Our patient was a 51-year-old male with a past medical history of hypertension and a past ocular history of blunt trauma OD at age 5. Subsequently, he had developed a traumatic cataract s/p cataract extraction with insertion of posterior chamber (PC) IOL OD in 2019 and myopia OU s/p LASIK OU in 1997. He was seen by an outside ophthalmologist and found to have elevated IOP (37 mm Hg) OD as well as new iris mass OD.
The patient was started on dorzolamide-timolol and latanoprost and referred to our clinic for evaluation by both glaucoma and oncology.
THE OCULAR EXAM
During his evaluation, the patient complained of blurry vision OD. The ocular exam revealed the following:
- BCVA: 20/60 PH 20/20 OD, 20/20 OS
- Pupils: equal, round, briskly reactive without afferent pupillary defect
- IOP: 11 OD, 14 OS
- Pachymetry: 599 um OD, 554 um OS
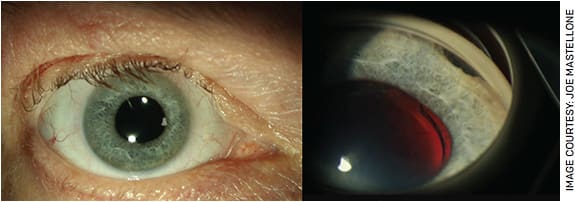
His slit lamp exam was significant for peripheral transillumination defects (TIDs), heme on the posterior lens capsule, a one-piece PC IOL with 2+ posterior capsular opacity (PCO) OD and nuclear sclerosis OS. The patient’s anterior chambers were deep and quiet OU, and corneas had clear LASIK flaps OU (Figure 1A). Gonioscopy revealed 2 clock-hours of iridodialysis inferiorly OD and 2+ diffuse angle pigmentation OU (Figure 1B). His posterior exam revealed a cup-to-disc ratio of 0.7 OU.
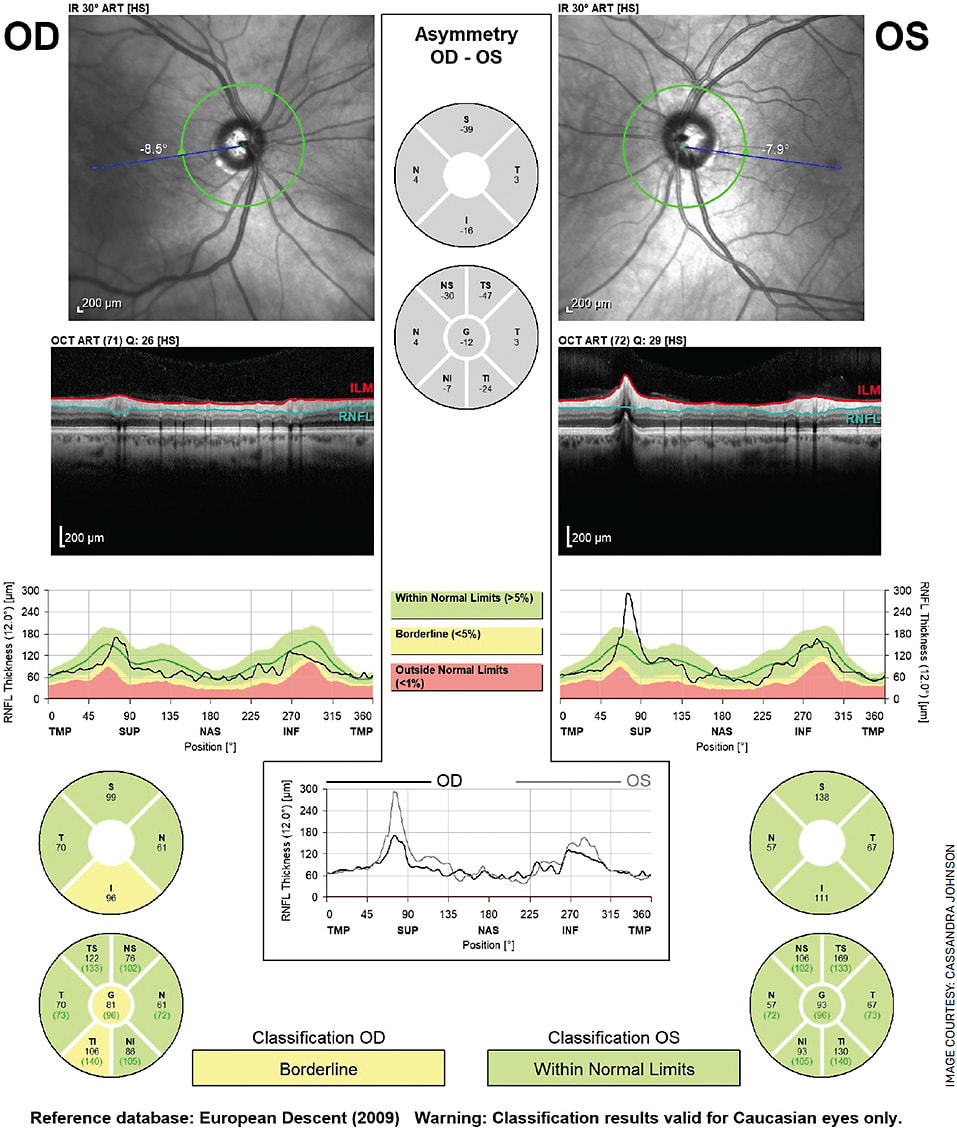
Quantitative nerve fiber layer assessment of the retinal nerve fiber layer (RNFL) and optic nerve head (ONH) using a Heidelberg Spectralis demonstrated borderline inferotemporal thinning OD; otherwise RNFL was full OU (Figure 2). Humphrey visual fields 24-2 was reliable and full OU.
