3D HEADS-UP DISPLAY TECHNOLOGY
BY ARJAN HURA, MD
I am a firm believer in the many benefits of utilizing three-dimensional heads-up display (3D HUD) technology when operating. During the past decade, this technology has advanced as both hardware and software have evolved. As an alternative to traditional oculars, visualization with 3D HUD affords a multitude of benefits, including greater depth of field,1,2 a broad range of magnification,1 superior ergonomics,3 enhanced visualization,4 didactic teaching, integration of imaging for simultaneous viewing (OCT, endoscopic surgery, optiwave refractive analysis, etc.),5 the ability to record surgical videos in 3D for 3D playback, and comparable safety and efficiency.1,6
Apart from performing laser vision correction in a laser suite, I have not returned to the traditional operating microscope since residency and have found significant benefits in the process of untethering from oculars. I utilize 3D HUD technology exclusively when performing cataract surgery, refractive lens exchange, implantable collamer lens surgery and micro-invasive glaucoma surgery.
Two 3D HUDs are available on the market: the NGENUITY 3D Visualization System (Alcon) and the Artevo 800 (Zeiss). BVI also recently introduced the Beyonics One platform, an ophthalmic exoscope with augmented reality headset.
As with the evaluation of any new technology, the more one can carefully plan out implementation in advance, the less the chance of user error and unoptimized utilization and the greater the chance of having a positive and meaningful experience. When transitioning to 3D HUD, consider the following factors for successful OR implementation.
STUDY THE OPERATING ROOM LAYOUT
Implementing 3D HUD in the operating room involves the introduction of a standalone high-resolution 3D television that should be oriented parallel to the patient bed and at a certain distance from the surgeon for optimal viewing and ergonomic conditions. This potential change in orientation of patient bed and microscope can alter where the anesthesia team sits, so it is important to study each operating room in advance and game plan where all members of the team will be situated, where cords will travel and where the phacoemulsification machine will be placed.
Ideally, the OR should be set up so that there is no need to move the microscope or television if laterality of the operative eye changes from case to case. Bringing the patient into the room either headfirst or feet first will minimize time and burden on the OR staff so they do not have to constantly shift the microscope and television in the room between cases. Vitreoretinal or cataract surgeons who operate superiorly will not have this issue.
EDUCATE ALL TEAM MEMBERS
If technicians, nurses and the anesthesia team are working with 3D HUD at your surgery center for the first time, review the technology and settings with them in advance. The device manufacturer’s local representative can be instrumental in getting all other members of the team up to speed on logistics such as moving the unit, start up and shutdown, troubleshooting and connecting the 3D HUD to other imaging devices. Ask the manufacturer to trial the technology and conduct a dry run with the staff to simulate OR flow prior to utilizing the technology in surgery. The more comfortable everyone is with 3D HUD in advance of surgery, the smoother the implementation will be.
OPTIMIZE VISUALIZATION SETTINGS
Every surgeon has different microscope parameter preferences, and utilizing 3D HUD is no different. Work with the device manufacturer’s local representative to optimize your preferences for screen color temperature, level of microscope illumination, aperture size, color filters, resolution at different magnification settings, degree of microscope tilt and overhead room lights. If you are presbyopic and used to wearing spectacles or contact lenses, consider using full distance correction (this may need to be slightly adjusted depending on surgeon preference for distance from television screen). Ask the representative to be with you for the first several OR days or until fully comfortable with the technology, room orientation and device settings optimized to your preferences.
PREPARE FOR VIEWING SURGERY IN 3D
Those who have never experienced 3D viewing before or who are not used to wearing 3D glasses to experience movies, video games, augmented/virtual reality or surgery may need time to transition from the traditional oculars to 3D HUD. Device manufacturers are usually happy to host prospective users on their campus to conduct wet labs/simulations and can connect you with current 3D HUD surgeons to set up time to potentially visit them and see the technology in action.
Schedule routine cases at first, and don’t attempt complex cases until you feel comfortable with the technology. Everyone’s neuroadaptation period is different; some surgeons will be able to sit down and instantly feel comfortable visualizing surgery in 3D, and others may take several cases or several days before starting to fully feel comfortable with the benefits of the technology.

