When preparing to perform cataract surgery in a keratoconus patient, there are several considerations that need to be taken into account. Most of these are refractive in nature, as the cataract procedure itself bears very little difference than a non-keratoconic eye.
It is tempting to try to correct in known keratoconus patients the cylinder in the refractive error with a toric IOL in order to enhance their uncorrected visual rehabilitation to the maximum. But there are several considerations that need to be taken.
SCREENING CATARACT PATIENTS
Testing
We estimate that one out of 20 people, including those we perform cataract surgery on, have keratoconus. This number includes mild subclinical cases that have never been diagnosed before — doing so prior to cataract surgery may enhance a patient’s refractive outcome!
Keratoconus appears to be endemic in countries like Greece, where I practice full time — a stark difference compared to the patients I encounter and operate on in New York City, where keratoconus is usually reported in one in 500 to 2,000 patients. Of course, this data represents older clinical paradigms when corneal imaging was not as popular and readily available in most clinical settings. I am sure that keratoconus “suspicious” corneas, even in the United States, will be surprisingly higher than most clinicians expect. So, as a precaution, we screen all of our cataract population — especially at the time of planning to undergo cataract surgery — with Scheimpflug tomography (ie, the Pentacam (Oculus)) to test for keratoconus. This is extremely important, in my opinion, because it helps to avoid the postoperative surprise of pseudophakia that does not reach an uncorrected or best-corrected visual acuity at the level that we had planned and hoped for and both we and our patients desire.
Contact lens use
An initial important parameter to consider is whether a keratoconic patient planning to undergo cataract surgery is a rigid gas permeable (RGP) lens or scleral lens wearer. This poses a special consideration since a decision, after careful discussion with the patient, yields whether the patient will continue to wear RGP or scleral lenses after the cataract procedure or prefer to avoid that. After a toric IOL is implanted, if a patient desires to go back to a RGP and/or scleral lens, then they must wear over the contact lenses, a spectacle correction that neutralizes the power of astigmatism present in the Toric IOL that has been implanted.
In general, patients who can only function with RGP or scleral lenses and desire to do so after their cataract procedure are probably best treated with a simple, non-toric, monofocal lens. They can continue to wear those lenses as they are already comfortable with them while also enjoying improved visual acuity.
IOL calculations and considerations
In my experience, most patients desire to explore the possibility of correcting not only their invariable myopia (keratoconic eyes are usually myopic and with deeper anterior chamber), but also astigmatism with the use of a toric IOL during cataract surgery. The IOL calculation is quite complicated due to variability of keratometries that can be registered in keratoconus, especially if the cone is oblique (which is the most common kind — 80% of cases). We have to consider that the interferometry device readings that we use to calculate IOLs assess the 2.8-mm to 3.2-mm anterior central corneal keratometry (along with axial length).
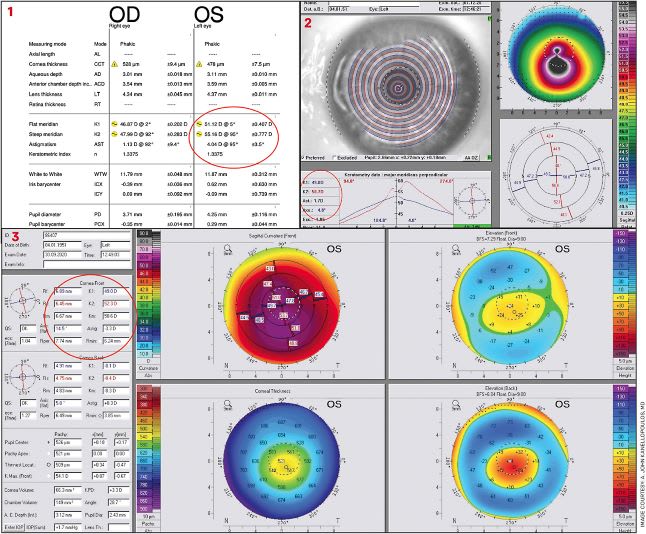
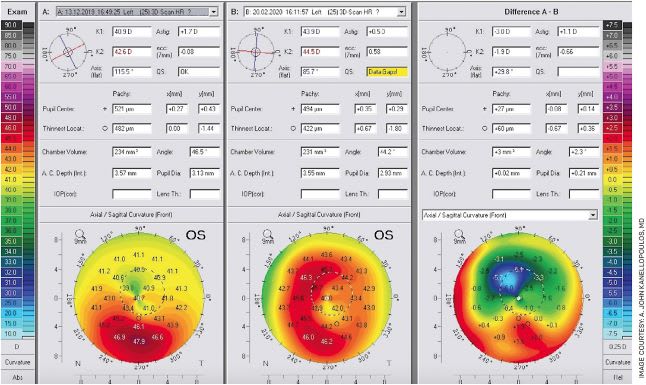
We have come to find the 5-mm total cornea (anterior plus posterior) keratometries and axis from a Pentacam that calculates the anterior and posterior cornea power altogether is probably the most accurate (Figures 1-3). In our practice, the “go-to” IOL formula for keratoconus is the Holladay 1. This is due to the invariably large axial length, which is more importantly combined with an invariably larger than usual anterior chamber depth in these eyes, as we have recently reported in the European and the American meetings (European Society of Cataract and Refractive Surgeons, ASCRS and AAO). Our study is currently under review for publication.
