TAKE-HOME POINTS
- Stay aware of the needs of your patients and the limitations of your current surgical therapies — ie, does it solve a current problem?
- Know (and state) your why. Evaluate new technologies based on your core values.
- Learn and anticipate as much as possible — ie, go beyond the sales pitch and learn the technology.
- Solicit ideas from your team on the logistics of implementing the new technology.
- Involve your patients and give them realistic expectations — ie, don’t hide the fact that it’s new.
- Know when to scale up or when to bail out — start slow. You’ll know soon enough if the technology is worth the hype.
How does a premium practice ophthalmologist safely and effectively integrate new procedures, technologies and staff, particularly in a refractive practice that emphasizes high levels of patient service and expectations? Cataract and refractive surgery practices are often distinguished by their adoption of new technology and leadership in the field; however, they are also relied upon for consistently superior outcomes, which are achieved by performing consistent procedures using trusted technology. Therefore, how does one overcome this dichotomy: achieving both machine-like precision and repeatable outcomes while also avoiding the stagnation of repeating the same thing year after year? Even more, how can a premium practice integrate new staff and doctors, and not lose what made the practice premium in the first place?
Technology is a key factor to our outcomes. Most of us have our “tried and true” technologies that we have carefully optimized, but we also know that there is a continual stream of new technology coming to market that may have the potential to improve outcomes and drive practice growth even further.
When many of us first graduate from training, we are excited to adopt all of the new advancements in ophthalmology. Eager for progress, we can sometimes fall for “new lens euphoria,” and “new tech euphoria.” After a few years of experience, we realize that while new may be necessary, it is not always better and that we need an objective way to evaluate new technology. At ClearSight and 43Vision, we developed a system to do so. Below, we’ll discuss how to evaluate and add new technology and doctors, along with a few questions to consider.
HOW TO EVALUATE AND ADD NEW TECHNOLOGY
Does it solve a current problem?
One must evaluate a new procedure or technology’s potential to add value to the practice. Whether it is to streamline processes (eg, new EMR, new patient survey systems), expand the range of eligible patients (eg, adjustable IOLs, implantable collamer lens) or to provide incremental improvements in therapies (eg, topography-guided LASIK), there must be a perceived value in integrating the new technology to the practice. If the technology can’t add significant value, it’s okay to pass. There’s always more to come!
At ClearSight and 43Vision, our moderate-to-high myope patients, especially those over 40 years old, have been a challenge to please. While nailing crisp distance vision in myopes is quite rewarding, the near vision expectations are more challenging to meet. In this patient population, we have been more conservative in our approach, often using blended vision with LASIK or monofocal IOLs rather than multifocal IOLs. According to a 2016 study published in the Journal of Refractive Surgery, “Theoretical effect of lens position and corneal curvature on the near focal point of multifocal intraocular lenses,” by McKee and Jhanji, the effectiveness of multifocal IOLs at near may decrease with the large anterior chamber depths common in myopes. However, with the advent of newer lenses, it is still a challenge, but we are more consistently able to meet these patients’ high expectations.
Know your why
When you opened or joined your new practice, you had a “why” driving you forward, consisting of your ultimate goals, your values and what you envisioned for the practice. This “why” is what ultimately makes your practice a reflection of you. As business expert and The New York Times best-selling author Simon Sinek says in “Start With Why,” “People don’t buy what you do; they buy why you do it and what you do simply proves what you believe.” Not only is it important to ask if a new tech, staff or company direction is profitable, but it is crucial to examine them in the context of your why. Discuss knowing who you are and asking if your new plan meets your values and practice style.
Acquire as much knowledge as possible
When a procedure or instrument is novel, it is crucial to build a knowledge base as soon as possible. Aggregating practice data over two, three or even several practices can expedite the learning process. When feasible, leverage colleagues’ experiences to jumpstart the implementation of new technology. It may be necessary to observe surgical procedures at other offices, receive training under another physician or even share surgical videos to gain valuable insights. When visiting an office, involve your practice administrator to learn about the operational aspects, which will aid in understanding the challenges of implementation. Potential challenges should be anticipated and addressed as comprehensively as possible.
Over the past few years, knowledge from colleagues has helped us both avoid and seek out new procedures. When the Raindrop inlay (Revision Optics) was approved, a trusted colleague told us there was a risk of haze. We started slowly as a result and were happy to place only 10 inlays. Alternatively, when we decided to expand our SMILE procedure to most of our laser vision correction (LVC) patients, we modified our surgical technique and nomogram after observing the technique of an established practice. This allowed us to proceed more safely and confidently during the growth period.

