A comparison of cataract surgery reimbursement 40+ years ago vs today reveals how much practice owners need a prudent business strategy.
When my father opened his ophthalmology practice in southern California in 1982, a surgeon in his area could expect to receive around $1,200 per cataract surgery. At that time, Medicare would pay the prevailing rate, using the “usual, customary and reasonable” method, in the area where services were provided. In practice, that meant that cataract surgery payments could vary between $1,000 and $2,200 depending on where the surgery was performed.
That all changed in 1989 when Medicare switched to a resource-based relative value scale (RBRVS) for reimbursement. The goal of this system was to set reimbursement based on the relative costs of providing a service. Each medical service, as defined by Current Procedural Terminology code, was assigned a certain number of Relative Value Units (RVUs). Then, RVUs were assigned a standard dollar value. The net effect of the transition to RBRVS has been a steady decrease in reimbursement levels for cataract surgery, down to the current $585 per surgery in Los Angeles, which equates to a reduction of about 51%.
JUSTIFYING THE REDUCTION IN REIMBURSEMENT
Cataract surgery is the most commonly performed procedure among Medicare beneficiaries, with millions of surgeries performed every year. Through the years, not only has quality improved based on better visual outcomes, faster recovery and better refractive options than ophthalmologists achieved in the ‘80s, but the amount of work per surgery has decreased. Surgeries are faster with fewer postoperative visits. Medicare has used this reduction in work to justify a continuous reduction in payment for cataract surgery.
I don’t think any cataract surgeon would argue this point: it takes most of us less time to perform a surgery now than it did in 2000. Also, the surgeries performed in 2000 were already faster than cases in 1982. However, not many surgeons would argue that 51% less work is involved in the average cataract operation, and that 51% doesn’t take into account the effects of inflation.
WHAT THE DATA SHOWS ON INFLATION
The CMS website shows reimbursement data from 2000-2024, listing Medicare allowable rates in different regions for procedures, including for cataract surgery (66984). Also, the U.S. Bureau of Labor Statistics has annual Consumer Price Index inflation data available with an inflation calculator that allows comparison of the purchasing power of dollars through the years.
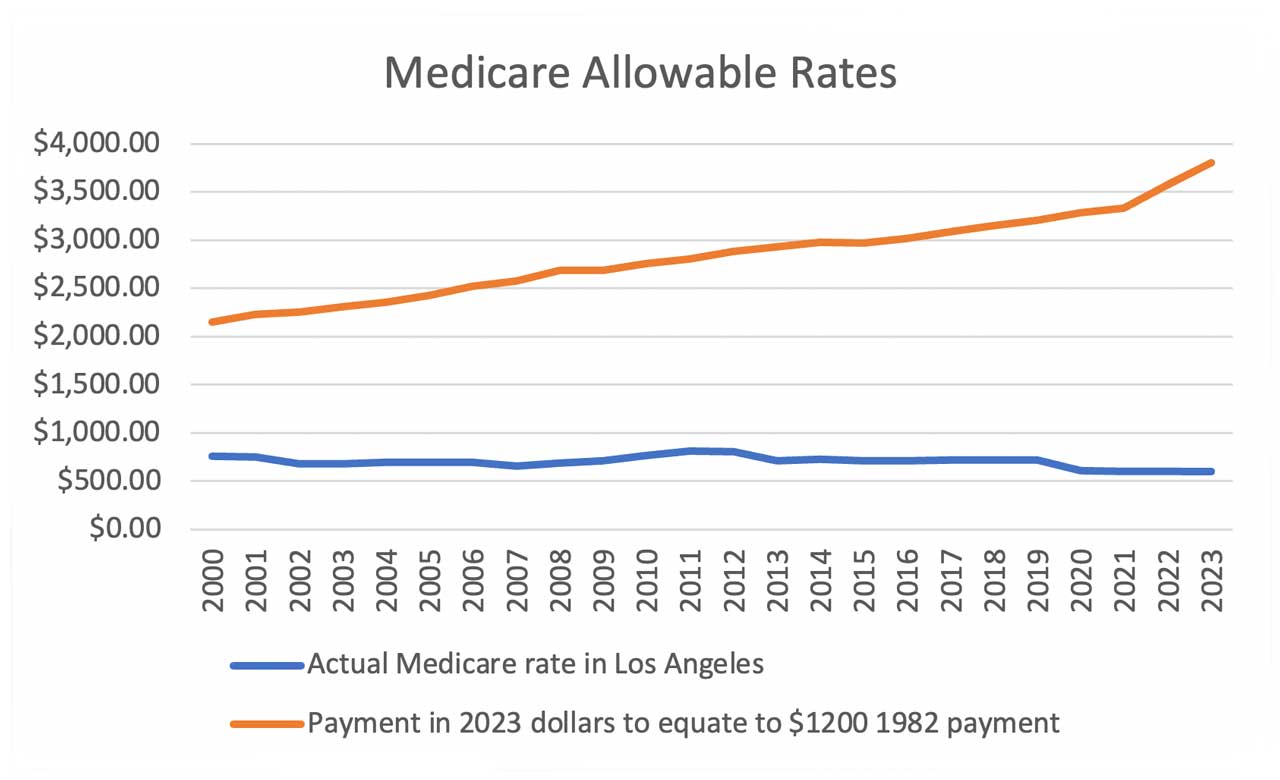
When one looks at current cataract reimbursement rates and compares them to an inflation-adjusted $1,200 payment in 1982, we see a large and growing difference (Figure 1). In 2023, Medicare would have had to allow more than $3,800 per procedure to be on par with a 1982 payment of $1,200. Instead, the 2023 payment was $598. And looking at current payments indexed back to 1982 dollars, that $598 payment would represent the purchasing power of only $189 in 1982.