REFERENCES
- Freeman WR, Chen KC, Ho J, et al. RESOLUTION, DEPTH OF FIELD, AND PHYSICIAN SATISFACTION DURING DIGITALLY ASSISTED VITREORETINAL SURGERY. Retina. 2019 Sep;39(9):1768-1771.
- Agranat JS, Miller JB, Douglas VP, et al. The Scope Of Three-Dimensional Digital Visualization Systems In Vitreoretinal Surgery. Clin Ophthalmol. 2019 Oct 24;13:2093-2096.
- Hura A, Riemann C. Intraoperative Electromyogram Analysis of Postural Musculature with 3D Heads-Up Display Vs. Traditional Operating Microscope in Ophthalmic Surgery. July 26th, 2021. ASCRS, Las Vegas, NV.
- Palácios RM, de Carvalho ACM, Maia M, Caiado RR, Camilo DAG, Farah ME. An experimental and clinical study on the initial experiences of Brazilian vitreoretinal surgeons with heads-up surgery. Graefes Arch Clin Exp Ophthalmol. 2019 Mar;257(3):473-483.
- Ehlers JP, Uchida A, Srivastava SK. THE INTEGRATIVE SURGICAL THEATER: Combining Intraoperative Optical Coherence Tomography and 3D Digital Visualization for Vitreoretinal Surgery in the DISCOVER Study. Retina. 2018 Sep;38 Suppl 1(Suppl 1):S88-S96.
- Weinstock RJ, Diakonis VF, Schwartz AJ, Weinstock AJ. Heads-up Cataract Surgery: Complication Rates, Surgical Duration, and Comparison With Traditional Microscopes. J Refract Surg. 2019 May 1;35(5):318-322.
PREMIUM IOLS
BY BLAKE K. WILLIAMSON, MD, MPH, MS
Any time a new IOL receives FDA approval and is released into the market, every busy cataract surgeon — myself included — is tempted to hop on board immediately. This initial launch window is often filled with excitement, and a certain new lens euphoria takes place.
During these early stages, it’s tempting to jump right in and only focus on the potential benefits of the lens while overlooking the downside.
To avoid falling into this trap, I focus on a few key areas to ensure my team and I know as much about the lens as possible so we can be set up for success.
Here I’ll explain these areas of focus with examples from two of the most recent premium IOLs to come through our doors: J&J Vision’s Symfony OptiBlue and Lenstec’s ClearView 3.
1. TALK TO OTHERS WHO USE THE LENS.
Before using a lens, the first thing I do is talk to people who have experience with it. I’ll reach out to those who were involved in FDA studies or directly to the manufacturer who can tell me who has been implanting the lens. During these conversations, I want to go beyond what’s great about the lens. I ask these surgeons about the patients who were unhappy as well. There is no such thing as a perfect lens, and it’s critical that surgeons understand the flaws of each new IOL when they come to market.
With the Symfony OptiBlue, I spoke with Daniel Chang, who is an optics guru and has experience with a lot of J&J’s lenses. All diffractive lenses have different targets that you should use, and Dr. Chang advised me to aim for plano to first minus. He said this was the best opportunity not to cause some defocus but also give a little more near.
We also discussed its InteliLight technology, which is violet light blocking and provides really good vision in low light situations. While patients have low incidences of halos, glare and starbursts, I learned from Dr. Chang that some patients still noticed these while driving at night, which is understandable with any type of diffractive technology.
With the ClearView 3 (previously SBL-3), I spoke to Drs. Jim Loden and Jeff Whitsett. This is a segmented bifocal lens with a blending zone in the center. Typically, with a bifocal lenses you have the add power on the bottom for near and the top is for distance vision, but I learned from these surgeons that it still works quite well with different orientations or if it rotates a little. Also, the ClearView 3 is a square haptic, not your typical optic with the haptic arms, so I wanted some insight on how to place the lens. They advised that the lens is a little bulky and explained how to gently rotate it into the bag, particularly the trailing end.
