Over the last decade, we’ve seen many advances made in our therapeutic approach to dry eye and ocular surface disease, including multiple procedural treatments that provide expanded options for our patients. Here’s a look at three conditions that come under the ocular surface disease umbrella, and the latest information on the treatments we have to address them.
MEIBOMIAN GLAND DISEASE
Meibomian gland disease (MGD) is the leading cause of dry eye disease (DED) in the United States. It includes a cycle of decreased quality and/or quantity of meibomian gland secretions, gland obstruction, and atrophy and keratinization of the gland orifices.1,2
Initial treatment often includes a combination of heat application to the eyelids and eyelid massage. However, patient compliance is often poor, and many patients experience persistent symptoms and gland blockage despite regular home treatment.
MGD TREATMENTS
Thermal expression/blepharoexfoliation
Thermal expression has been shown to be an effective method for treating MGD with multiple studies of various available devices showing both subjective and objective improvement in patient’s ocular surface disease.3-5 Several devices are available on the US market that deliver simultaneous or sequential heat and expression to the eyelids to soften and express the stagnant and viscous meibum (Table).
| DEVICE | MANUFACTURER | DESCRIPTION |
| LipiFlow | Johnson & Johnson Vision | Applicators placed on either side of the eyelid deliver simultaneous heat and massage |
| TearCare | Sight Sciences | External heat applicators placed over each eyelid, followed by manual gland expression |
| iLux | Alcon | Handheld device delivering heat on either side of the eyelid with simultaneous gland expression |
| MiBo | MiBo Medical | Heated metal eye pad placed over eyelid, often followed by manual gland expression |
| Thermal 1-Touch | OCuSOFT | Eye mask applies heat to the external lid, often followed by manual gland expression |
| BlephEx | BlephEx LLC | Microsponge on handheld device that is used along eyelid margins and lashes to perform blepharoexfoliation |
Duration of treatment effect varies depending on multiple factors, including the device used, disease severity and response to treatment. For example, the LipiFlow Thermal Pulsation System (J&J Vision) has been shown to improve meibomian gland function and reduce dry eye symptoms after a single 12-minute treatment.6 Meibomian gland secretion scores and tear break-up time improved significantly from baseline to 1-month post-treatment, and this improvement was maintained with no significant regression at 9 months.7
TearCare (Sight Sciences) has shown positive effects on the signs and symptoms of DED persisting for at least 6 months (Figure 1).8 TearCare and LipiFlow have been shown to be equivalent in alleviating signs and symptoms of dry eye in patients with MGD with a similar safety profile, but TearCare has shown superiority in improving quality of vision and DED symptom frequency in subjects with more severe meibomian gland dysfunction.9,10

Thermal treatments can be offered as a single treatment for flares of symptomatic disease or for maintenance therapy every 6-12 months or when symptoms begin to worsen or recur.
Lastly, BlephEx can be used to perform blepharoexfoliation, whereby a medical grade micro-sponge on a handheld device is used along the edge of the eyelids and lashes to provide precise exfoliation, unroof the meibomian glands and removes excess bacteria and the inflammatory biofilm that leads to chronic MGD and eyelid irritation.
Intense pulsed light
Intense pulsed light (IPL) is a non-invasive procedure that uses a polychromatic, broad-spectrum light source with variable wave lengths ranging from 500 nm to 1,200 nm directed to the skin (Table). IPL treats a variety of conditions, including hyperpigmentation, telangiectasias, facial and ocular rosacea and MGD. The emitted light is selectively absorbed by specific chromophores, such as blood vessels or melanin; the thermal effects lead to the liquefaction of meibum when applied to the periocular skin. Several studies have shown the efficacy of IPL for the treatment of MGD, though the specific mechanism is not fully understood.6,11-15
For optimal efficacy, a series of treatments spaced by 3-6 weeks is typically performed and often include a treatment to the periocular skin followed by manual expression of liquified meibum. Optima IPL and OptiLight (Lumenis) and Eye-Light (Topcon Healthcare) are a few of the IPL devices available for the treatment of DED.
