One of the most rewarding and impactful decisions I ever made in my practice journey was to embrace premium implant and refractive cataract surgery. The reason I embarked on this journey was twofold: For one, I wanted to address the desire of a number of my patients for a refractive approach to cataract surgery and reduced spectacle dependence. Secondly, and of secondary importance, in this environment of reduced reimbursements, there’s a financial benefit that increases practice health. And when we do something that makes our patients happy and improves practice health, we win on both counts.
Refractive cataract surgery involves any technology and/or surgical maneuver to minimize refractive error, including a standard monofocal implant in combination with intraoperative astigmatic keratotomy or a premium IOL. After a diagnostic and physical eye exam to identify patients who are candidates for premium IOLs, followed by a comprehensive patient education process, approximately 40% of our patients choose refractive cataract surgery and 60% choose a standard monofocal.
I have learned many things along the way that have helped with this growth in refractive cataract surgery, which I share in this article.
FIRST, THE RULING THAT CHANGED EVERYTHING
The CMS rulings of May 3, 2005, and Jan. 22, 2007, bridged the gap between refractive and cataract surgery by both supporting presbyopia and astigmatism correcting implants and the diagnostic and extra work activities that surround them as noncovered services. This was a major step in energizing industry support and advancements in premium implants and the technologies needed for them. The rulings also allowed practitioners to have clear direction on how to handle the billing of patients who desire refractive cataract surgery.
This also meant that all tests and services attributable to the presbyopia- or astigmatism-correcting implants were not covered by Medicare and, therefore, the doctor could charge above and beyond conventional cataract surgery, with the difference paid for by the patient. Finally, it allowed a surgeon who chooses astigmatic keratotomy in combination with a monofocal implant to charge extra for this service.
Making the business of refractive cataract surgery clear was a major step in energizing the growth of refractive cataract surgery in the United States.
CLEAR AND SIMPLE PATIENT EDUCATION
The advancements in presbyopia- and astigmatism-correcting IOLs have been a big reason for the remarkably high level of patient satisfaction that comes with lens replacement surgery. This is because modern-day extended depth of focus and trifocal implants replace both functions a patient’s lens used to perform.
Our IOL options education process has multiple stages, because we know that patients can forget a great deal. So, the more things are repeated, the more likely patients are to remember them accurately and make a well-informed decision. Toward that end, our IOL options education begins with a packet of information that includes a video and links to our website, then conversations with staff and optometrist, all leading up to my discussion with the patient.
When my patients finish this process they understand that in our younger years, our lens has two main functions: to transmit light to help facilitate clear vision and to provide variable focus power to help us focus with clarity at multiple distances (far, intermediate and near). Then, I explain that typically, our lens loses its function of variable focus power first when we reach our 40s, resulting in the need for readers or bifocals. However, we still enjoy good clarity of vision as the presbyopic lens often still transmits light well. Over time, though, it loses its remaining variable focus power and its clarity.
I want patients to understand the two functions of their healthy natural lens during their younger years so they will realize they have a “rest of their life” new lens implant replacement decision to make: an implant that replaces clarity only (and puts the variable focus power in trifocal glasses) or an implant that replaces clarity and reading range (variable focus power at multiple distances and clarity). I go on to explain that what is best for them simply depends on their goals in life.
CLEAR AND SIMPLE FINANCIAL EDUCATION
Doctors are so accustomed to third-party insurance pay in medicine that they are often uncomfortable asking patients for out-of-pocket investment. Be assured that patients want to be educated on all their options, even those that require an out-of-pocket investment, and will make the final decision on whether they want to “invest extra.”