Obtain staff buy-in
One must recruit staff involvement in the new technology. Using visionary leadership, explain to your staff its value. Understanding the “why” behind the work will alleviate any initial turbulence. Whether it’s a streamlined process for clinic techs, happier post-op patients or telling more patients “Yes, you are a candidate,” the “why” might be slightly different for each department.
Also, solicit team ideas on the logistics of implementing the new technology. For example, your clinic director and lead techs may see potential roadblocks or opportunities to make a smoother transition.
Establish a clear plan and maintain open lines of communication, both upward and downward in the chain of command. A willingness to be open, acknowledge shortcomings in new technology and knowing when to pivot will facilitate its successful adoption.
Patient involvement and expectations
Now that you have obtained staff buy-in, your staff and physicians will be instrumental in the communication around the new technology. Maximize patient engagement by actively involving them in the excitement. Physicians should clearly communicate the advantages and benefits that the new procedure offers, emphasizing how it specifically caters to their needs. This information should be conveyed to patients transparently and without hesitation! Give realistic expectations to the patients. This can be explained to them verbally in the office by physicians, on the phone with counselors, the clinic techs, etc.
Whether the procedure will require additional follow-ups, a higher chance of enhancement or other foreseeable compromises, you must clearly state these to the patient. If you have surgical counselors, they will be instrumental in communicating expectations for follow-up appointments. For example, in implementing the Light Adjustable Lens (LAL, RxSight), one must describe the “journey” from surgery to final outcome. Additionally, if there is uncertainty in the final outcome, this should be shared with the patient as part of the informed consent process.
Know when to scale up, scale down or to stop
Regardless of whether a procedure exceeds expectations or falls short, one should not shy away from or feel personally validated or invalidated due to the outcome.
For example, when the LAL was added at ClearSight and 43Vision, it was adopted very quickly and broadly and in a wide context of lenses and patients to include bilateral LALs and mixed with advanced-technology IOLs in both post-refractive and virgin eyes. Scaling quickly allowed for rapid learning. However, we also realized where the technology excelled and where modifications could be made. Had we started a little more slowly, we might have had more time to determine our nomogram.
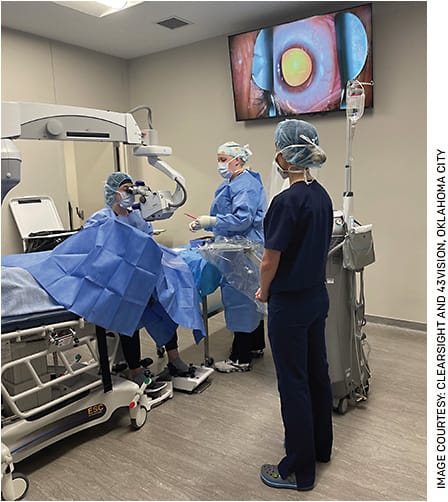
Implementation of this technology also involved broad communication amongst support staff given the frequent follow-up appointments. Staff buy-in was swift, and this allowed our office to become proficient in this technology within a few short months.
TEACHING AND LEARNING FROM MDS IN PRACTICE
When we onboard new doctors and fellows, we train heavily (and even have a consultant) on communication with patients and staff. We strive for cohesion among our staff as this improves the patient experience. The right new doctor, surgeon or fellow is open to constructive criticism and early feedback.
Not only do we need cohesion in the clinic, but we also need cohesion in the operating room, as our surgeons aim to be as interchangeable as possible. Safety is of utmost concern, especially as fellows or surgeons learn new procedures.
In our refractive surgery fellowship, we proceed with the simplest LVC procedures first and use wet lab training and shadowing, followed by slow introduction of hands-on procedures. We allow for increased per-procedure time early on and add more volume as the fellow becomes proficient. We use full supervision and review recorded surgical videos. Each fellow proceeds as his or her skills allow to have the basic foundation of all our surgeries within a few months.
As transparency is important for trust, we include an optional fellow consent for all surgical procedures. Fellows only participate in surgeries for which there is a completed fellow consent. Similar to fellow training, if a surgeon who is added to the practice needs additional refractive surgery training, we add a separate consent and supervision.
A GREAT PRACTICE IS WORTH FIGHTING FOR
It takes deliberate and continual effort to add new technologies and procedures, all while maintaining a premium ophthalmology practice. Though this goal is ambitious, the right staff will be energized by the addition of new adventures and challenges. In fact, this will keep things fresh and help employees feel a sense of ownership and responsibility as the company and employees grow together.
As new procedures and technologies are added, accomplishments should be celebrated and the wins tied back to your company’s “why.” Update your employees on the successes: the efficiencies created, the new patients treated, the happy patients. All employees have the opportunity to assist with the integration of these processes and experience professional growth and fulfillment. And, with a premium practice with satisfied patients and staff, your satisfaction will grow immensely. OM










