The most impactful recent growth in our cataract surgery practice, driven by both the patients and physician desire to achieve the most optimal results, has been centered around implementing new IOL technology. We have noticed that the more growth seen in premium IOL utilization, or advanced cataract surgery, the more growth also seen in monofocal IOL technology, or traditional cataract surgery.
Ultimately, patients want a balanced education process that helps them make an educated decision on what implant vision is best for them for the rest of their life. And patients talk with each other! The most powerful marketing for your practice is a happy patient telling a future potential patient that they received a balanced education process about their vision options at your center followed by great surgery and care to help them achieve their visual goals.
In this article, we’ll discuss the preoperative education process.
EDUCATING YOURSELF AND YOUR TEAM
When adding a new premium implant to your practice, you want to educate yourself about all its features that represent an advancement. Your confidence in the technology will lead to you being excited, which the whole practice will feel.
It helps greatly to educate your whole team about the new technology as well so they understand why you have confidence in it. Since most of the time your patients are not with you but rather with a member of your team (Figure 1), it is important that your team understand the technology and their role in helping to complete the premium implant patient experience cycle.
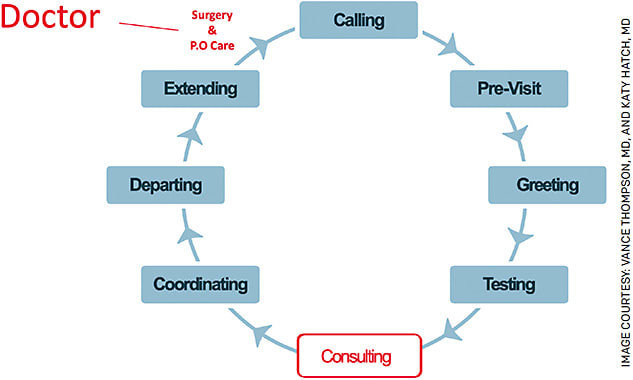
FIGURE. The doctor (red) and the team (blue) roles in “The Premium IOL Patient Experience Cycle”
GUIDE THE PATIENT
Patients simply want to make the best implant choice “for them” for the rest of their visual life. Which implant they choose is one of the biggest decisions they will make for the rest of their life. As physicians, our job is to guide the patient in this decision. We can use our training and lifelong learning to help our patients make the best possible decision if we dive into understanding their goals, personality and visual system details. This allows us the honor of making a life-changing recommendation based on that powerful combination of our knowledge and their situation.
If you remember one thing in this article, it should be an understanding of the various categories for these implants (Table 1). If you can understand your patients’ spectacle-use expectations for the rest of their visual life and how their personality and visual system (their eyes) fit into the categories, you can add any modern-day lens advancement to your practice. Yes, there are other considerations such as the business of refractive cataract surgery, but the most intimidating part of fitting multiple implant options into a practice is “how do I make that final recommendation of what implant to recommend to my patient?”
| Implant Category | Wear Glasses Time | Willingness To Accept Fine Tune | Tear Film Management | Posterior Capsule Haze | Cornea HOAs | Macular Status (Exam & OCT) | Optic Nerve Status (Exam & OCT) | Willingness To Accept Neural Adaptation Time | Informed Consent Additions | |
| Traditional monofocal | All or most of the time | Low | Mild dry eye tolerated | Mild haze tolerated | Less of an issue | Less of an issue | Less of an issue | Not an issue | Absolute presbyopia | |
| Premium monofocal | Mainly for near and sometimes computer | Low | Mild dry eye tolerated | Mild haze tolerated | Less of an issue | Less of an issue | Less of an issue | Not an issue | Less than absolute presbyopia | |
| Traditional monofocal toric | Mainly near unless monovision | High | Mild dry eye tolerated | Mild haze tolerated | Less of an issue | Less of an issue | Less of an issue | Not an issue unless monovision | Absolute presbyopia | |
| Premium monofocal toric | Mainly near unless monovision | High | Mild dry eye tolerated | Mild haze tolerated | Less of an issue | Less of an issue | Less of an issue | Not an issue unless monovision | Less than absolute presbyopia | |
| EDOF | Mainly near | High | Mild dry eye tolerated | Trace haze tolerated (higher YAG rate) | Less of an issue | Mild issue accepted | Mild issue accepted | High | Mild to moderate presbyopia | |
| Light Adjustable Lens | Sometimes near | High | Mild dry eye tolerated | Trace haze tolerated (higher YAG rate) | Less of an issue | Mild issue accepted | Mild issue accepted | Low | Mild presbyopia if mild monovision accepted | |
| Trifocal | Almost never | High | Need normal or fully treated | No haze tolerated (highest YAG rate) | Low | Normal | Normal | High | Reading range of someone in their 30’s |
PATIENT EDUCATION: OUR NATURAL LENS
When patients understand their lens used to be clear for focusing and flexible for reading range — and now it is stiff and cloudy (a cataract) — their face lights up when they realize they have a choice to replace both things they lost — reading range and clarity — or one of the functions they lost — clarity. In general, the patients who choose to replace both functions are seeking spectacle independence for the majority of their functioning, and the patients who choose to replace just the clarity are fine with replacing any residual refractive error and the reading range at near and intermediate in spectacles. But they sure value having a choice.
