A steady stream of innovation in refractive cataract surgery in recent years has enhanced surgical precision and helped us to meet our patients’ high expectations. Many of these technological advancements are specifically designed to enhance the odds of achieving better uncorrected vision for our patients. Intraoperative refractive guidance systems are a perfect example of this innovation.
This category of technology consists of a group of devices and systems used during cataract surgery to help minimize postoperative refractive error. They offer guidance on incision placement, capsulorhexis size and centration, as well as lens power selection (both sphere and cylinder), toric lens alignment and multifocal lens centration.
These technologies are not covered by insurance; thus, as non-covered services, they can be billed directly to patients. For cataract surgeons looking to improve their refractive outcomes and provide cash-pay services, adopting one or more of the intraoperative refractive guidance systems detailed in this article may be an easy first step.
OPTIWAVE REFRACTIVE ANALYSIS (ORA) SYSTEM
The ORA System (Alcon) is a well-established example of the potential offered by intraoperative refractive guidance systems. The aberrometer attaches to the bottom of a surgical microscope and uses Talbot-Moiré fringes to measure the refractive state of the phakic or pseudophakic eye intraoperatively. Essentially, ORA uses a propriety biometric formula to suggest an IOL power during an aphakic measurement, and most surgeons will use aphakic measurements to determine IOL power for their patient, both sphere and cylinder (Figure 1). The patient’s biometry data, the selected lens, the target refraction, and formula are all entered into the AnalyzOR, a cloud-based software solution and database.

Postoperative refractive data are also entered — usually a technician, optometrist, assistant or the physician themselves will enter the information manually into the AnalyzOR — and the system periodically updates A-constants to adjust for the surgeon’s results to improve future patient outcomes.
When discussing ORA with my patients, I often explain to them that it provides another data point, and the more data points I have, the more precise I can be about their lens selection.
ORA for spherical power refinement
Kaufman and Pineda published a review on ORA in January 2023. For cases not involving prior refractive surgery, they found that ORA produced a modest yet statistically significant improvement in spherical equivalent refractive outcome vs preoperative calculations.1 In cases of extreme axial length, most studies suggest that intraoperative aberrometry does not outperform preoperative calculations and may be more beneficial in cases where emmetropia is targeted rather than moderate myopia. For patients with prior refractive surgery, ORA appears to be most beneficial in following myopic ablation. Knowing this, I encourage most of my post myopic LASIK patients to opt for ORA. Again, this provides another data point to help with the level of precision.
I often enter my cases with both a lens selected and a plan of what I am willing to adjust based on my ORA measurement (my notes will say “plan for 20.0, go to 20.5 per ORA”). It is important to keep in mind that some factors can result in measurement variability, including ocular surface irregularity, low IOP and the integrity of (or hydration of) corneal wounds. Surgeons should be cognizant of these changes and trust ORA measurements accordingly. For example, in patients with numerous radial keratotomy scars, the cornea might hydrate slightly during cataract extraction, making ORA measurements less accurate.
Additionally, vitreous floaters can sometimes impair the aberrometer. In such cases, I have the patient abduct the eye, then quickly re-fixate the “red light,” and I capture the image as quickly as possible. I find that this displaces some floaters long enough to capture a measurement.
