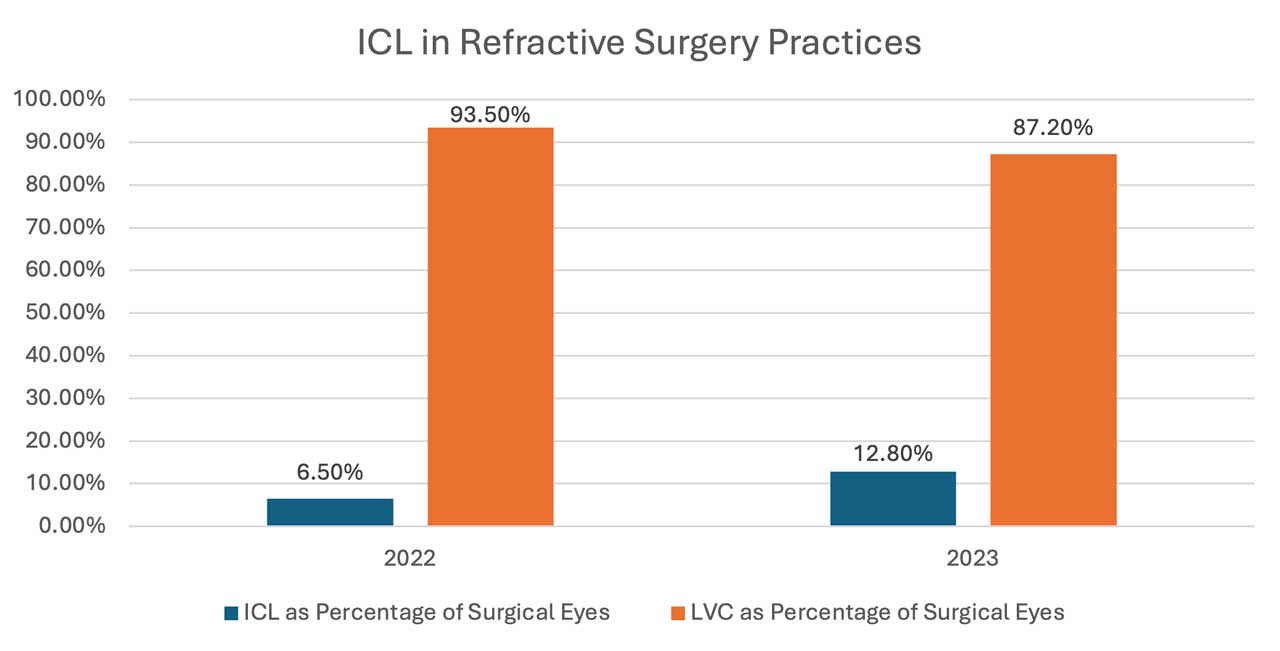
Looking at ICLs and their incorporation into refractive practices, we can see a general trend. Amongst a few refractive surgery clinics across the United States, the percentage of ICL surgery as a part of total refractive volume (ICL/LASIK/SMILE/PRK) was 6.5%. In 2023 the percentage of ICL surgery grew to 12.8% (Figure). This illustrates how ICL is gaining in popularity. I expect this trend to continue as more and more of the public are aware of ICLs. STAAR Surgical just reported 3 million ICLs sold globally as of March 2024.2
I hope this article has helped in showing you how to implement ICLs into your workflow and provided some tips on how to develop a natural discussion or talking point around ICLs with your patients. I encourage any ophthalmologist who is looking to incorporate ICLs into their practice to reach out to STAAR Surgical as they have a wonderful support team. Also, look towards your colleagues to see how they have succeeded with this technology. OM
Dr. William F. Wiley and Dr. Joseph J. Ling contributed to this article.
References
1. Gjerdrum B, Gundersen KG, Lundmark PO, Potvin R, Aakre BM. Prevalence of Signs and Symptoms of Dry Eye Disease 5 to 15 After Refractive Surgery. Clin Ophthalmol. 2020;14:269-279. Published Jan. 28, 2020.
2. STAAR Surgical Celebrates Three Million Implantable Collamer Lenses. Press release. March 18, 2024. https://investors.staar.com/press-releases/press-release-details/2024/STAAR-Surgical-Celebrates-Three-Million-Implantable-Collamer-Lenses/default.aspx. Accessed June 13, 2024.