As the majority of our patients in Athens are intolerant to contact lenses, 95% of our cataract patients enjoy the options of a T2 to T9 range of toric IOL correction. Our go-to IOL is the AcrySof IQ Toric IOL (Alcon) with range of inclusive cylinder as noted above from 1 D to 6 D — a shorter range of toricity is approved and available in the United States.
As mentioned previously, we use the Holladay 1 formula and the keratometries and axis from a 5-mm total cornea power from a Pentacam measurement, and we found that visual correction has been very rewarding in these patients. We are cautious, however, in adding pilocarpine drops despite intraoperative acetylcholine to attain miosis because of the hovering danger of Urrets-Zavalia Syndrome of a permanently dilated pupil that can be associated with an intraocular procedure in keratoconus patients.
The last consideration is that if a femtosecond laser will be used to enhance the cataract procedure, the clinician needs to carefully screen for any corneal opacities (common at the peak of advanced cones) that may interfere with the optical clarity needed for the femto-assisted procedure
KERATOCONUS TREATMENT
The Athens Protocol
Normalizing the cornea optics with the Athens Protocol corneal cross-linking (CXL) procedure (which we introduced in 2005) can be viewed as a prequel to a cataract procedure, as it will drastically improve the visual function and likely the spectacle-free lifestyle.
For many years, we have advocated that CXL can become far more effective when combined with a minimal-in-thickness topographic-guided photorefractive keratectomy (PRK) procedure. That needs to be viewed more as a phototherapeutic keratectomy (PTK) procedure aiming to reduce the cornea refractive coma induced by the corneal ectasia. We have named this CXL procedure the Athens Protocol. Since introducing this procedure, we have reported close to 50 peer-reviewed papers and more than 1,000 eyes very carefully studied, some of them recently, with 10 years follow up, establishing the safety and efficacy of this technique.1-50
Of course, this approach makes more sense when attempting to visually rehabilitate patients in an environment where rigid contact lenses and scleral lenses are very difficult to tolerate, such as in southern Europe.
So, for us, this approach usually includes besides the topography-guided normalization, the refractive treatment of 1.0-2.0 D of astigmatism and 1.0 to 2.0 D of myopia — most of the time only a fraction of the actual refractive errors that the patients have strictly on the topography-defined astigmatic axis and not the manifest refraction axis. The advantage of combining this partial in refraction, topography-guided PRK of maximum 50 μm ablation at the minimum thickness of the cornea is that it appears to achieve unique robust synergy with the CXL procedure (We have used accelerated fluence of 6mW/cm2 in exposure of 15 minutes to deliver the same amount of energy with the FDA-approved classic Dresden protocol, which uses 3mW/cm2 for exposure of 30 minutes.) (Figure 4).
We have found that this fluence offers the best cross-linking effect in these patients as it achieves the deepest cross-linking line studied with anterior segment optical coherence tomography (OCT); it reaches more than 60% of the total cornea thickness and, with the Athens protocol, appears to be very uniform in depth throughout the 9 mm of cornea that usually are started with this technology (Avanti, Optovue) (Figure 5).