The limitation of this treatment includes caution in treating patients with darker skin tones (Fitzpatrick Skin Types V&VI). As with any medical procedure, there are potential risks and side effects associated with IPL, such as burns, irritation and pain. These are usually mild and short-lived, but patients must be informed of these potential risks before the procedure.16
AQUEOUS DEFICIENT DRY EYE
Punctal occlusion and punctal cautery
Many dry eye patients have either predominantly aqueous deficient DED or mixed mechanism DED with a component of aqueous deficiency. A decreased tear lake is a helpful indicator of aqueous deficient dry eye, in addition to significant corneal erosions without significant MGD.
Many of these patients benefit from punctal occlusion and/or punctal cautery. Collagen punctal plugs that dissolve over 3-6 months (such as SOFT PLUG Collagen Plugs, Oasis Medical; DuraPlug, Katena; Vera90 synthetic extended punctal inserts, Lacrivera) can be placed in the lower and/or upper puncta to slow the drainage of tears from the ocular surface and retain a higher tear volume.
Collagen plugs can be trialed first; if patients have a positive response, non-dissolvable silicone plugs (SOFT PLUG Collagen Plugs, Oasis Medical or SuperEagle punctum plug [EagleVision]) can then be employed.
Plugs can be placed in all four puncta in cases of severe dryness. They can be billed to insurance and are an expedient procedural intervention from which patients can benefit.
In cases where plugs do not fit well in the puncta or constantly fall out, punctal cautery (Bovie disposable high temperature fine tip cautery, Bovie) can be performed to permanently scar the puncta and achieve the same effect. Punctal cautery can be done in the office setting with high-temperature, fine-tipped, handheld cautery, such as Alcon’s Optemp II V, after anesthetizing the punctal orifices with subconjunctival lidocaine and/or lidocaine gel or an injection of subcutaneous lidocaine close to the punctal opening.
The procedure can also be billed to insurance and can be extremely beneficial for patients with severe OSD.
CONJUNCTIVOCHALASIS
Conjunctivochalasis (CCH) is a condition characterized by the loss of elasticity and of the conjunctiva, resulting in loose and redundant tissue often overlying the lid margin and interrupting tear clearance and homeostasis. CCH has been associated with both aqueous deficient and evaporative DED and is associated with symptoms such as dryness, irritation, and foreign-body sensation.
TREATMENTS FOR CCH
To start out
Conservative and initial treatment options for CCH include frequent lubricating drops, gels or ointments, steroid drops for pulse-dosed or chronic use and/or punctal plugs in attempts to stabilize the tear film. In cases of severe CCH that fail conservative measures, conjunctival resection is an effective treatment option to eliminate the mechanical effects of the redundant tissue on tear clearance and the lid margin. Several methods of conjunctival resection can be effective in management, including simple resection with closure with suture or fibrin glue.17
Newer surgical approaches
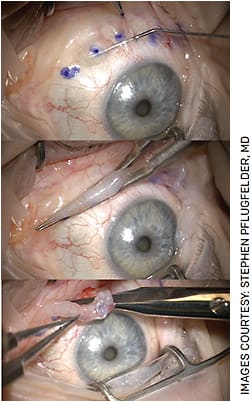
The paste-pinch-cut (PPC) conjunctivoplasty method published by Doss et al is another effective and comfortable technique for patients. Small incisions are made in the inferior redundant conjunctiva, and fibrin glue is introduced and polymerized subconjunctivally to allow for a controlled and sutureless excision of the redundant tissue (Figure 2).18
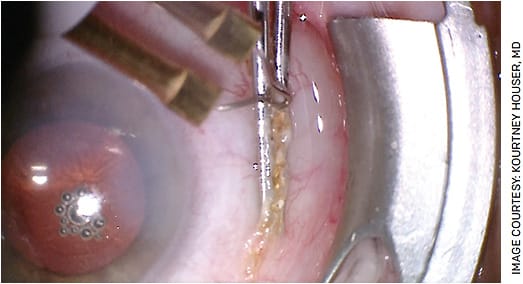
Conjunctival coagulation and shrinkage using cautery is also effective and can be performed in the office.19 After topical anesthetic is applied, handheld high or low temperature cautery (Bovie disposable low/high temperature fine tip cautery) is applied in a linear fashion to inferior bulbar conjunctiva gathered with angled tying forceps, typically 3-4 mm inferior to the lower limbus so the cauterized area is covered by the lower eyelid (Figure 3). Caution should be taken in cases of autoimmune disease, as cautery can be pro-inflammatory and melts can occur.