We spoke about patient identification for this lens as well. I learned that ClearView 3 is a good lens for patients who are not typically good candidates for a diffractive technology, such as post-refractive patients or those with a mild epiretinal membrane. Also, they told me that it’s a good option for patients who are dependent on their vision for nighttime driving who may not be able to tolerative occasional halos, glare and starbursts.
2. IDENTIFY THE CHARACTERISTICS YOURSELF.
Although you can learn a lot about a lens from others, you need to have it in-house to truly know whether the lens is a good option for you and your patients. With the Symfony OptiBlue and ClearView 3, my experience has been very similar to that of my peers.
The Symfony OptiBlue has become my fastball for patients who desire spectacle freedom. I pair it with a Tecnis Synergy, which I place in the nondominant eye as my go-to pair for presbyopia correction.
We’re still in the post-market trials with ClearView 3, so I’m continuing to gain experience with that lens. But so far I’ve found that my patients can routinely achieve J2-plus vision with almost no dysphotopsia.
3. LEARN FROM YOUR PATIENTS.
You don’t want to perform the surgery and just send the patients back to the managing optometrist and never see them again. You can pick up a lot of nuances about a new lens that you wouldn’t learn otherwise by talking directly to the patient first.
When you start performing surgery with a new lens, I think it’s critical to personally see your postops with these first 20 to 50 patients. This allows you to follow the patients’ experience, ask them questions and learn directly how they’re doing. Also, as you learn how the lens behaves, you want to make sure you’re doing a trusted manifest refraction and entering in your postoperative result based on this feedback, whether it’s using ORA or another nomogram.
After about 50 implantations, I know whether a new lens is the real deal and is going to become part of my practice.
4. GET EVERYONE ON BOARD.
When you are launching a new lens, staff education is critical. Before we bring in a new lens, I explain to our entire team why we’re implementing the change and tell them about the key features of the IOL. Once they’re up to speed, we try to roleplay patient scenarios to make sure they are prepared to answer any questions. This usually takes place during a team lunch where we go over new technology additions to the practice.
The companies assist with staff education as well. With the Symfony OptiBlue, our local J&J rep spoke to our refractive team and our surgical counselors about the InteliLight technology. This is important because they educate and answer questions from patients about how it performs in low light situations.
Lenstec also sent a representative for an in-service day with my surgical team. Since we’re still in trials, we mainly watched surgical videos and then focused on lens loading, other surgical pearls and keys to patient selection.
5. HAVE REALISTIC EXPECTATIONS.
Finally, not all new IOL technologies are a success, so it’s good to have an exit strategy. You can aim for the best of outcomes, but if you’re going to offer new premium lens technology you need to have a good explant plan just in case.
ZEPTO
BY CRISTOS IFANTIDES, MD, MBA
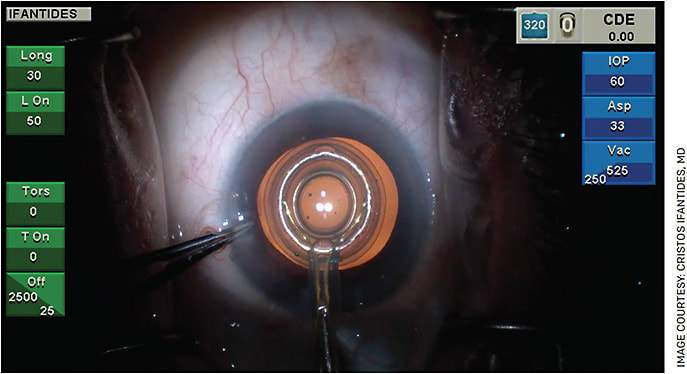
The Zepto precision pulse capsulotomy system (Centricity Vision) is a versatile device that I used extensively in my last academic practice and am getting up and running at the private practice I recently joined.
With any new technology, working through the logistics of adoption and whether your practice will benefit clinically and financially is of utmost importance. For Zepto, there is work upfront to consider along with a need to understand what it takes to get great results in the operating room.
