Direct-to-consumer genetic testing services have become increasingly popular. One industry leader, 23andMe, boasts of 12 million customers worldwide.1 Individuals who order genetic testing services can select from a menu of genetic data, including ancestry, various traits, health predisposition and carrier status reports. The health predisposition reports genetic susceptibility for a variety of complex multifactorial health conditions that are the result of gene-environment interactions, such as anxiety, restless leg syndrome, atrial fibrillation — and even glaucoma.
As individuals have more access to their own genetic data and interpretations of its implications, understanding genetic predisposition to glaucoma has become increasingly clinically relevant. In this article, we will discuss what is known and not known about the role of genetics in the etiology of glaucoma and offer advice on working with patients who come to clinic with the results of genetic testing services.
HERITABILITY OF GLAUCOMA
Heritability is defined as the proportion of overall variation in a population that is attributable to genetic variation. Glaucoma has an estimated heritability of 70% and is one of the most heritable of all complex human diseases.2 Glaucoma that develops during childhood can be inherited as autosomal dominant or autosomal recessive traits due to a single gene mutation, while adult-onset forms of glaucoma typically exhibit complex inheritance due to contributions of multiple genetic and environmental risk factors.
The two primary types of adult-onset glaucoma, primary angle-closure glaucoma (PACG) and primary open-angle glaucoma (POAG), are known to be highly heritable. For example, siblings of individuals with angle closure have 13.6 times greater odds of angle closure, compared to normal siblings.3
Recent multiethnic genome-wide association studies (GWAS) have identified eight independent loci associated with PACG risk, including those in PLEKHA7, COL11A1 and PCMTD1–ST18 genes.4,5 Similarly, to date, 127 independent common risk variants for POAG have been identified in multiethnic populations. These risk variants are found in genomic regions that include genes such as SVEP1, RERE, VCAM1, ZNF638, CLIC5, SLC2A12, YAP1, MXRA5 and SMAD6.6 Some early-onset glaucoma genes may also contribute to adult onset disease. For example, MYOC (myocilin) mutations frequently cause severe juvenile open-angle glaucoma in children. However, one MYOC mutation, the p.Glnn368Ter variant, has been found in 2-7% of POAG patients.7-9
RISK SCORES
Genetic vs polygenic
For complex diseases such as glaucoma with numerous potential genetic contributors to disease phenotype, genetic and polygenic risk scores can be used to measure the cumulative contribution of multiple risk variants to provide an aggregate measure of an individual’s overall genetic risk for a given disease.
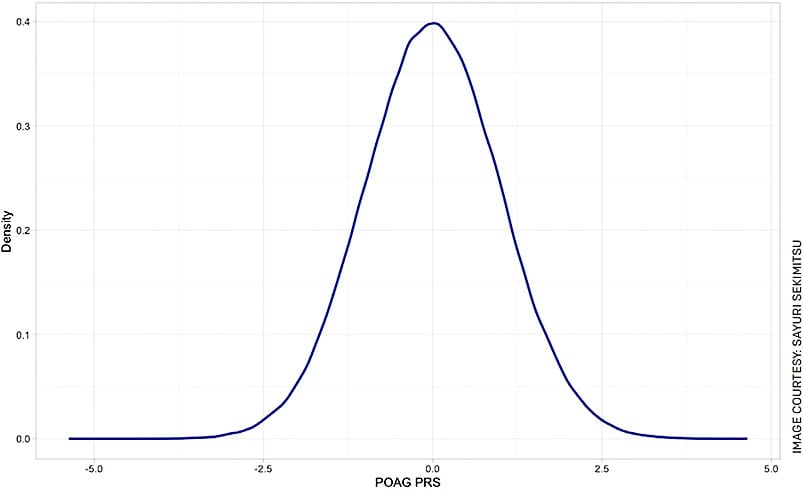
To calculate a genetic risk score, known genetic variants associated with a given disease are combined into a cumulative risk score. The variants that are included in the polygenic risk score are discovered through GWAS, where genomes of individuals with and without a disease are compared; variants found more frequently in individuals with a disease are identified and assigned a weight based on association with disease. Polygenic risk scores are calculated by identifying the collection of variants each individual’s genome contains and constructing a cumulative scores adjusted for the weight of each variant’s impact on disease risk (Figure 1).
