The COVID pandemic caused every practice to re-examine its workflows around the most basic elements of patient care. With limited staff who were often less than fully trained, it became essential to create efficiencies. These staffing challenges continue in the post-pandemic world, as does the need to create revenue and time efficiency for every condition we treat. The pandemic also helped us understand the value of digital systems that can replace time-consuming human interaction.
Yet another trend that grew during the pandemic was dry eye disease (DED). Spending more time on-screens, eating a less healthy diet and being less active took their toll. Even asymptomatic patients became symptomatic. And mask-associated dry eye became a new clinical entity.
Dry eye has long been the bane of many clinicians’ practice. A market research study by TearScience several years ago showed that practitioners on average spend approximately 10% of their time treating ocular surface disease but earn only 2% of their revenue from the same range of conditions. That’s because collecting a proper history for dry eye and educating patients properly about various treatment options has — until recently — depended exclusively on time-consuming human interaction.
In the past, the only clinicians who might develop a “dry eye center of excellence” were those who took a personal interest in this disease. With automation and digital tools to assist in patient interaction, however, doctors can greatly reduce their time spent collecting histories and educating patients and spend more time on clinical decision making — which is far more gratifying.
DED TECHNOLOGY WISH LIST
As Darrell White, MD, an ophthalmologist at SkyVision Centers in Cleveland, says, “Any time you can automate a process that is integral to a standard care protocol, you instantly increase the quality of care you are rendering. In the case of DED, having a standard questionnaire response on hand for each visit, but especially the initial visit, improves our ability to measure our results for an individual patient and our results across patient groups. If the process is automated and completed before a patient arrives, we remove the effects of a particular office day’s level of business/chaos on our performance of this step.”
An ideal digital tool to assist in treating dry eye:
- Works automatically, without significant staff or physician input
- Thoroughly collects patient history and presents it in a concise manner
- Assists in educating patients both before after the visit
- Follows up on their progress to ensure treatment success.
- Allows us to aggregate data on which treatments work best for which types of patients, giving doctors real feedback and potentially publishable data.
SOFTWARE FOR DED PLUS
MDbackline is a tool I designed that not only streamlines dry-eye treatment but boosts adoption of premium IOLs and streamlines other workflows related to patient interaction. The system is a secure, web-based software that links to the EMR or practice management system to detect upcoming appointments for patients with ocular surface problems. (The same workflow also serves cataract patients, those with glaucoma, macular degeneration and other diseases.) Prior to the appointment, it contacts patients via text or email using the name and picture of the doctor and invites them to click the website link, briefly verify their identity and answer questions related to their upcoming appointment.
DRY EYE APPLICATIONS
In the case of dry eye, it takes about 3 minutes to complete the questions, which range from describing symptoms to listing background conditions and medications related to dry eye. While brief, the questionnaire, which has extensive branching logic to save patients time, collects a detailed history related to ocular surface disease based on the preferred practice patterns of some of the country’s leading dry-eye practitioners.
The dry eye pre-consultation module also educates patients broadly and without using brand names of the treatment options offered by the practice, including premium DED procedures and offerings. This way, patients arrive at the office having some background understanding on the treatment options they may be offered.
EVERYTHING THE PHYSICIAN NEEDS TO KNOW
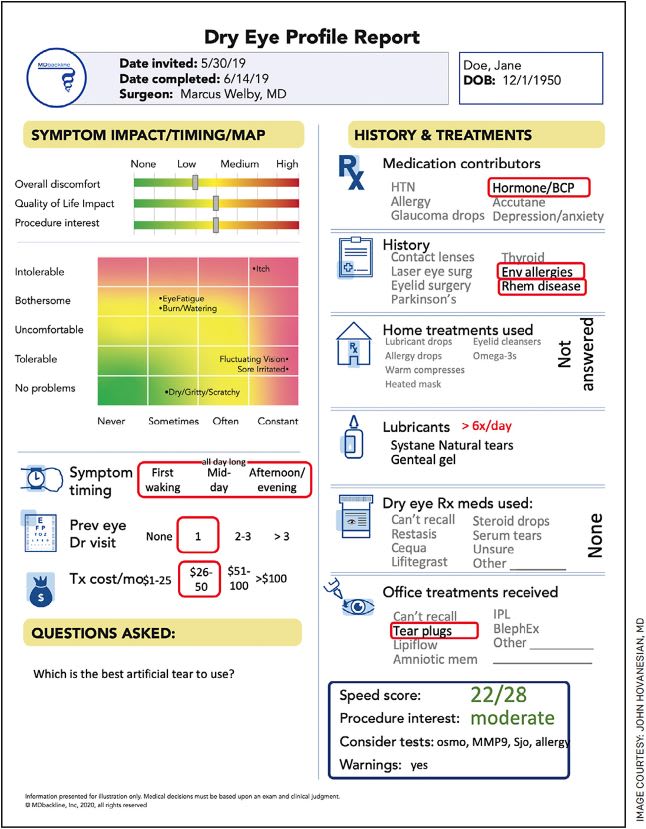
To convey all this complex information to the practitioner, a concise, colorful Visual Profile Report (VPR) presents a one-page depiction of all the patient’s history, including symptoms, with severity and frequency separately reported, SPEED (standard patient evaluation of eye dryness) score, relevant medical history, dry eye treatments being used, lifestyle impact and a summary of the patient’s likelihood to elect a premium procedure or treatment (Figure). The average clinician takes about 15 seconds to review all this information — a process that used to take many minutes in verbal history collection. For about 80% of patients, many clinicians feel prepared to offer a treatment option even before an examination is performed.
“It saves time not to have patients complete a questionnaire in the office, which can take up to 10 minutes,” says Alice Epitropoulos, MD, a dry eye specialist in Columbus, Ohio. “I really like the efficiency created by already knowing the SPEED score and what treatments patients have already tried. I can have a plan in mind before stepping into the lane.”
In the exam room, clinicians can explain to patients a summary of the symptoms they reported on the visual profile report. For patients, this is highly gratifying to meet a doctor who cares enough about their condition to collect a detailed history and then have internalized it and repeated it to the patient to make sure it has been well understood.
BEYOND THE EXAM ROOM
Following the visit, MDbackline contacts the patient via text or email to ask how satisfied they are with treatment and which treatments are actually being used then determines whether a follow-up visit is needed. This is reported to the practice in a simple-to-read format categorized as red, yellow or green based on whether the patient is continuing to have significant problems, progressing or doing well. These reports are, recorded in the EMR system — in many cases automatically.
Long-term care of dry eye patients can evolve, comparing SPEED scores and other symptom reports over time. MDbackline can report in aggregate format on how all of a doctor’s patients respond to similar questionnaires. This has already allowed a number of published studies to examine the effectiveness of various treatment options. At the very least, it helps doctors understand which of their treatments work best.
MDbackline has similar functions for glaucoma patients, exploring side effects of eyedrops, ascertaining interest in surgical options and reporting on their cost, compliance and overall sentiment about their topical drop therapy. In cataract, the software collects a patient’s visual complaints, lifestyle and visual desires and reports on the likelihood of a patient to choose a premium lens implant during surgery. In each case, the software allows automated collection of highly detailed and relevant information while reducing person-to-person contact — a highly desirable combination in a world still recovering from the coronavirus pandemic. OM
Disclosure: Drs. White and Epitropoulos have no financial interest in MDbackline.









