As ophthalmologists dedicated to thoroughly and effectively supporting our patients, a crucial part of pursuing our mission is finding creative ways to resolve obstacles that face our practices. For many of us in this post-pandemic time, that balancing act includes struggling to overcome staffing shortages, paying higher salaries to keep pace with inflation and absorbing Medicare’s reimbursement cuts for the surgeries we routinely conduct.
While those conditions might seem stark, a number of strategies can help us streamline our efforts so that we never lose ground when it comes to providing top-notch care.
At the Eye Centers of Racine & Kenosha, we’ve implemented a series of measures designed to save time not only for our administrators but also for our doctors, who are now able to give their attention to more patients each day. A key strategy has been to safely eliminate a single topical eye medication from the regimens we typically prescribe for patients with glaucoma or cataracts (for more, see page 14).
A SAFE AND EFFECTIVE TRADE-OFF
Surgical options
But how can we restrict the number of eyedrops we use without sacrificing patient outcomes? We rely on several modern technologies, starting with specialized outpatient procedures for patients with glaucoma or cataracts that both control eye pressure and limit the incidence of dry eye, resulting in a reduced need for drops.
Evidence shows that minimally invasive glaucoma surgery (MIGS), selective laser trabeculoplasty (SLT) and even the less invasive bleb surgery can help reduce the drop burden for these patients. For instance, in the LiGHT trial,1 SLT provided predominantly drop-free treatment that matched the effectiveness of drop therapy in controlling eye pressure while providing better long-term disease control, with patients experiencing a reduced need for incisional glaucoma and cataract surgery over 6 years. Meanwhile, a separate trial that evaluated iStent (Glaukos)2 found that more patients who received a stent along with cataract surgery remained medication-free after the procedure compared with patients who received cataract surgery alone. Those who received the stent also reported more quality-of-life improvement than those who had cataract surgery alone.
Sustained-release medications
Ophthalmologists can also help keep patients off drops and assure adherence by administering treatments that release topical medication into the eye over the course of months.
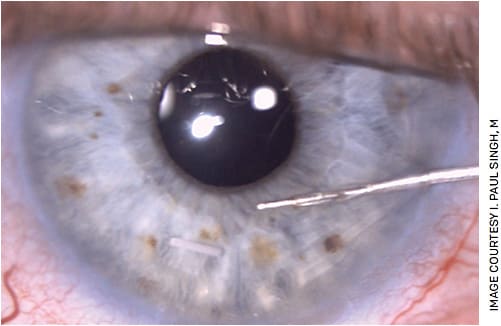
For instance, Durysta (Allergan) is an intracameral implant that treats glaucoma by releasing bimatoprost 24 hours a day for 4 months, with efficacy lasting up to 2 years in select patients (Figure 1).
Another sustained release medication, DEXTENZA (Ocular Therapeutix), is a resorbable insert used when patients need steroids after undergoing procedures for cataracts, glaucoma or other eye conditions. This 0.4-mg intracanalicular insert dispenses preservative-free dexamethasone for a month at a time to help control inflammation and pain following ophthalmic surgery (Figure 2). This product, which can be intuitively placed into the tear duct by any eye-care provider (ECP) in the office or at the time of surgery, is an excellent way to avoid the kind of noncompliance that can lead to post-surgical inflammation, dry eye and even cystoid macular edema.

Additionally, compounding pharmacies, such as OSRX and Imprimis, can combine a steroid, an antibiotic and an NSAID into a single preservative-free solution, which makes compliance easier for patients.
The time savings
By cutting just one bottle of drops, we can minimize the time our teams spend seeking prior authorizations, giving patients instructions, fielding follow-up questions about regimens and verifying medication lists during appointments.
In an informal study, our practice found that eliminating a single post-operative eyedrop prescription in patients with glaucoma saved 4 minutes at each visit. Cutting two drops from the regimens used by those patients gave us back 5.5 to 6 minutes per visit.
A larger survey3 confirmed an average savings of 41.4 staff hours per week by 19 U.S. cataract surgery practices that postoperatively treated patients with DEXTENZA compared with the amount of time they would have spent administering their usual standard of care. In that survey, staff recalled spending 45% less time per patient on postoperative eyedrop counseling and 46% less time per patient on pharmacy calls after inserting DEXTENZA and switching the survey subjects from a three-drop to a two-drop regimen.
With resources stretched thin for practitioners in our field, thoughtfully restricting drop regimens should be a go-to strategy for big and small ECPs alike, as it can help us stay focused on the tasks that add the most value to our practices.
IMPROVING PATIENT QUALITY OF LIFE
Limiting eyedrop prescriptions does more than help us streamline our businesses: It also increases satisfaction for our patients. We have good evidence from studies, including the iStent Inject Phase 3 trial, that quality of life improves when patients can decrease their drop burden.
I’ve seen many individuals who had glaucoma or cataracts struggle with compliance when faced with a large drop burden, whether due to the price tags of drugs, uncertainty about regimens, tolerability issues or frustration with trying to remember to take the medications.