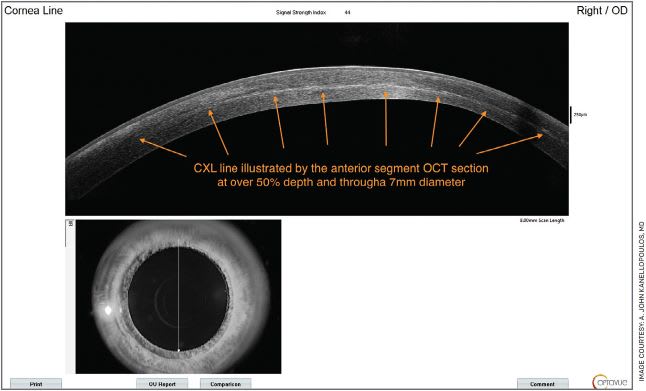
This is in great contrast to a classic standalone CXL procedure that usually achieves a more in-depth cross-linking effect centrally and less peripherally. This is the reason why the cross-linking — combined with the partial-in-refractive error corrected minimal thickness PRK — is able to invariably achieve 5.0 D to 15.0 D of flattening, where the laser alone would achieve maximum 1.0 D or 2.0 D of flattening. CXL as a standalone procedure usually achieves the same 1.0 D to 2.0 D of flattening.
This greater flattening achieved in these patients at the peak of their cone or their ectasia underlines the previously noted synergistic effect of using both procedures together. We have theorized that this probably happens for two reasons. First, the larger riboflavin molecule better penetrates a cornea that has been partially ablated in its surface. In addition, UV light is able to better penetrate the cornea and achieve a better cross-linking effect, thus offering a more stable and dramatically reduced steepest keratometry.
Cross-linking rather than stabilizing oaths
We have also applied this procedure in the United States since topography-guided ablations became FDA-approved in 2013, and CXL later became approved as well. It is an off-label combined procedure and needs to be consented with patients appropriately, but our US experience has been very rewarding.
A large number of US surgeons, especially cornea specialists, are very familiar with specialized cornea work with the excimer laser and keratoconus management. They have been able to duplicate these results and offer the benefits of employing the Athens Protocol in US patients as well. When used with caution, this procedure can become a great tool to add stability and to dramatically visually rehabilitate these patients. It should, nevertheless, not be viewed as a pure refractive procedure.
Discussing the refractive target with patients
The Athens Protocol CXL may be a pre-cataract surgery step to consider with advanced keratoconus patients, as it may enable them to approach emmetropia following a cataract procedure several months later and after their corneas have been significantly normalized. It makes cataract surgery a longer path, but some patients may be interested in this approach. We have used the vast experience accumulated from mostly younger keratoconus patients that are commonly treated with the Athens Protocol CXL.
Evaluating a family for keratoconus
This work has also made us very astute of carefully investigating possible subclinical keratoconus. We like to evaluate the whole family — and we have presented a 100% yield of finding one of the two parents of a known keratoconic young patient having a trait of keratoconus. This becomes valuable for us to evaluate the other young adults in that family. A thorough ophthalmic evaluation to rule out keratoconus can never exclude a cornea topography or tomography. A 20/20 patient with perfect corneas in slit-lamp biomicroscopy may still harbor an obvious keratoconus when cornea topography or tomography is employed, and it is even more accurate when anterior segment OCT is employed that can also offer a 3D image of the cornea epithelium that may mask the actual expression of ectasia in early stages. We have reported extensively on this in both meetings and in the peer-reviewed literature.
A cataract surgery candidate likewise having a grandchild with known keratoconus raises the suspicion for closer evaluation of subclinical irregular topography that may aid in a better refractive outcome in their cataract surgery.
Integrating laser work
Although there are currently many venues of employing CXL, such as epithelium-on (sufficient to stabilize the keratoconus short term), it has shown in our hands and in the literature that it is not as robust as the standard epithelium-off cross-linking.
Iontophoresis to deliver the large riboflavin molecule transepithelially into the cornea was very popular a little more than 5 years ago, but it is fading away as a popular clinical option, as other techniques appear to be as effective and simpler.