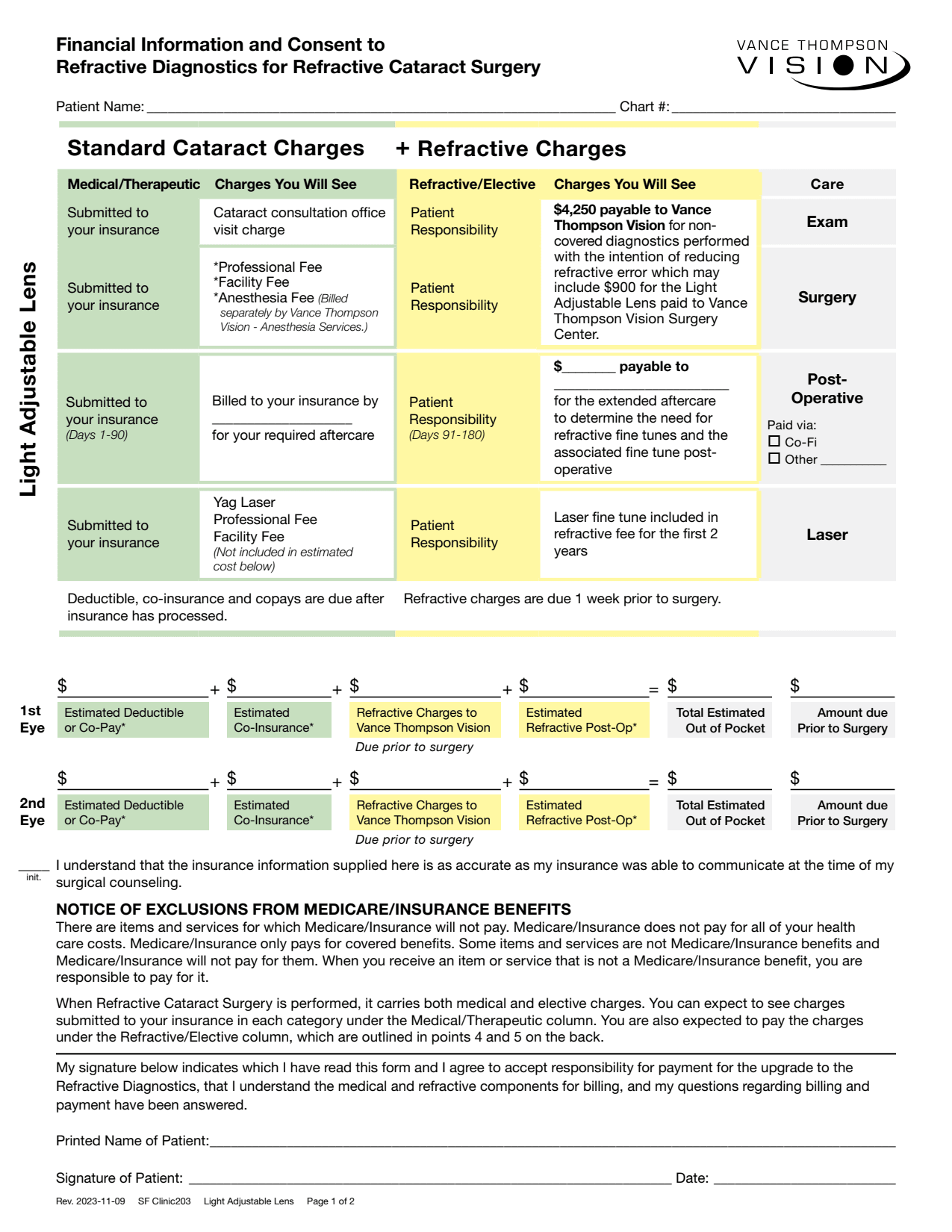
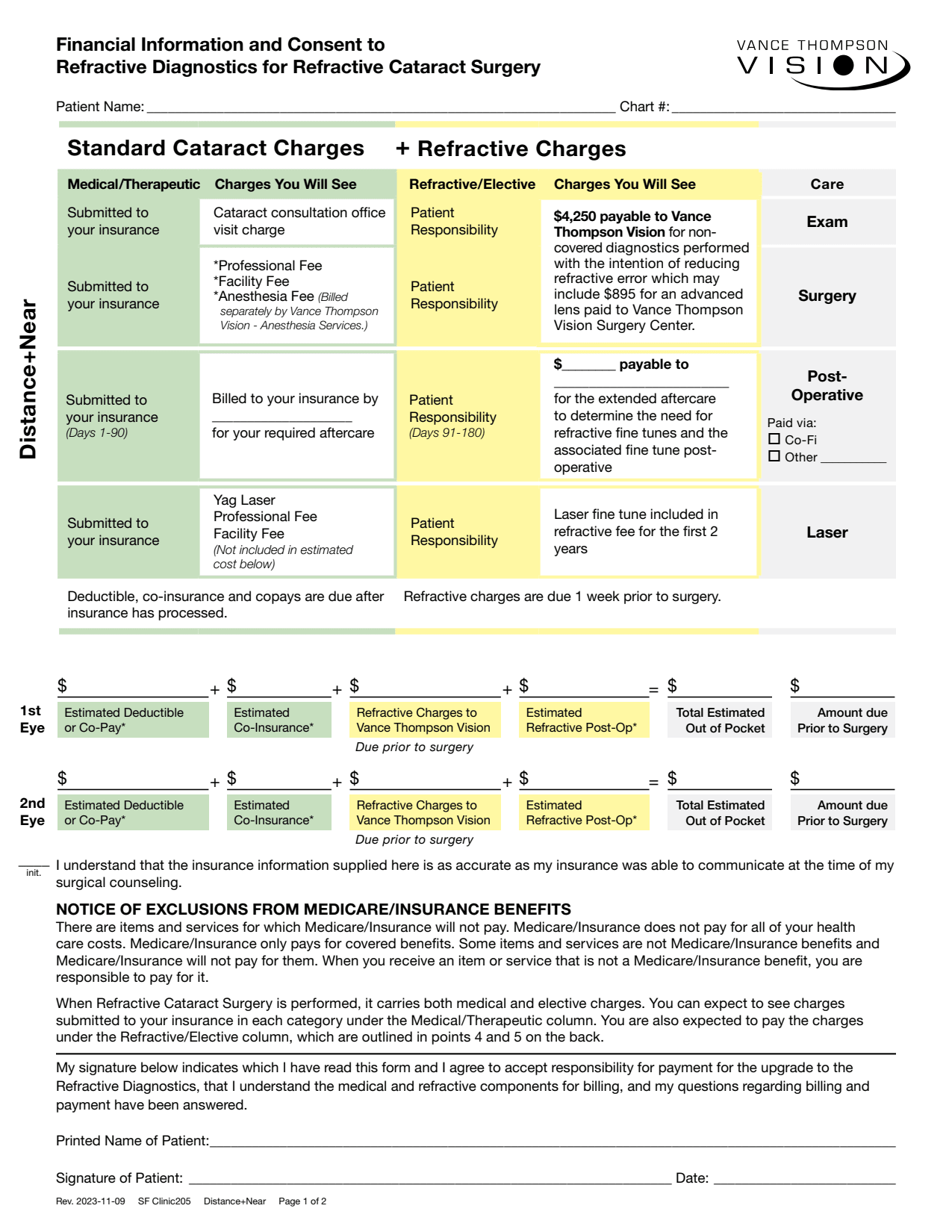
Simple and clear patient education involves simple and clear financial counseling complimented by visual aids (and forms that are read and signed). I like to explain things and have forms that state things “officially.” I tell patients, “Your insurance typically covers replacing the clarity part of the vision you have lost, but it does not pay for managing your astigmatism or replacing the reading range in your IOL. So, you are responsible for the co-pay part of your insurance and the extra investment in treating these aspects of your vision.”
Then, in our forms, we emphasize that Medicare does not pay all the patient’s health-care costs, that only covered benefits are paid by that insurance and that the patient is responsible to pay any remaining costs. We inform them specifically that when cataract surgery is performed with a monofocal implant in combination with astigmatic keratotomy or with a presbyopia- or astigmatism-correcting implant, it carries both medical and elective charges, and that the patient is expected to pay any charges that fall under the refractive/elective category (outlined on our form).
If you wish to see the complete document, see Figure. It is best to tailor your patient education and documents to your practice’s needs. Regardless of the language used, keep in mind that patients appreciate clear and concise financial forms, which help to set pre-surgical expectations and minimize the chance of a misunderstanding.
SETTING YOUR PATIENTS' EXPECTATIONS — AND YOURS
For someone transitioning to refractive cataract surgery, the most important advice I can convey may be to understand the patient’s premium implant journey. I have had the honor of participating in many laser and IOL clinical trials. When I was involved in our country’s first trifocal study, my clinical impression was that neural adaptation was much quicker with trifocal implants than with the generation of bifocal implants I was using. Patient satisfaction was quite good early on, but the highest rate of patient satisfaction was 6 months after surgery. I concluded that, after hitting 20/20 uncorrected with a healthy tear film, there is a period of the patient’s brain adapting to multifocality. In essence, this time period is halo adaptation.