A short course of topical steroids and antibiotics are often started following the procedure, and artificial tears can be used to minimize postoperative irritation and burning. Performing conjunctival cautery can be time-saving and cost-effective for the patient as compared with surgical resection/PPC techniques that require a trip to the operating room.
SUPERIOR LIMBIC KERATOCONJUNCTIVITIS
Superior limbic keratoconjunctivitis (SLK), which is characterized by inflammation of the superior tarsal and bulbar conjunctiva, is often associated with superior peripheral corneal erosions, filament formation and symptoms of irritation. SLK has many systemic associations, including DED, thyroid eye disease, floppy eyelid syndrome and graft vs host disease, though many cases occur with no known systemic association.19,20 Mechanical injury due to redundant conjunctiva and repeated microtrauma with blinking are believed to be contributors to SLK, though the specific pathogenesis is not fully known.19
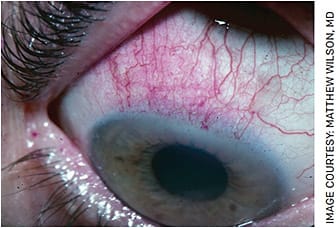
Diagnosis can be easily made with lissamine green or rose bengal dye revealing superior bulbar conjunctival erosions or a concentration of corneal erosions at the superior limbus staining with fluorescein (Figure 4).
SLK TREATMENTS
Initial treatment regimens often include topical lubricants, bandage contact lenses and anti-inflammatory agents. For refractory cases, several procedural options have been shown to be effective and well-tolerated. These include superior conjunctival excision with or without amniotic membrane and superior bulbar conjunctival cautery (Figure 5).21,22 While both of these procedures can be well-tolerated in an office-based setting, conjunctival excision with amniotic membrane is often performed in the operating room for improved patient comfort.

SUMMARY
Many procedural treatments for dry eye are available that can broaden our therapeutic offerings to our patients with this chronic and often progressive disease, including thermal expression, microblepharoexfoliation, IPL and punctal occlusion/cautery.
Investment in thermal pulsation and/or microblepharoexfoliation devices can be practice and revenue builders and can help attract more dry eye and MGD patients with recalcitrant signs and symptoms seeking a higher level of care/procedural intervention and have failed more conservative therapies.
A careful and thorough clinical exam can also help to detect ocular surface conditions such as SLK and CCH that can worsen dry eye symptoms and are often better treated with surgical or procedural interventions than drops alone.
Expanding our OSD treatment offerings to include these procedures gives us tools to expand and improve our ocular surface treatment algorithms and bring relief to patients. OM
REFERENCES
- Craig JP, Nichols KK, Akpek EK, et al. TFOS DEWS II definition and classification report. Ocul Surf. 2017;15:276–283.
- Nelson DJ, et al. The international workshop on meibomian gland dysfunction: report of the definition and classification subcommittee. Invest Ophthalmol Vis Sci. 2011;52: 1930–1937.
- Nichols KK, Foulks GN, Bron AJ, et al. The international workshop on meibomian gland dysfunction: executive summary. Invest Ophthalmol Vis Sci. 2011;52:1922-1929. doi:10.1167/iovs.10-6997a
- Blackie CA, Carlson AN, Korb DR. Treatment for meibomian gland dysfunction and dry eye symptoms with a single-dose vectored thermal pulsation: a review. Curr Opin Ophthalmol. 2015;26:306-313. doi:10.1097/ICU.0000000000000165
- Wesley G, Bickle K, Downing, J, et al. Systane iLux Thermal Pulsation System in the treatment of meibomian gland dysfunction: A post-hoc analysis of a 12-month, randomized, multicenter study. Clin Ophthalmol. 2022 Nov 3;16:3631-3640.