DISCUSS MODERN OPTIONS
The goal is to minimize the chance of a patient ending up disappointed in their implant vision with a great preoperative education program on modern-day IOL options.
We are diagnosing cataract blur at a younger and younger age. As a result, it is not unusual that some accommodation or pseudo-accommodation is lost when the mild cataract is removed and replaced with a monofocal lens. You should discuss this preoperatively. For example, a 50-year-old with posterior subcapsular cataracts who is functioning with some reading range preoperatively and has a monofocal implant might choose a plano result that results in a reading range of a 70-year-old. This is what we call “absolute presbyopia.” We have seen patients like this present disappointed that they were never offered a modern-day multifocal implant and they want an IOL exchange to have a multifocal placed.
VISION GOALS VS IMPLANT TECHNOLOGY
Whether a practice is just starting to implement modern-day presbyopia-correcting IOLs or is implementing the latest and greatest extended depth of focus (EDOF) or trifocal, the principles are the same: understand your patient and their desires. It helps a great deal when a surgeon understands their patient’s visual goals and matches the technology to those goals.
With so many options, it can be sensory overload for a patient. They relax when you tell them, “My job is to get to know you and learn how you want to use your vision for the rest of your life and then I can advise you on what implant I would recommend for you to achieve those goals ... it is like combining my training, knowledge and experience with your vision goals, expectations and personality.”
A wonderful way to start that conversation after the anatomy talk on their natural lens is to ask a simple but very important question: “Do you want to do a lot with eyeglasses after surgery or a lot without eyeglasses?”
It amazes us how many people we see in consultation who want presbyopia-correcting technology when they learn what their lens used to do and how they now have an opportunity to get back both functions thanks to the modern-day implant technology that the medical device companies, their research and the FDA-approval process have blessed us with.
Note that it is important to keep this a vision-focused outcome discussion as opposed to a technology discussion. Ideally, specific implant technology discussion should be done after learning how the patient wants to use their vision for the rest of their life. Keeping the foundation of your patient education based on this criterion also offers the benefit of making it easier for your practice when adding a new implant technology — because your patient education process changes very little.
Now that you understand your patient and everyone understands the categories of implant options (Table 1), you can match the implant that best suits the “rest of their life” visual goals.
A LONG-TERM PROCESS
If a patient chooses to go down the road of maximizing spectacle independence, it is important to always think in parallel about both the implant that will achieve those goals and the plan for optimizing their vision. The doctor needs to assure the patient that this may involve more than just the cataract surgery itself. It’s a process that requires time and sometimes an additional procedure or two and/or medical optimization if they do not achieve their goals with just the implant surgery.