ORA for cylinder power refinement

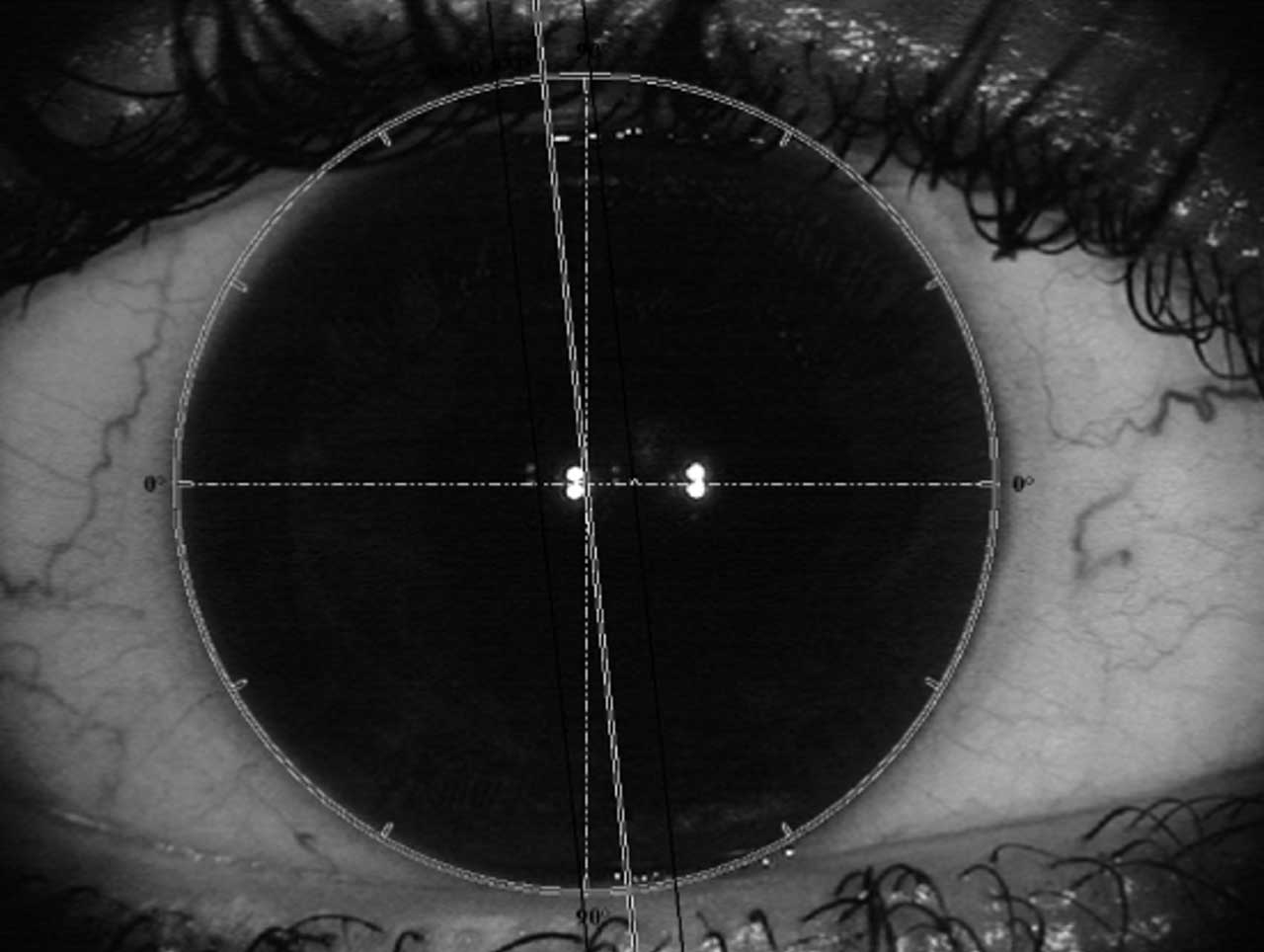
Another feature of the ORA system is its dynamic reticle, which displays real-
time streaming refractive correction (Figure 2). I turn it on as the toric lens unfolds then align my toric guided by the reticle. A pseudophakic “post-toric” measurement can then inform the surgeon of the residual cylinder and whether rotation of the toric IOL might reduce it. Kaufman’s review found that intraoperative aberrometry tends to result in minimal residual astigmatism in the postoperative period.1
Regarding cylinder power, we often enter the operating room with a patients’ preoperative astigmatism based on biometry and tomography and feel most confident when the two numbers are similar. ORA measurements provide a third data point that I often use as a “tie breaker” if there is a discrepancy in the preoperative data.
Finally, ORA can also be helpful in manually placing peripheral corneal relaxing incisions (PCRIs) and/or adjusting the opening of laser-created PCRIs.
VERION IMAGE GUIDED SYSTEM
The Verion Image Guided System (Alcon) consists of a preoperative reference unit and software that utilizes a high-resolution image of the patient’s eye for digital marking. Initially, Alcon had a separate Verion Reference Unit, which obtained preoperative measurements of corneal curvature as well as an image of the front of the eye. Axial length then was imported from another instrument, such as a biometer. Now, these functionalities have been transferred to Alcon’s Argos biometer.
