BEST PRACTICES FOR TELEHEALTH
- Use HIPAA-compliant software such as Zoom, Epic, Teams, Doximity, Vidyo and Doxy.me .
- Designate telehealth-only clinics; do not mix with in-person clinics.
- Engage your office staff for telehealth visits.
- Messaging is critical. Staff must be trained and scripted for positive messaging.
- Include messaging and consent for telehealth visits in your patient registration forms.
- Group chat with your team on virtual visit days to maintain communication.
- Follow your standard exam procedure, including tech and scribe workflows.
- Use a scribe who can join the visit virtually.
- e-Checkin streamlines the tech workup and engages patients further.
Telehealth has become a normal part of a physician’s toolkit, expanding services to patients that they have come to enjoy and expect. Virtual care continues to grow, with 76% of U.S. hospitals and physicians using it in some form, according to the American Hospital Association. This trend is expected to continue as patients increasingly demand more accessible and convenient care options — and as physicians look for ways to expand their reach and improve health outcomes. However, as the public health emergency (PHE) is set to end on May 11, 2023, there have been updates to telehealth policies, regulations and reimbursement guidelines.
In 2023, physicians can bill for a range of telehealth services. The Centers for Medicare and Medicaid Services (CMS) sets the guidelines for billing and coding for these services. These include the ability to provide telehealth services regardless of where the patient or physician is located.
This article should help shed light on what visit types can still be used in ophthalmology and how to use them.
SYNCHRONOUS VIDEO VISITS
These are real-time video visits between a physician and patient using a HIPAA-compliant platform. Physicians can bill using CPT codes 99201-99215 for evaluation and management (E/M) services with the GT or -95 modifier to indicate telemedicine services. These visits can be utilized for new, established, tele-counseling and post-operative patients. Examples include triage of new complaints, monitoring of chronic conditions such as dry eyes, pre-op counseling for surgery, and post-operative visits.
URGENT CARE/TRIAGE VISITS
Virtual triage and urgent care have been implemented across the country as a practical way to manage patients with low-acuity conditions remotely while expediting treatment of high-acuity patients. While common conditions such as chalazia and conjunctivitis are managed virtually, patients suspicious for more serious issues including new flashes and floaters, vision loss or eye trauma are expedited for timely in-person evaluation.
Physicians can bill using CPT codes 99201-99215 (GT/-95) for E/M services, for new or established patients.
TELE-COUNSELING VISITS
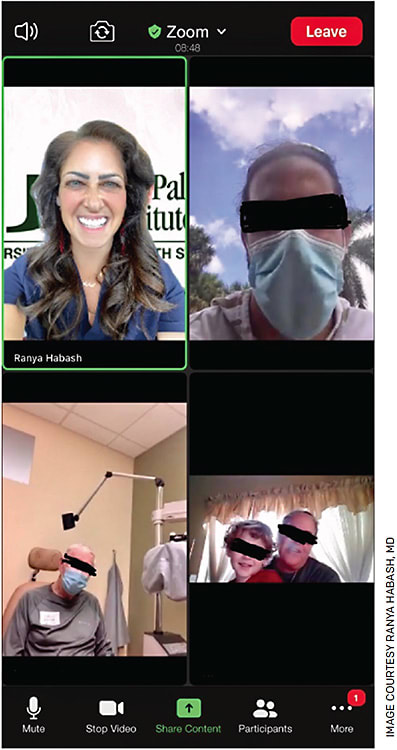
Video visits dedicated to discussion and counseling lend themselves well to a virtual workflow. We’ve observed that patients seem more relaxed in their home environments and family members participate more often, either virtually or in the patient’s home (Figure). Cataract and refractive discussions, uveitis, neurologic and genetics counseling are some examples of visit types.
Physicians can bill using CPT codes 99201-99215 (GT/-95) for E/M services, and these can be time-based visits in the case of long counseling sessions.
HYBRID VISITS
This may be the most popular and lasting form of telehealth for all involved. In-person testing is performed with a subsequent video visit to relay results and discuss management. Hybrid visits significantly minimize wait times for patients while improving clinic flow.
Retina and glaucoma patients requiring optical coherence tomography imaging, IOP checks and visual field testing are well-suited for this visit type, for example. Patients who merit treatment, such as intravitreal injection, are scheduled for expedited procedure-only visits on a standard clinic day.
As hybrid visits have advanced, many physicians are now managing patients at multiple locations virtually on the same day, limiting travel by all. After-hours and weekend clinics have been implemented for greater scheduling flexibility as well as the utilization of office time on surgery days.
SECOND OPINION CONSULTS
Many departments and practices now offer domestic and international second opinion virtual consults. Patients are scheduled for telehealth appointments with the appropriate specialists, and their medical records are uploaded to the EHR. The physicians review the records and perform video consultations. Referring physicians can be included as well, allowing them to keep and care for their own patients locally. These visits are less costly for patients, avoid unnecessary travel and allow patients in underserved areas to receive tertiary level care.
Some of the most common examples of second opinion consults include those for IOL selection in cataract surgery, retinal detachment repair options, pediatric conditions such as amblyopia, and observation vs injection for macular degeneration cases.
Of note, recent changes in the regulations require physicians to be licensed in the state where the patient is located at the time of treatment. There are some exceptions to the rule, but these vary significantly between states. The Interstate Medical Licensure Compact is an option for physicians looking to practice in multiple states. The compact allows licensed physicians to apply for expedited licensure in participating states, making it easier to work across state lines. As of March 2023, 30 states have joined the compact.
E-VISITS FOR ONLINE COMMUNICATION
Though rarely recognized as virtual care, correspondence via email and portal has skyrocketed. This is most common for patient-initiated image review, triage and response to follow-up questions. These visits can be billed using CPT codes 99421-99423.
REMOTE PATIENT MONITORING
A major development in telehealth is the increasing availability of remote patient monitoring (RPM) services, which allow patients to monitor their health from home using software and devices for chronic conditions including glaucoma, macular degeneration, dry eyes, diabetic retinopathy and amblyopia. Eyecare-specific software and devices include those for home perimetry, home tonometry and electronic Amsler grids. RPM can help improve patient outcomes and alert patients and physicians of acute changes in status which allows for timely intervention.
Of note, as of the end of the PHE, RPM services will be permitted for established patients only and will require 16 measurements per month (every other day). Physicians can bill for remote patient monitoring services using CPT codes 99453, 99454 and 99457, which cover initial setup and require just 20 minutes of cumulative clinical staff time per month.
TELEPHONE VISITS
During the PHE, Medicare temporarily waived the audio-video requirement and reimbursed telephone-only visits similarly to in-person visits. With the end of the PHE, however, regulations and reimbursement for telephone visits will change according to individual state and payer policies.
CONCLUSION
Telehealth has introduced benefits to patient care, safety, patient and physician satisfaction, workflow efficiency and health-care costs. It is a rapidly evolving area of health-care delivery, and physicians should continue to follow the specific requirements in their states.
Hopefully this article can help with ensuring the persistence and progression of this new paradigm. OM