Since 2013 we have also introduced — in collaboration with Avedro (now part of Glaukos) — advanced UV projection technology (the KXL II device CE marked in 2013, later named Mosaic) that can allow us to use a pattern of different fluence and energy delivered into the cornea to attain reproducible refractive changes in keratoconic and even normal corneas.
Ray tracing excimer customization
We recently reported in Cornea the use of ray tracing as a means of measuring total eye aberrations (low and high) in combination with CXL. This means using a ray-tracing customized ablation instead of a topography-guided partial refraction excimer laser ablation and higher fluence cross-linking. This employs data from the Sitemap device, an adapted Pentacam AXL Wave (offering HR Pentacam, Lenstar interferometry and Hartmann-Shack wavefront measurements along with pupillometry and limbal and iris recognition landmarks) and the Innoveyes software (WaveLight, Alcon), which is undergoing FDA trial in the United States and was CE-marked in Europe in 2019.
Ray tracing offers the attractive option of measuring total eye aberrations in a keratoconic or an ectasia patient, in normalizing the cornea and treating some of the higher aberrations as well, in combination with CXL. On a practical level, ray tracing appears to view the ectatic corneas and tilted cornea, thus normalizing that cornea with treating mainly a superior cornea hyperopic arc. This approach helps to avoid treatment in the very debatable area of the thinnest part of the cornea, which is the area of the steepest part of the cone.51-52
This is a new, exciting frontier in the treatment of keratoconus. Ray-tracing customization in therapeutic excimer ablations used in keratoconus management may become an application used by more clinicians globally and help establish whether this will be more beneficial than the topography-guided ablation, which has become the standard of care when trying to not only stabilize the cornea but also improve visual function globally and within the United States. OM
REFERENCES
- Kanellopoulos AJ. Post-LASIK ectasia. Ophthalmology. 2007;114(6):1230.
- Hafezi F, Kanellopoulos J, Wiltfang R, Seiler T. Corneal collagen crosslinking with riboflavin and ultraviolet A to treat induced keratectasia after laser in situ keratomileusis. J Cataract Refract Surg. 2007;33(12):2035-2040.
- Kanellopoulos AJ, Binder PS. Collagen cross-linking (CCL) with sequential topography-guided PRK: a temporizing alternative for keratoconus to penetrating keratoplasty. Cornea. 2007;26(7):891-895.
- Kanellopoulos AJ. Comparison of sequential vs same-day simultaneous collagen cross-linking and topography-guided PRK for treatment of keratoconus. J Refract Surg. 2009;25(9):S812-S818.
- Kanellopoulos AJ. Collagen cross-linking in early keratoconus with riboflavin in a femtosecond laser-created pocket: initial clinical results. J Refract Surg. 2009;25(11):1034-1037.
- Krueger RR, Kanellopoulos AJ. Stability of simultaneous topography-guided photorefractive keratectomy and riboflavin/UVA cross-linking for progressive keratoconus: case reports. J Refract Surg. 2010;26(10):S827-S832.
- Kanellopoulos AJ, Skouteris VS. Secondary ectasia due to forceps injury at childbirth: management with combined topography-guided partial PRK and collagen cross-linking (Athens Protocol) and subsequent phakic IOL implantation. J Refract Surg. 2011;27(9):635-636.
- Kanellopoulos AJ, Binder PS. Management of corneal ectasia after LASIK with combined, same-day, topography-guided partial transepithelial PRK and collagen cross-linking: the athens protocol. J Refract Surg. 2011;27(5):323-331.
- Kanellopoulos AJ. Long term results of a prospective randomized bilateral eye comparison trial of higher fluence, shorter duration ultraviolet A radiation, and riboflavin collagen cross linking for progressive keratoconus. Clin Ophthalmol. 2012;6:97-101.
- Kanellopoulos AJ. The management of cornea blindness from severe corneal scarring, with the Athens Protocol (transepithelial topography-guided PRK therapeutic remodeling, combined with same-day, collagen cross-linking). Clin Ophthalmol. 2012;6:87-90.