I tell patients, “Any halos you experience after surgery are from the reading part of the implant showing itself around lights at night. This gets better with time as your brain adapts to it.” Some patients cannot adapt to multifocality and need an implant exchange, but this is rare when the patient is educated on the process and the doctor follows through to complete the premium implant optimization.
I tell patients there are basically three important steps to optimizing the image in any cataract surgery: implant, refractive enhancement and YAG laser capsulotomy. In traditional cataract surgery, the refractive enhancement is typically eyeglasses. In premium cataract surgery, however, the refractive enhancement can be eyeglasses — but you and your patient should come to that conclusion preoperatively. While some patients don’t mind eyeglasses, most of my premium implant patients desire spectacle independence, so I work hard on implant calculations.
For those who do not hit 20/20 because of the effective lens position spherical equivalent residual refractive error or incisional astigmatism, I do a laser fine tune, typically LASIK. If their uncorrected vision is not sharp and a manifest refraction doesn’t make it sharp and everything else looks good, I start to look at the capsule as the culprit. This is why I tell patients to expect the three steps — the implant, the YAG and the refractive enhancement — and to consider it a pleasant surprise if they don’t need them all.
I tell patients to remember that, “Once we hit 20/20 and as close to zero correction as possible, your brain needs 3-6 months of adapting and blending the halo. If you go into this understanding the first 3-6 months is spent optimizing your optical system to 20/20 and the second 3-6 months is your brain adapting to your new optical system, you will have some of the world’s most sophisticated optics in your eyes to enjoy for the rest of your life.”
Understanding this process sets their expectation. At follow-up visits, we continue to refer to this preoperative story about optimization and neural adaptation postoperatively.
HAVE A PLAN FOR FRUSTRATED PATIENTS
To minimize frustrated patients, it’s important to keep in touch with patients postoperatively. If we are not doing their after care, we call them at 1 month to check on them and review the journey, and we see them at 3 months to see if they need optimization. Still, frustrated patients will happen, so it is important to prepare your team and yourself for them.
Psychiatrist Elisabeth Kubler Ross taught “There are only two emotions: love and fear …” I try to remember this when I see a frustrated patient. Their vexation is often their way of telling us they are afraid. We need to be patient, do a good exam and explain to them what they are going through. The majority of time, it is not only explainable, but also “showable.”
When I show patients their improved image quality with manifest refraction and remind them about our preoperative discussion on the healing variables and the potential for a fine tune, they are often relieved. If the manifest refraction is not crisp and my exam shows that the capsule is already showing some cloudiness, it relieves them when I remind them about the YAG laser capsulotomy discussion we had preoperatively.
Showing grace and patience to frustrated patients is so important. Clinically, figuring out the source of their frustrations and relieving their anxiety with a calm explanation is one of the most professionally rewarding things I do as a physician and surgeon.
THE OPTIMIZING POWER OF PEOPLE
We are in a new world in cataract surgery thanks to the technological advances of IOLs as well as the diagnostics and surgical tools that compliment them. Even with these advances, we could not make this transition without a great team.
At my practice, I like to say we are very progressive when it comes to technology, and we are very old fashioned when it comes to the people part of what we do. The team who cares for each other will create an environment where the patient feels cared for. To nurture our culture, we have a morning huddle every day that connects virtually all seven of our centers and the people in them. We also celebrate employees, including their birthdays or other special events, and engage in monthly team-building events.
I am so thankful for the team I am a part of, and I credit them with our success. Work on your team experience as you transition from traditional to refractive cataract surgery because they are the ones who will help you get there.
CONCLUSION
Colin Powell said, “A dream doesn’t become a reality through magic; it takes sweat, determination and hard work.” If you put in the work with your people to create a program that includes advancements in refractive cataract surgery and you follow through with the optimization and neural adaptation journey, you will take your practice to the next level and bring improved practice health and joy to your life. OM