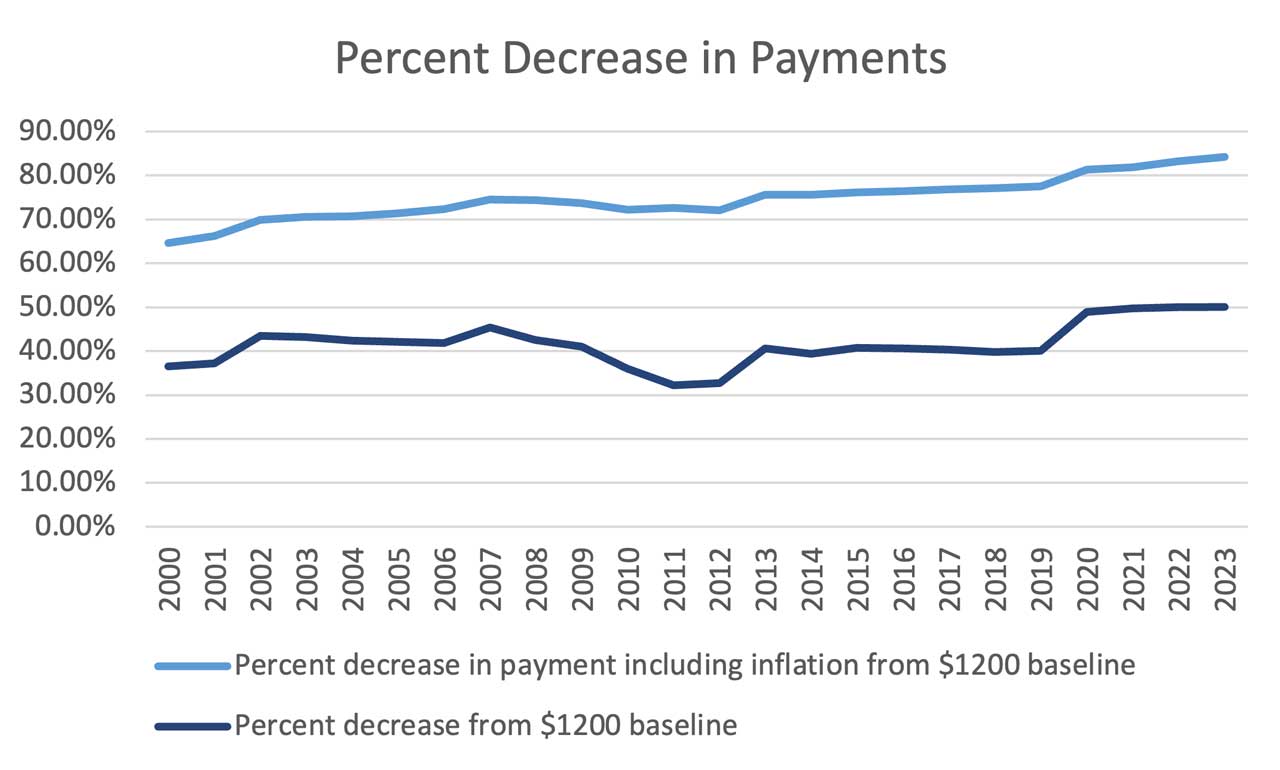
The percent decrease in inflation- adjusted dollars (Figure 2) has been astounding. While payments in the current century have remained stable or slowly downward trending, the inflation adjusted decrease has grown significantly from 65% in 2000 to 84% in 2023.
