Do not leave your RCM to chance.
When the world stopped during the pandemic, many practices found themselves reviewing all facets of their business. One area that gained much attention was revenue cycle management (RCM) due to patient visits and revenue coming to an abrupt halt. In their review, some clinics realized there was uncollected money sitting in accounts receivable (AR), indicating their RCM was not running optimally.
Despite clinics having resumed normal business operations, RCM performance should stay top-of-mind to enhance the capture, management and collection of patient service revenue.
As you continue to monitor your cash flow in 2023, consider these five ways to optimize your revenue cycle and its management.
1. MONITOR YOUR METRICS
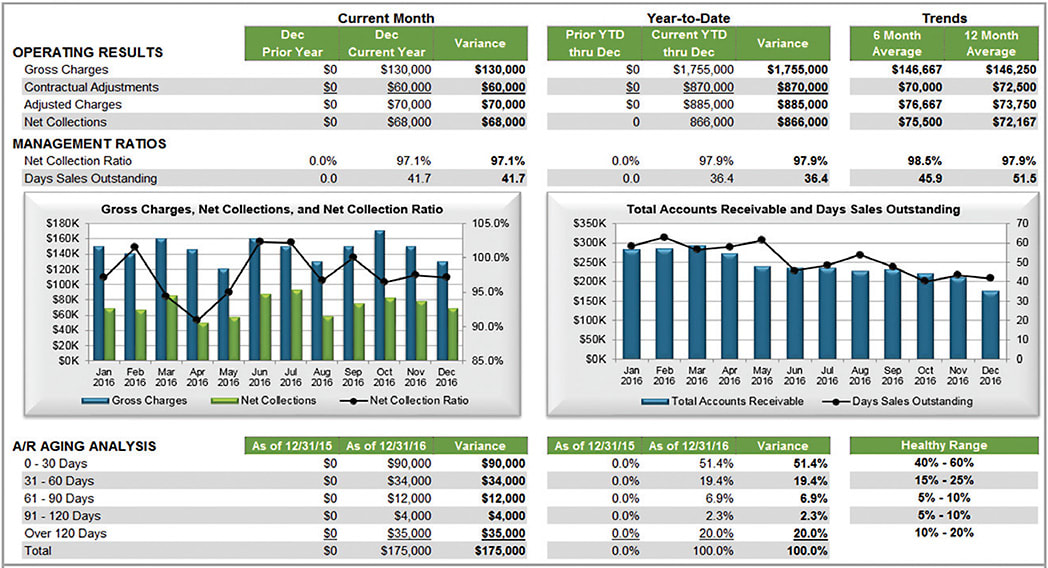
If you do not know your RCM benchmarks, start by tracking your internal data. Then use that information to calculate and compare to industry “standard” metrics. Those metrics include (Figure 1):

- AR aging analysis, which shows all monies the practice is trying to collect by a percentage over time. By breaking down the amount to be collected into aging buckets (0–30 days, 31–60 days, 61–90 days and so on), you can tell how long you have been trying to collect certain monies. This benchmark is calculated by dividing the balance in an aging bucket by the total AR amount. Typical healthy ophthalmology benchmark ranges are listed in Figure 1, but keep in mind that all industry measures are directional in nature. You can often spot a revenue problem if you monitor your aging percentages each month against external and internal benchmarks.
- Net collection ratio, calculated by dividing net collections by adjusted charges. Typically, a practice’s net collection ratio is 96%-104%,* indicating your team’s success in collecting reimbursable dollars.
- Days sales outstanding, the number of days it takes you to get paid for your services. The average is 19-33 days* when submitting a clean claim.
These three metrics can give you a good indication of how your business department is performing, and the easiest way to track them is to create a monthly dashboard report (Figure 2). It’s best to review your dashboard consistently to make sure your practice is running properly.