Unlike genetic risk scores that sum the cumulative risk from variants that meet genome-wide significance, a polygenic risk score sums cumulative risk from all variants. While an individual variant may not individually statistically increase risk of disease, the sum of thousands of small risk-increasing variants may increase risk of disease significantly, making a polygenic risk score more comprehensive than its genetic risk score counterpart. It is important to note, however, that polygenic risk scores provide relative risk of a disease; it can identify individuals who are at higher risk for a disease compared to the general non-diseased population but does not confer absolute risk. This is in comparison to a BRCA1 mutation, for whom individuals who carry the mutation have a 60-80% risk of breast cancer.10
Interest in calculating polygenic risk scores for glaucoma has been growing amongst the scientific community. Indeed, the PubMed results for “polygenic risk” and “glaucoma” have increased significantly in the last 4 years, from zero papers published in 2018 to 15 papers published in 2022 alone, likely due to increased availability of large-scale human genomic data, such as the U.K. Biobank.
Prior work has demonstrated the utility of glaucoma-specific genetic and polygenic risk. For PACG, a genetic risk score was calculated using eight known genetic variants; after adjusting for age and sex, individuals in the highest quartile of PACG genetic risk were found to be seven times more likely to have PACG compared to individuals in the lowest quartile of risk.11 Similarly, a higher PACG polygenic risk score was found to be an independent predictor of PACG in a multiethnic cohort; a one standard deviation increase in PACG polygenic risk score was associated with a 1.3 times higher odds of PACG, after controlling for age, sex and ancestry.12
The same PACG polygenic risk score is associated with higher IOP and more hyperopic refractive error, both markers for potentially more severe disease. Finally, individuals with higher PACG polygenic risk scores had a higher PACG prevalence at a younger age, indicating an association with earlier disease presentation.
Prevalence and severity
Similarly, prior work demonstrates that a higher POAG genetic and polygenic risk score is associated with POAG prevalence and disease severity.
Specifically, a POAG genetic risk score is associated with earlier age of diagnosis with the top 5% of POAG genetic risk having a mean diagnosis 5.2 years before those in the bottom 5% of risk.13 In our latest work, we found the prevalence of POAG in the highest decile of polygenic risk was more than five times the prevalence of POAG in the lowest decile of polygenic risk. After adjusting for age and sex, one standard deviation increase in POAG polygenic risk score was associated with 1.72 times higher odds of POAG.
Importantly, we found glaucoma medication and surgery/laser use increased with greater POAG genetic burden, suggesting more severe disease; medication and surgery/laser use in the highest decile of genetic risk was almost 10 and six times that of those in the lowest decile of genetic risk, respectively. Individuals with higher polygenic risk scores were also more likely to have disc hemorrhages and optic nerve notching/rim thinning on fundus photography.
Finally, we have also found associations between increased polygenic risk and thinning of retinal nerve fiber layer and ganglion cell complex, as measured by optical coherence tomography. Other researchers have also found that higher POAG polygenic risk is associated with more rapid visual field worsening and peripapillary retinal nerve fiber layer thinning over a 5-year period.14
The body of work to date clearly shows that genetic and polygenic risk scores are independent predictors of both POAG and PACG, and are associated with more severe disease and earlier diagnosis, underscoring the large role of genetics to glaucoma predisposition.
Pitfalls of risk scores in glaucoma
Despite promising advances in our understanding of genetic predisposition to glaucoma, several limitations remain regarding genetic and polygenic risk scores.15
While genetic and polygenic risk scores provide information about relative risk (eg, “one standard deviation above average risk”), they do not necessarily translate to absolute risk (eg, “30% lifetime risk”). These risk scores, therefore, do not answer the question that most patients might want to know: “How likely is it that I will develop glaucoma during my lifetime?” Furthermore, relative risk depends on the population from which they are calculated; one may be in the top 1% risk in one cohort but in the top 20% risk in another cohort, which makes interpretation of scores more challenging. We also know that while polygenic risk confers greater risk of glaucoma, not all individuals with high genetic burden have or will develop glaucoma. Similarly, individuals with low genetic burden have been shown to have disease, albeit at a lower rate. Why one individual with high-risk burden has glaucoma and why another does not is still not well understood.