CONSIDER YOUR PATIENT POPULATION
There are two main patient populations for which Zepto works best: premium cataract surgeries and complex surgeries. Zepto is great to help expand your premium conversion rate whether you use a femtosecond laser or not. It adds value by allowing the surgeon to center the capsulotomy on the visual axis, directly on the center of the premium IOL. Manual and femto capsulotomies are typically centered on the pupillary axis. It can also help make complex cases more routine by preventing the Argentinian flag sign on white cataracts, bypassing corneal scars for when visibility is poor, and can even help make the capsulotomy in zonulopathy cases. Peer-reviewed literature exists for both groups.
Zepto has made surgery safer and easier while allowing me to generate a new revenue stream for the practice by offering this new and different premium offering to our patients.
SURGICAL COUNSELING AND PRICING
Once you figure out if the technology is right for your practice, there are logistics that need to be addressed. For surgical counseling purposes, I like to describe the technology as “one step closer to perfect” and use the comparison of drawing a circle by hand versus one made with a stencil. Patients tend to understand the difference there and can grasp the value.
As for pricing, this service allows for different models, including bundled and a la carte. Depending on your current pricing model, either way works. It is important, however, to remember that unlike femtosecond laser, you are unable to charge extra for the Zepto service in patients undergoing routine, non-astigmatism correcting monofocal IOL placement since you are not addressing the astigmatism with the device. For adoption to be successful, your surgical counselors, practice managers and other surgeons all must be on the same page about the added value and messaging.
TRAINING
Centricity Vision does an incredible job of training surgeons and staff. During a device trial, their knowledgeable trainers arrive at your practice to train staff on using the device and remain with the surgeon throughout the day doing surgical cases.
Staff training takes only a few cases, so a day should be enough, especially if you only need to train a couple of staff members. Training includes understanding the technology, how to manage the console, connecting the handpiece tubing to the console, how to handle the handpiece itself and going through the motions of the surgical steps, including the release step. The “release” at the end of the capsulotomy procedure is often the most challenging part for staff. Working with the trainers on this will get them up to speed and prevent any OR slowdowns. In addition, I recommend watching a couple of online videos of the device in action on the company’s website.
On the surgeon side, training includes handling of the handpiece, insertion and removal from the eye, positioning and tips for successfully centering the capsulotomy device on the patient’s visual axis. Routine cases work best for this, and I would advise against trying this device on complex cases without first having 10 or so routine cases under your belt.
The online training offered on Centricity Vision’s website is quite good for the surgeons and only takes about 30 minutes to do. I found value in the training modules even after using the device many times. Similar to in-person training, the online training goes over handpiece handling, insertion and removal and techniques for successfully centering the capsulotomy device on the patient’s visual axis. This helps you master the steps of the technique before stepping foot in the operating room.
FEMTOSECOND CATARACT TECHNOLOGY
BY GREGORY D. PARKHURST, MD, PCEO
I have used femtosecond laser technology for 10+ years. My first experience training with this technology occurred during my fellowship with Dr. Steven Slade in Houston. During this time, I learned that it’s not sufficient to just read about this technology or see it on a show floor. Until you’ve experienced it in your own hands, it’s hard to truly appreciate the benefits of the femtosecond laser cataract surgery .
Since my early experience, I’ve discovered that a successful implementation of femtosecond laser technology is easily attainable, because it’s really just a shift in mindset. We’re not talking about expensive advertising campaigns or hiring new staff to sell the technology — it’s a matter of believing in the technology, understanding its benefits and properly conveying those benefits to patients.
Here are the most important factors that will lead to a successful implementation of a femtosecond laser system.
1. BUY-IN
Having surgeons who believe in the technology is the first and single most important thing that will lead to success. For surgeons to use any new technology, they have to buy in to the idea that it’s in their patients’ best interests. If there are questions in the surgeon’s mind about whether that’s the case, it will never be successful.
Femto has been a hot button issue for years now and resulted in some polarization between the pro- and antifemto crowds. If you and your team are already in the pro-femto group, you can move on to step two.
If you are not currently pro femto, there probably aren’t enough peer-reviewed papers or conversations with trusted colleagues to convince you. So, I recommend seeing these platforms in action, which I feel can go a long way to dispel some outdated femto myths, including that it is inefficient or causes tags and anterior capsular rents.