2. COMMIT TO TIMELY ACTION AND FOLLOW-UP
RCM success requires a team effort, including clinical and office staff. Their roles:
- Providers: Ideally, they should complete their chart notes on the same day as the patient exam to ensure timely billing. If there are extenuating circumstances, providers should finalize the chart within 24 hours of the visit. For surgeries, surgeons should confirm Current Procedural Terminology (CPT) codes and finalize the op note within 24-48 hours of surgery.
- Billing team: This group must have a system in place to process daily work, which includes posting new charges within 24 hours of the patient visit, posting payments received by insurance companies within 24-48 hours of receipt, and transferring remaining balances to patient responsibility immediately when posting and sending statements. The team should also work any denials right away to ensure they are addressed within filing deadlines.
Meanwhile, one billing team member should stay ahead of any takebacks or recoupment notice deadlines. If payers indicate that you owe them money, the practice should send the check back to the insurance company as soon as possible to avoid the accounting and posting hassle of next payment recoupments.
3. AGGRESSIVELY WORK ACCOUNTS RECEIVABLE
The total AR should be “worked” (meaning reviewed and researched) by billing staff every month, starting with charges older than 60 days. They should also work AR based on payers in this order:
- First, tackle commercial payer claims, starting with the highest amounts over 60 days. Begin with commercial payers, because contracts often require submitting a clean claim within 90 days. Addressing these first will avoid any timely filing issues and likely prevent delays in payments.
- Next, work on Medicare claims. Again, start with the highest amounts, which are usually related to surgeries. For Medicare, you can work on outstanding AR for 12 months after the date of service.
- Last, switch to patient AR, which has no timely filing limits. Still, be aware that the longer an AR exists, the less likely the full amount will be collected. Review each claim to ensure the patient owes the money. If so, review your statement log. Did you send the patient a statement indicating he or she is responsible for the amount? Depending on the claim’s age, you may need to call the patient regarding payment. Each month, the billing team should touch every late patient account owing the practice money. The team should also review patient credit balances each month, and patient refunds should be generated every 30 days.
4. MAXIMIZE YOUR SYSTEM SETUP
Try to automate as much as possible by using electronic tools (eg, batch eligibility checks and account ticklers) to help with processing. If you have not set up automated systems in your practice management system, check with your vendor to maximize these resources. To demonstrate the usefulness of automation, let’s look at the following collection process.
With the proper setup, many electronic practice management (EPM) systems can trigger a patient statement as soon as the billing team transfers an amount to patient responsibility. The practice can then run statements every day and avoid the billing department bottleneck that results in high call volumes for billing representatives. EPM systems can also generate another statement every 30 days if the patient has not paid.
As for patients who do not pay within 90 days, someone from the billing team should personally reach out to them by phone. If the practice does not receive payment or a response from a patient, ensure the team follows the practice’s policy for delinquent accounts.
5. SYSTEMIZE YOUR BILLING DEPARTMENT
Reduce waste by establishing financial and collections policies and creating department workflows that support them. Without standards in place, your billing team may spend time on unproductive tasks and, as a result, account follow-up may lag.
Two key policies to have established are the following:
- Small balance policy. This might state that the practice will not send patient statements for amounts less than $20, creating a reversible write-off. The amount will be reactivated on the patient’s account and collected at the next visit.
- Small credit policy. A similar approach can be followed if the practice owes the patient less than $10, with the amount credited to the next service.
Such policies and workflows allow for the best use of practice resources and enhance internal efficiencies.
THE BIG PICTURE
Maximize your RCM by understanding your benchmarks, analyzing your team’s workflows and creating an action plan to improve billing operations. Without standard processes and reporting, you may not know you have AR issues until it is too late. Timely and diligent monitoring will help ensure success for your practice’s RCM and overall finances. OM
* The cited healthy range amounts are developed by BSM Consulting, working with ophthalmic practices throughout the country. The healthy ranges are based on results between the 25th and 75th percentile rankings. This information is corroborated with other industry data and the AAO benchmarking database results.