Another significant limitation of genetic and polygenic risk scores is their limited translatability from a cohort of participants in a research study to the general population. Calculation of risk scores often relies on large GWAS, the majority of which are performed on predominantly White/European ancestry populations, despite known differences between different ancestries and associations between glaucoma and genetic variants.16 As a result, risk scores that may predict glaucoma accurately in one population may perform poorly in another. This is an important issue, and there is a growing push in the genomics field towards use of multiethnic data. However, the majority of genetic data currently used in the creation of risk scores are derived from individuals of European ancestry.
WALKING THROUGH ONE EXAMPLE
23andMe methodology
The popularity of direct-to-consumer genetic testing has provided patients with a significant trove of personal genetic data that they may not know how to interpret and apply to their own lives. With the purchase of a 23andMe kit, an individual can identify their predisposition to many conditions, including glaucoma (Figure 2).

Recently, 23andMe started offering a calculated health predisposition via a polygenic risk score, explaining to consumers that “this report is based on a statistical model that takes into account your genetic results at more than 8,000 genetic markers.” A customer may receive a result that states “X% of people with genetics and other factors like yours develop glaucoma by their 80s.”
23andMe published a white paper detailing the methodology behind their polygenic risk score calculation and how it translates to estimated likelihoods.17,18 In short, the estimated genetic relative risk for each polygenic risk score percentile is multiplied by baseline glaucoma prevalence per ancestry for individuals in their 80s. This is simply an effort to correct for differences due to ancestry prevalence. The prediction of age of onset and severity is still based on published work that mostly does not include populations other than European Whites populations.
Limitations
While 23andMe provides an opportunity for patients to better understand how their genome may cause predilection for certain diseases, their methodology has some limitations. Though 23andMe utilized ancestry-specific cohorts to calculate their risk scores, the predictive power of glaucoma polygenic risk score varies across different ancestral backgrounds. It is possible this variation is due, in part, to self-report of disease status (eg, they identify individuals with glaucoma through self-report for “glaucoma or possible glaucoma”) instead of specifying the specific subtype (eg, POAG vs PACG). Self-reported data often suffers from inaccuracy, thus increasing possible false positives and false negatives introduced to the dataset.
Finally, their baseline prevalence of individuals with glaucoma in their 80s is based on a limited sample size for some ancestries; while they had a sample size of 50,781 and 49,975 for women and men of European ancestry in their 80s, respectively, their sample of South Asian women and men in their 80s consisted of only 110 and 230 individuals, respectively.
OUR ADVICE
Throughout the past decade, our understanding of genetic predisposition to glaucoma has grown and our evidence base for glaucoma pathogenesis and genetics has improved. As direct-to-consumer genetic testing grows more popular, the understanding of the genetics underpinning of glaucoma becomes more clinically relevant. Patients may come to our clinics with their 23andMe results at hand, and it will be our job to contextualize these results. For example, we can explain to our patients that genetic risk scores indicate their risk of disease compared to the study population. It is important to stress that while genetic risk scores can estimate risk of disease, this is a developing field of research and has not been validated broadly. Additionally, we can explain that elevated genetic risk score is another data point, similar to family history and central corneal thickness, which can help us better understand the patient’s risk of disease and possible worsening. While genetic and polygenic risk scores can be useful to risk-stratify patients, more research must be done to validate findings of polygenic risk scores more broadly before using it as the basis to change clinical management.
In the future, we envision using polygenic risk scores allowing for more individualized care of patients with the potential to identify patients most likely to develop disease and progress to vision loss. For now, if a patient presented with a high polygenic risk score for glaucoma, screening is certainly warranted. If the patient additionally had phenotypic evidence of glaucoma, we may be inclined to follow them more frequently and treat more aggressively. On the other hand, patients may present with a low polygenic risk score but clinically evident glaucoma.