- Greiner JV. A single LipiFlow Thermal Pulsation System treatment improves meibomian gland function and reduces dry eye symptoms for 9 months. Curr Eye Res. 2012;37:272-278. doi:10.3109/02713683.2011.631721
- Badawi D. A novel system, TearCare, for the treatment of the signs and symptoms of dry eye disease. Clin Ophthalmol. 2018;12:683-694. Published 2018 Apr 10. doi:10.2147/OPTH.S160403
- Gupta PK, Holland EJ, Hovanesian J, et al. TearCare for the treatment of meibomian gland dysfunction in adult patients with dry eye disease: A masked randomized controlled trial. Cornea. 2022;41:417-426. doi:10.1097/ICO.0000000000002837
- Holland EJ, et al. A comparison of TearCare and Lipiflow systems in reducing dry eye disease symptoms associated with meibomian gland disease. Clin Ophthalmol. 2022 Aug 30;16:2861-2871.
- Toyos R, McGill W, Briscoe D. Intense pulsed light treatment for dry eye disease due to meibomian gland dysfunction; a 3-year retrospective study. Photomed Laser Surg. 2015;33:41–46.
- Kassir R, Kolluru A, Kassir M. Intense pulsed light for the treatment of rosacea and telangiectasias. J Cosmet Laser Ther. 2011;13:216-222. doi:10.3109/14764172.2011.613480
- Craig JP, Chen YH, Turnbull PR. Prospective trial of intense pulsed light for the treatment of meibomian gland dysfunction. Invest Ophthalmol Vis Sci. 2015;56:1965–1970.
- Giannaccare G, Pellegrini M, Carnovale Scalzo G, et al. (2023). Low-level Light therapy vs intense pulsed light for the treatment of meibomian gland dysfunction: Preliminary results from a prospective randomized comparative study. Cornea. 2023;42: 141-144. doi: 10.1097/ICO.0000000000002997.
- Piyacomn Y, Kasetsuwan N, Reinprayoon U, et al. Efficacy and safety of intense pulsed light in patients with meibomian gland dysfunction-a randomized, double-masked, sham-controlled Clinical Trial. Cornea. 2020;39:325–332.
- Leng X, Shi M, Liu X, et al. Intense pulsed light for meibomian gland dysfunction: a systematic review and meta-analysis. Graefes Arch Clin Exp Ophthalmol. 2021;259:1-10. doi:10.1007/s00417-020-04834-1
- Cote S, Zhang AC, Ahmadzai V, et al. Intense pulsed light (IPL) therapy for the treatment of meibomian gland dysfunction. Cochrane Database Syst Rev. 2020;3:CD013559. Published 2020 Mar 18. doi:10.1002/14651858.CD013559
- Marmalidou A, Palioura S, Dana R, Kheirkhah A. Medical and surgical management of conjunctivochalasis. Ocul Surf. 2019;17:393-399. doi:10.1016/j.jtos.2019.04.008
- Doss LR, Doss EL, Doss RP. Paste-pinch-cut conjunctivoplasty: subconjunctival fibrin sealant injection in the repair of conjunctivochalasis. Cornea. 2012;31:959–62.
- Lahoti S, et al. Superior limbic keratoconjunctivitis: a comprehensive review. Survey of Ophthalmology. 2022:331-341.
- Kadrmas EF, Bartley GB. Superior limbic keratoconjunctivitis: A prognostic sign for severe Graves ophthalmopathy. Ophthalmology. 1995;102:1472-1475.
- Donshik PC, Collin HB, Foster CS, Cavanagh HD, Boruchoff SA. Conjunctival resection treatment and ultrastructural histopathology of superior limbic keratoconjunctivitis. Case Reports Am J Ophthalmol. 1978 Jan;85:101-10.
- Udell IJ, Kenyon KR, Sawa M, Dohlman CH. Treatment of superior limbic keratoconjunctivitis by thermocauterization of the superior bulbar conjunctiva. Ophthalmology. 1986;93:162-166.