In a patient who is experiencing blur postoperatively, we like to think of their eye and how we help them by starting in the front and working our way through their visual system. Thus, we are asking ourselves questions and answering them through our exam and diagnostics (Table 2). This methodical thinking from the front of the eye to the back helps us to be sure we have optimized everything for our patient that we can possibly optimize.
| Problem/Issue To Consider | Test | Action |
|---|---|---|
| Residual refractive error | Phoropter manifest refraction by experienced refractionist | AK, PRK, or LASIK fine tune |
| Eye dryness | History of red, irritated eyes, discomfort, slit lamp exam with staining, osmolarity testing, meibography | Artificial tears, topical therapeutics, punctal plugs, MGD therapy |
| Tear film optimized | History of blink-to-blink variability, decreased TBUT, irregularities on tests such as topography and HOA measurements that vary when repeated with a good blink | Artificial tears, topical therapeutics, punctal plugs, MGD therapy |
| Corneal epithelium, stroma | Slit lamp exam, epithelial mapping, corneal topography, corneal HOA testing | If epithelial (anterior basement membrane dystrophy), then a superficial keratectomy with or without PTK |
| Irregular astigmatism scattering light irregularly and degrading the pristine optics of the advanced implant | Gas permeable contact lens over-refraction documenting a good contact fit with no bubble on slit lamp exam followed by a quality refraction by an experienced refractionist | If this test makes the vision crisp, you know that the tear film, epithelium or stroma are creating an irregularity that should be treated |
| Implant position | Is the EDOF or multifocal optic centered? Typically not the issue even if the optic is not centered on the pupil | An implant exchange should be a rarity with modern day technology and an optimized visual system but occasionally is needed |
| Capsule clarity | Slit lamp exam and internal HOA measurements | YAG laser capsulotomy |
| Vitreous clarity | Slit lamp exam with dilated fundus exam | We have seen patients benefit from this greatly after all other aspects of their visual system have been optimized |
| Macula pathology including macular edema | Exam and OCT | Retinal consult and, if necessary, treatment |
| Optic nerve issue | Exam and OCT | Glaucoma consult if necessary |
With regards to residual refractive error — since it is the most common cause of a disappointed patient — from the moment you meet your patient it is important to think about how to optimize their vision if the implant surgery alone does not achieve the level of satisfaction they desire. During the preoperative workup, include preoperative testing, which includes thinking critically about the refractive side of refractive cataract surgery. A refractive cataract surgeon should be thinking about the health of tear film, cornea (epithelium, thickness and stroma) prior to cataract surgery and asserting they have all their tools (astigmatic keratotomy, PRK, LASIK) available to them to enhance the patient’s vision.
With regards to “What level will we enhance?” it is no different than fitting glasses. If a manifest refraction gives them the image quality they are looking for, we often do a surgical enhancement even if it is only 0.50 D of sphere or cylinder. If it is only 0.25 D, you should typically be suspicious that either something else like tear film needs to be treated or the patient needs more healing time and neural adaptation (see below). A surgical treatment of 0.25 D of sphere would be very rare, and cylinder at that level is even more rare. But one of the keys to remember in making patients happy with modern-day premium implants is that if you show your patient their low manifest refraction and it makes their vision better, respect it and realize your work is not done in their vision optimization journey.
SETTING PROPER EXPECTATIONS
This is critical with any surgery and likely one of the most important parts of our job as doctors. When adding a new premium implant to your practice, having a clear story that you repeat to every patient makes the journey much more pleasant for the patient and the surgeon.
Tell all patients who desire optimized spectacle independence that “in addition to this advanced implant, it is important to realize that it is common 3 months after surgery to need to treat any left-over correction from healing, such as astigmatism. It is also common that the capsule can get hazy and you need that lasered. And after we have optimized your vision to as close to zero correction as possible, there is a time period where your brain is getting used to your new optical system that we call ‘neural adaptation.’ Don’t worry if you don’t have everything you are looking for after step one. Consider the first 3-6 months the time of optimizing your new vision and the next 3-6 months as the time your brain needs to get used to your new optical system.”
IOL EDUCATION IS KEY
Going through each step of the patient experience cycle with your team will optimize every step of the patient journey. This includes the education on your website, how your staff talks to the patient, how the technicians understand the importance of their testing, the education and exam performed by you and your other doctors, informed consent, surgical counseling details, financial details and more. By educating yourself and your team, the excitement and confidence in a new implant technology is helped immensely. Also, the patients can feel it, which builds their confidence in your practice.
CONCLUSION
One of the most energizing aspects of a modern-day cataract surgery practice is offering and keeping up with advancements in premium implant technology. The companies have brought us amazing technologies and if you follow the principles outlined in this article, it will help your practice go to the next level with confidence and joy. OM