While environmental, nutritional and systemic factors may certainly contribute to disease in such patients, it is also important to stress that rare genetic variants are not included in polygenic risk scores and that these scores are mostly driven by IOP and, thus, may not apply in every setting. Future research will provide additional insight and improve polygenic risk score predictive power. Additionally, patients who present with high polygenic risk score and a normal exam may be best served by explaining what we know about the influence of genetics in glaucoma and continuing to encourage regular vision screening. OM
REFERENCES
- 23andMe. 23andMe for Healthcare Professionals. https://medical.23andme.com . Accessed Jan. 11, 2023.
- Wang K, Gaitsch H, Poon H, Cox NJ, Rzhetsky A. Classification of common human diseases derived from shared genetic and environmental determinants. Nat Genet. 2017;49(9):1319-1325.
- Kavitha S, Zebardast N, Palaniswamy K, et al. Family history is a strong risk factor for prevalent angle closure in a South Indian population. Ophthalmology. 2014;121(11):2091-2097.
- Khor CC, Do T, Jia H, et al. Genome-wide association study identifies five new susceptibility loci for primary angle closure glaucoma. Nat Genet. 2016;48(5):556-562.
- Vithana EN, Khor CC, Qiao C, et al. Genome-wide association analyses identify three new susceptibility loci for primary angle closure glaucoma. Nat Genet. 2012;44(10):1142-1146.
- Gharahkhani P, Jorgenson E, Hysi P, et al. Genome-wide meta-analysis identifies 127 open-angle glaucoma loci with consistent effect across ancestries. Nat Commun. 2021;12(1):1258. Published 2021 Feb 24.
- Fingert JH, Héon E, Liebmann JM, et al. Analysis of myocilin mutations in 1703 glaucoma patients from five different populations. Hum Mol Genet. 1999;8(5):899-905.
- Han X, Souzeau E, Ong JS, et al. Myocilin Gene Gln368Ter Variant Penetrance and Association With Glaucoma in Population-Based and Registry-Based Studies. JAMA Ophthalmol. 2019;137(1):28-35.
- Zebardast N, Sekimitsu S, Wang J, et al. Characteristics of p.Gln368Ter Myocilin Variant and Influence of Polygenic Risk on Glaucoma Penetrance in the UK Biobank. Ophthalmology. 2021;128(9):1300-1311.
- National Human Genome Research Institute. Polygenic risk scores. https://www.genome.gov/Health/Genomics-and-Medicine/Polygenic-risk-scores . Accessed Jan. 11, 2023.
- Nongpiur ME, Cheng CY, Duvesh R, et al. Evaluation of Primary Angle-Closure Glaucoma Susceptibility Loci in Patients with Early Stages of Angle-Closure Disease. Ophthalmology. 2018;125(5):664-670.
- Sekimitsu S, Wang J, Elze T, Segrè AV, Wiggs JL, Zebardast N. Interaction of background genetic risk, psychotropic medications, and primary angle closure glaucoma in the UK Biobank. PLoS One. 2022;17(6):e0270530. Published 2022 Jun 28.
- Fan BJ, Bailey JC, Igo RP Jr, et al. Association of a Primary Open-Angle Glaucoma Genetic Risk Score With Earlier Age at Diagnosis. JAMA Ophthalmol. 2019;137(10):1190-1194.
- Siggs OM, Qassim A, Han X, et al. Association of High Polygenic Risk With Visual Field Worsening Despite Treatment in Early Primary Open-Angle Glaucoma [published online ahead of print, 2022 Nov 10]. JAMA Ophthalmol. 2022;e224688.
- Lewis CM, Vassos E. Polygenic risk scores: from research tools to clinical instruments. Genome Med. 2020;12(1):44. Published May 18, 2020.
- Genetics of Glaucoma in People of African Descent (GGLAD) Consortium, Hauser MA, Allingham RR, et al. Association of Genetic Variants With Primary Open-Angle Glaucoma Among Individuals With African Ancestry. JAMA. 2019;322(17):1682-1691.
- Quetglas RB. PRS Methodology Appendix: Glaucoma. https://permalinks.23andme.com/pdf/23_21-PRSMethodologyAppendix_2022.pdf . Accessed Jan. 11, 2023.
- Ashenhurst JR, Zhan J. A Generalized Method for the Creation and Evaluation of Polygenic Scores. https://permalinks.23andme.com/pdf/23_21-PRSMethodology_May2020.pdf . Accessed Jan. 11, 2023.