To summarize, this patient had remote trauma OD resulting in traumatic cataract extraction and PC IOL placement as well as iridodialysis OD, and an episode of elevated IOP OD. Additionally, he was found to have TIDs, hyphema and borderline inferotemporal nerve fiber layer thinning on RNFL OD. Our suspected diagnosis was uveitis-glaucoma-hyphema (UGH) syndrome.
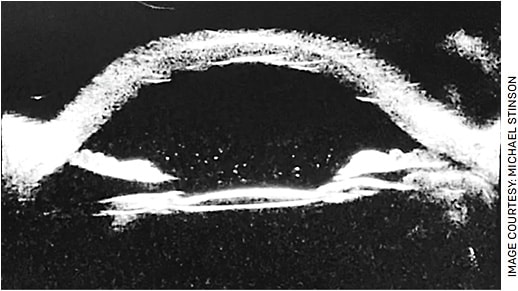
Other less likely diagnoses for elevated IOP in the setting of an iris transillumination defects include pigment dispersion syndrome/pigmentary glaucoma and pseudoexfoliation glaucoma. We obtained an ultrasound biomicroscopy (UBM) image. This study demonstrated a tilted PC IOL OD, confirming our diagnosis of UGH syndrome (Figure 3).
UGH SYNDROME
UGH syndrome, also referred to as Ellingson syndrome, was first described in 1977.1,2 Ellingson noted that implantation of specific anterior chamber (AC) IOL models was associated with iris chafing and subsequent mechanical irritation of uveal structures, hyphema and elevated IOP. Additionally, Ellingson confirmed that removal of these specific AC IOLs led to symptom resolution.
Historically, UGH syndrome has been associated with rigid AC IOLs; however, we now know that this complication can occur with placement of any type of IOL, including AC IOLs, intracapsular or sulcus-supported PC IOLs and scleral fixation IOLs.2-4 UGH syndrome may also result from malpositioned or poorly sized IOLs or by IOL instability due to zonular laxity or dehiscence.5 As IOL design and surgical techniques have improved, incidence of UGH syndrome has declined.6
Patients with UGH syndrome often present with complaints of blurry vision, pain, photophobia and/or redness in the affected eye. As implied by the name, common physical exam findings include AC inflammation characterized by cell and/or flare, red blood cells in the AC and elevated IOP; however, only one of these findings needs to be present for the diagnosis of UGH syndrome. The examiner should carefully assess the IOL, as patients may have a decentered lens or phacodonesis.
Retroillumination should be used to identify any TIDs, which usually overlie the haptic or area of the IOL that is chafing against the iris. Presence of a vitreous hemorrhage in the setting of the above findings is called UGH Plus syndrome.
DETECTION AND TREATMENT
Any patient suspected of having UGH syndrome should undergo thorough gonioscopy. The examiner should inspect the angle for increased pigmentation, blood or areas of zonular weakness/dehiscence. Regarding diagnostic imaging modalities, a prior study utilized UBM, which demonstrated IOL malpositioning in nine out of nine patients diagnosed with UGH syndrome.7 As was the case with our patient, the use of UBM can identify IOL tilt and IOL-uvea contact not easily discernable with slit lamp alone.
Treatment is initially directed at managing the individual components of this syndrome. AC irritation and inflammation, elevated IOP and hyphema are treated with topical corticosteroids, pressure-lowering agents and cycloplegics, respectively. However, definitive treatment of refractory UGH syndrome is to secure or replace the implanted IOL.
BACK TO OUR PATIENT
In this patient with blurry vision and PCO OD, an initial plan would have been to schedule him for YAG capsulotomy OD. However, concern for UGH syndrome given the patient’s hyphema and glaucoma is a contraindication for this procedure, as it could further destabilize the tilted PC IOL and complicate future IOL revision surgeries. Instead, he was continued on dorzolamide-timolol and latanoprost OD and referred to our cornea specialist for IOL repositioning or exchange. OM
REFERENCES
- Ellingson FT. Complications with the choyce mark VIII anterior chamber lens implant (uveitis-glaucoma-hyphema). J Am Intraocul Implant Soc. 1977;3:199-201.
- Ellingson FT. The uveitis-glaucoma-hyphema syndrome associated with the Mark VIII anterior chamber lens implant. J Am Intraocul Implant Soc. 1978;4:50-53.
- Armonaite L, Behndig A. Seventy-one cases of uveitis-glaucoma-hyphaema syndrome. Acta Ophthalmol. 2021;99:69-74.
- Accorinti M, Saturno MC, Paroli MP, et al. Uveitis-Glaucoma-Hyphema Syndrome: Clinical Features and Differential Diagnosis. Published online ahead of print, Apr. 1, 2021. Ocul Immunol Inflamm. 2021;1-6.
- Durr GM, Ahmed IIK. Intraocular Lens Complications: Decentration, Uveitis-Glaucoma-Hyphema Syndrome, Opacification, and Refractive Surprises. Ophthalmology. 2021;128:e186-e194.
- Apple DJ, Mamalis N, Loftfield K, et al. Complications of intraocular lenses. A historical and histopathological review. Surv Ophthalmol. 1984;29:1-54.
- Piette S, Canlas OA, Tran HV, et al. Ultrasound biomicroscopy in uveitis-glaucoma-hyphema syndrome. Am J Ophthalmol. 2002;133:839-841.