In fact, in an unpublished survey, our practice polled satisfied patients 90 days after surgery and learned that they perceived ongoing eyedrop use as the most difficult part of their treatment process.
Unfortunately, as ECPs, we sometimes inadvertently add to this burden by prescribing solutions preserved with chemicals that can stimulate dry eye, an uncomfortable condition that often necessitates the prescription of even more drops. That dynamic has certainly proven problematic for patients with glaucoma, as research4 shows that their risk of dry eye, and thus of non-adherence, rises with the use of topical medications preserved with chemicals such as benzalkonium chloride. To make matters worse, researchers have found5 a nearly 30% reduction in compliance with topical glaucoma medications in patients who have signs or symptoms of ocular surface disease.
By using the above options to intervene in that vicious cycle, we have markedly reduced the number of complaints we receive about convoluted eyedrop regimens and dry-eye symptoms such as tearing, burning and pain. I’m pleased to note that this has helped us engender both trust and compliance among our patients as well.
EXPLORING ADDITIONAL TIME-SAVING STRATEGIES
In addition to finding ways to safely restrict eyedrop regimens, our practice has generated significant time savings through a host of other techniques. Here are some examples:
- To help ease gaps when qualified staffing candidates are difficult to find, we regularly turn to Alchemy Vision. This company offers affordable video-based curriculum that can teach people with no experience in ophthalmology or eye care to work up patients, understand technologies and start to become familiar with the “language” of our field.
- We’ve also had success training new staff members as designated diagnostic testing technicians, an easy process that facilitates flow and efficiency in our practice. Later, as time allows, we have the option of providing additional instruction to make these technicians more versatile so that they can provide full work-ups.
- I’m never without a scribe who understands my process and can educate my patients about issues such as medication and at-home care regimens after I’m done with an exam. This allows me to move on to the next exam room sooner and to focus on my patients during appointments, rather than on a screen.
- Zeiss’s Forum supports medical decision-making by integrating visual fields such as optimal coherence tomography, fundus photographs and IOP findings with a patient’s EMR to create a snapshot of all test results. Another Zeiss software product, Veracity, allows me to plan cataract surgery from anywhere, with all diagnostics simultaneously available for review.
- Telemedicine enables me to triage patients who are experiencing eye problems or seeking surgical follow-ups. Determining which individuals need to be seen immediately and who can wait is a good way to streamline in-office scheduling.
- Partnering with medical optometrists, who can step in to co-manage cases, saves me time while maintaining excellent patient care.
- Newer diagnostic technologies allow us to quickly appreciate the quality of the eye’s entire optical system. One example is iTrace (Tracey Technologies), a powerful tool that provides information on higher-order aberrations of the cornea and vitreous fluid, as well as angle Alpha and angle Kappa measurements. More importantly, with this tool’s dysfunctional lens index screen, we can efficiently educate patients on the value of treating astigmatism.
- In our in-office surgical suite at the Eye Centers of Racine & Kenosha, we can add on cases as needed to quickly resolve issues such as complications from glaucoma surgeries without needing to find a time slot at an ASC.
TAKE YOUR TIME
Envisioning the positive results of time-saving measures can be enticing, and it may be tempting to implement a series of them in short order. However, I urge my fellow practitioners to move slowly, incorporating one change at a time and measuring its effectiveness and benefit to patients before adopting any more.
Moving forward carefully and deliberately empowers staff members to get acquainted with novel ideas, strategically incorporate them into the flow of the practice and, ultimately, champion them to help ensure their success. OM
REFERENCES
- Gazzard G, Konstantakopoulou E, Garway-Heath D, et al. Laser in Glaucoma and Ocular Hypertension Trial: Six-Year Results of Primary Selective Laser Trabeculoplasty versus Eyedrops for the Treatment of Glaucoma and Ocular Hypertension. ScienceDirect. 2022 Sep 17. (Epub ahead of print).
- Glaukos.com . Pivotal Trial Results for Glaukos’ iStent inject Published in Leading Ophthalmic Journal. Published March 15, 2019. https://investors.glaukos.com/investors/news/news-details/2019/Pivotal-Trial-Results-for-Glaukos-iStent-inject-Published-in-Leading-Ophthalmic-Journal/default.aspx . Accessed Jan. 3, 2023.
- Nijm L, et al. Real-World Evidence of an Intracanalicular Dexamethasone Insert Saving Time on Patient Education and Calls for Post-Cataract Surgery Care. Presented at the American Academy of Ophthalmology Annual Meeting; November 12-15, 2021; New Orleans, Louisiana.
- Baudouin C. Detrimental effect of preservatives in eyedrops: implications for the treatment of glaucoma. Acta Ophthalmol. 2008;86:716-726.
- Stringham J, Ashkenazy N, Galor A, Wellik S. Barriers to Glaucoma Medication Compliance Among Veterans: Dry Eye Symptoms and Anxiety Disorders. Eye Contact Lens. 2018;44:50-54.