MAKING THE ECONOMICS WORK
With lower reimbursement rates, ophthalmologists will need to think carefully about how to make these evolving economics work for them. Certainly, most of us have tried to improve efficiency, reduce case time and allow for more surgeries per surgery day, but this can only go so far. No matter how efficient one is as a surgeon, it is not possible to boost productivity by 84%.
Some providers will choose to reduce, instead of increase, the number of surgeries they perform and make up the lost revenue by increasing their volume of office visits. With a return comprehensive eye code paying $139, one would only need to see about four patients in the office to make up for the lost revenue from one cataract surgery. For a surgeon who performs eight or fewer cases per day, this strategy could increase practice revenue.
Additionally, surgeons can offer minimally invasive glaucoma surgery with cataract surgery, which boosts the payment by $137 per case, or add on refractive procedures such as astigmatism management or multifocal lens implantation that can add thousands to case reimbursement.
CONCLUSION
Whatever strategy surgeons pick, with increasing practice costs and declining reimbursement, ophthalmologists will need to pay even more attention to the business of medicine in order to stay in the business of preserving and restoring vision. OM
WHAT’S NEW IN CATARACT AND REFRACTIVE SURGERY
Bausch + Lomb launched SeeNa, a diagnostic system for refractive cataract patients that is fully integrated with its Eyetelligence surgical planning software to help streamline surgical planning and information flow. The company also introduced enVista Aspire monofocal and toric IOLs. enVista Aspire Toric IOLs provide an option for treatment of astigmatism during cataract surgery.
Centricity Vision received 510(k) clearance from the FDA for the ZEPTOLink IOL Positioning System that seamlessly integrates the ZEPTO precision pulse capsulotomy technology with any phaco system to streamline cataract surgery.
Heidelberg Engineering announced FDA clearance of its ANTERION platform that combines biometry, IOL power calculation with corneal topography and tomography, anterior chamber metrics and high-resolution imaging. Patented eye tracking and composite imaging technologies help to deliver sharp image quality.
LENSAR Inc. announced a step forward in its plans to integrate phacoemulsification technology from Oertli Instrumente AG into the ALLY Adaptive Cataract Treatment System. Oertli filed a 510(k) with the FDA for its Faros easyPhaco device, bringing LENSAR closer to delivering combined femto phaco technology.
ZEISS Medical Technology’s VISULAS yag therapeutic laser received 510k clearance by the FDA, expanding offerings within the ZEISS Cataract Workflow. It provides a precise and compact laser workstation for safe and effective posterior capsulotomy and iridotomy procedures.
Lupin Limited received FDA approval for its abbreviated NDA for bromfenac ophthalmic solution, 0.07%, to market a generic equivalent of Prolensa ophthalmic solution, 0.07% (Bausch + Lomb).Lupin also received FDA approval for its abbreviated NDA for bromfenac ophthalmic solution, 0.09%, a generic equivalent of Bromday ophthalmic solution, 0.09% (Bausch + Lomb).
IN THE NEWS
Meridian Medical received FDA approval for the MR Q family of lasers. The MR Q is a fully integrated Nd:YAG laser combined with a precision optics LED slit lamp; the MR Q SLT is an Nd:YAG laser combined with a selective laser trabeculoplasty photo-regenerator; and the MR Q supine is an Nd:YAG laser that treats patients in supine position.
The iDose TR from Glaukos Corp. is now commercially available. It uses VitalDose EVA from Celanese Corp. to provide sustained drug release for the treatment of glaucoma. iDose TR is a long-duration, intracameral procedural pharmaceutical therapy designed to continuously deliver 24/7 therapeutic levels of travoprost.
CorNeat Vision introduced the CorNeat EverPatch synthetic tissue substitute for ocular surface surgeries. Its novel structure enables seamless integration with surrounding tissue without triggering a chronic foreign body response, and its non-degradability permanently reinforces the ocular surface.
Ikerian AG and RetinAI Inc. US launched RetinAI Discovery for Clinics, with two product versions to address the needs of ophthalmologists and optometrists. Discovery for Clinics and its AI models are designed to accelerate and enhance clinical decision workflows, teleophthalmology management, referral decisions and patient management.
The FDA granted Breakthrough Device Designation to SightGlass Vision’s Diffusion Optics Technology spectacle lenses, which are intended to slow myopia progression in children. It uses a contrast management mechanism of action, incorporating thousands of elements that gently scatter light across the retina.
Patient payments with CareCredit, a Synchrony solution, can now be processed through CoFi Inc.’s multi-party payments platform. Patients can finance the entire cost of a procedure with CareCredit — including the surgeon’s fees and those of their surgical partners, such as the ASC and/or co-managing provider — through the surgeon’s office.