I had the opportunity to experience it myself in the early days. Now, I pass that along when training my own fellows. Anyone who goes through my fellowship gets a year-long training in the use of femto technology. In addition, LENSAR has arranged for interested surgeons to visit me and spend the day observing me use the ALLY system. Many of these surgeons are seeing femto in action for the first time, and this experience allows them to observe many interesting surgical scenarios where femto can be particularly helpful, including things such as white cataracts, loose zonules and “squeezy” patients to name just a few, not to mention its capability with astigmatism management. I recommend surgeons reach out to the manufacturers to see if they can make a similar arrangement.
2. PATIENT EDUCATION
Much of the cataract patient population is not well informed about cataracts and cataract surgery. This requires surgeons and staff to be equipped to properly educate patients on the diagnosis and process of cataract surgery so they can explain the benefits of femtosecond laser technology.
I have found that many patients come to us with assumptions of the cataract surgery process. In many situations, patient have a baseline expectation or assumption that cataract surgery is a laser procedure and don’t know it has historically been done via phacoemulsification without a laser. So, it’s in our best interests to lean into these baseline expectations and not get in our own way with our approach to femto.
Our practice does not have the mindset that femto is an upgrade — rather, it is our standard technique recommended for most patients. That’s not to say basic cataract surgery without astigmatism management when necessary is bad — with basic cataract surgery we can successfully remove the cataract, and patients can have a very good result in terms of clarity of vision.
However, femto is our gateway to refractive cataract surgery with or without a premium IOL, which allows us to correct refractive error with precision as well as astigmatism and presbyopia. Because of this, femtosecond laser cataract surgery is our standard offering when we first approach cataract patients who need astigmatism and/or presbyopia management.
It’s important to note that many patients don’t even understand what a cataract is. Some assume it’s a film or growth over the top of the eye that just needs to be peeled off. So, before patients are equipped to decide on a refractive cataract procedure, femtosecond laser technology and/or a premium IOL, we first need to educate them that a cataract is a clouding of the lens that impacts their vision and that with cataract surgery we remove the natural lens and replace it with an artificial lens. Then, we can properly move on to the methods of removal and lens options at our disposal
We make sure that patients are made aware of this for the first time before they arrive in our office. First, we ensure that doctors who commonly refer cataract patients to us provide basic education on their treatment options. Second, when patients call to make an appointment, our phone team gives them a heads up of what they can expect during their evaluation. We tell them that this will include a discussion of options and what is and is not covered by their insurance. In addition, we send educational videos for them to watch before they arrive. Our hope is that at least one of these messages sticks so they aren’t hearing this for the first time in our office.
3. STAFF EDUCATION
Staff have a primary role in providing patient education, so they need the proper training to make sure they are equipped to communicate with patients about cataract surgery and femto.
One way we do this is by bringing the staff into the operating room to observe surgery, similar to what we do with surgeons visiting our practice. We have them watch a series of basic manual cataract surgeries followed by a series of cataract cases using the ALLY system so they can witness the differences firsthand. In this regard, 3D heads up technology is very helpful. Staff put on the 3D glasses and are able to truly see and appreciate what the surgeon is seeing for both methods of cataract surgery.
In addition, we explain to staff the key benefits of this technology so they can discuss them with patients. For example, when we are recommending ALLY to treat a patient’s astigmatism, we coach staff to discuss that femto best suited to produce a precise and repeatable result that is necessary when placing a premium IOL.
Our staff members also know to talk about the comfort and efficiency of this process. They tell cataract patients not to expect a long surgical experience — we are able to dock and do a laser treatment in about 30 to 40 seconds.
4. PRESENT WITH CONFIDENCE
This ties back to the first step. We have a duty to our patients to recommend what we feel is in their best interests. If you believe in the technology enough to invest in it, the cost of femto should not make you shy about presenting it to patients. Even with the out-of-pocket costs associated, you should be confident in recommending it to patients because you feel you are delivering a valuable service.
Our practice has success with this technology because we know it’s worth it. And we find that our patients are happy to invest in it, because we convey how much it will transform their lives. So, celebrate that opportunity. If you don’t believe that it’s worth the cost, your patients are never going to believe it’s worth it either. OM