Once measurements and images are obtained, Alcon Vision Planner software enables a surgeon to create a treatment plan that includes the phaco incision placement, arcuate incision placement, toric IOL positioning and IOL power selection. The digital marking and treatment plan can be transferred from the Vision Planner software to a Digital Marker that attaches to the Digital Marker LenSx laser (DML) to compensate for cyclotorsion when placing arcuate incisions. The data can also be transferred to a Digital Marker attached to a surgical Digital Marker Microscope that guides toric IOL axis positioning and creates “heads down” displays within a microscope eyepiece for incisions and the capsulorrhexis (Figure 3). This can be particularly helpful to resident physicians as they fine-tune their manual capsulorrhexis skills.

CALLISTO EYE
CALLISTO eye (Zeiss) is another intraoperative refractive guidance system that is designed to integrate the IOLMaster 500 or 700 and a Zeiss microscope, such as the OPMI LUMERA 700 and ARTEVO 800 (Figure 4). While it can function independently or in conjunction with the Zeiss Veracity Surgical Planner, CALLISTO eye enables a surgeon to plan surgery in the office and display relevant axis and lens alignment information through the oculars on a surgical microscope.
CALLISTO has a built-in eye registration using a patient’s limbal vessels that eliminates the need to manually mark the eye to account for torsion. It also helps guide accurate centration of a capsulorhexis and IOL based on the patient’s visual axis. A meta-analysis from Zhou et al looked at five studies comprising of 257 eyes and found that digital marking outperformed manual marking of toric IOLs in reducing postoperative cylinder errors.2
FEMTOSECOND LASER-ASSISTED CATARACT SURGERY
The revised ASCRS and AAO joint femtosecond laser billing guidelines specify that imaging performed by a femtosecond laser that is necessary to implant a specialty refractive lens can also be considered a form of intraoperative refractive guidance.3 A number of femtosecond lasers are used for cataract surgery, some of which can be connected to refractive guidance systems. For example, Verion can send data directly to the DML on a LenSx femtosecond laser so that the registered image of the patient’s eye can guide the femtosecond laser to mark the cornea with intrastromal corneal cuts to guide the toric IOL placement. Also, the ALLY Adaptive Cataract Treatment System (LENSAR) provides an IntelliAxis Refractive Capsulorhexis system that creates small pointers or capsular marks on the capsular rim during the anterior capsulotomy, reducing any errors due to surgical parallax.
One study suggested femtosecond laser-assisted capsular marking is more precise than digital marking methods described earlier.4 The authors also point out that capsular marking allows for easy evaluation of postoperative toric IOL rotation.
CONCLUSION
All of these intraoperative technologies are reshaping the landscape of cataract surgery, enhancing surgical precision to minimize residual refractive errors and improve UCVA. While there is a need for training and adaptation by surgeons and their teams, I feel most of these devices have a very shallow learning curve.
For ophthalmologists who are looking to incorporate refractive packages into their surgical armamentarium, intraoperative refractive guidance is easy to adopt and provides a layer of security, or confirmation, for lens selection, centration and alignment. By incorporating these technologies, cataract surgeons can not only provide a better service for their patients but also generate additional “safe harbor” income for their practices. OM
REFERENCES
1. Kaufman AR, Pineda R 2nd. Intraoperative aberrometry: an update on applications and outcomes. Curr Opin Ophthalmol. 2023;34:48-57.
2. Zhou F, Jiang W, Lin Z, Li X, Li J, Lin H, Chen W, Wang Q. Comparative meta-analysis of toric intraocular lens alignment accuracy in cataract patients: Image-guided system versus manual marking. J Cataract Refract Surg. 2019; 45:1340-1345.
3. Femtosecond Laser Billing Guidelines. American Society of Cataract and Refractive Surgery (ASCRS). https://ascrs.org/advocacy/regulatory/guidelines/femtosecond-laser-billing. Accessed Feb. 1, 2024
4. Schultz T, Hoffmann S, Dick HB. Comparison of toric intraocular lens alignment between femtosecond laser-assisted capsular marking and digital marking. J Cataract Refract Surg. Published online October 17, 2023.