- Kanellopoulos AJ. Laboratory evaluation of selective in situ refractive cornea collagen shrinkage with continuous wave infrared laser combined with transepithelial collagen cross-linking: a novel refractive procedure. Clin Ophthalmol. 2012;6:645-652.
- Kanellopoulos AJ, Asimellis G. Comparison of Placido disc and Scheimpflug image-derived topography-guided excimer laser surface normalization combined with higher fluence CXL: the Athens Protocol, in progressive keratoconus. Clin Ophthalmol. 2013;7:1385-1396.
- Kanellopoulos AJ, Moustou V, Asimellis G: Evaluation of visual acuity, pachymetry and anterior-surface irregularity in keratoconus and crosslinking intervention follow-up in 737 cases. J Kerat Ect Cor Dis. 2013;2(3):95-103.
- Kanellopoulos AJ, Asimellis G. Keratoconus management: long-term stability of topography-guided normalization combined with high-fluence CXL stabilization (the Athens Protocol). J Refract Surg. 2014;30(2):88-93.
- Kanellopoulos AJ. Novel myopic refractive correction with transepithelial very high-fluence collagen cross-linking applied in a customized pattern: early clinical results of a feasibility study. Clin Ophthalmol. 2014;8:697-702. Published Apr 7, 2014.
- Kanellopoulos AJ, Asimellis G. Corneal refractive power and symmetry changes following normalization of ectasias treated with partial topography-guided PTK combined with higher-fluence CXL (the Athens Protocol). J Refract Surg. 2014;30(5):342-346.
- Kanellopoulos AJ, Dupps WJ, Seven I, Asimellis G. Toric topographically customized transepithelial, pulsed, very high-fluence, higher energy and higher riboflavin concentration collagen cross-linking in keratoconus. Case Rep Ophthalmol. 2014;5(2):172-180. Published June 18, 2014.
- Kanellopoulos AJ, Asimellis G. Epithelial remodeling after partial topography-guided normalization and high-fluence short-duration crosslinking (Athens protocol): results up to 1 year. J Cataract Refract Surg. 2014;40(10):1597-1602.
- Kanellopoulos AJ, Krueger RR, Asimellis G. Cross-linking and corneal imaging advances. Biomed Res Int. 2015;2015:306439.
- Kanellopoulos AJ, Loukas YL, Asimellis G. Cross-Linking Biomechanical Effect in Human Corneas by Same Energy, Different UV-A Fluence: An Enzymatic Digestion Comparative Evaluation. Cornea. 2016;35(4):557-561.
- Kanellopoulos AJ, Asimellis G. Novel Placido-derived Topography-guided Excimer Corneal Normalization With Cyclorotation Adjustment: Enhanced Athens Protocol for Keratoconus. J Refract Surg. 2015;31(11):768-773.
- Kanellopoulos AJ. Topography-guided hyperopic and hyperopic astigmatism femtosecond laser-assisted LASIK: long-term experience with the 400 Hz eye-Q excimer platform. Clin Ophthalmol. 2012;6:895-901.
- Kanellopoulos AJ. Long-term safety and efficacy follow-up of prophylactic higher fluence collagen cross-linking in high myopic laser-assisted in situ keratomileusis. Clin Ophthalmol. 2012;6:1125-1130.
- Kanellopoulos AJ, Kahn J. Topography-guided hyperopic LASIK with and without high irradiance collagen cross-linking: initial comparative clinical findings in a contralateral eye study of 34 consecutive patients. J Refract Surg. 2012;28(11 Suppl):S837-S840.
- Kanellopoulos AJ. Very high fluence collagen cross-linking as a refractive enhancement of a regressed previous astigmatic keratotomy. J Refract Surg. 2013;29(7):504-505.
- Kanellopoulos AJ, Asimellis G. Refractive and keratometric stability in high myopic LASIK with high-frequency femtosecond and excimer lasers. J Refract Surg. 2013;29(12):832-837.
- Kanellopoulos AJ, Pamel GJ. Review of current indications for combined very high fluence collagen cross-linking and laser in situ keratomileusis surgery. Indian J Ophthalmol. 2013;61(8):430-432.
- Kanellopoulos AJ, Asimellis G. Epithelial remodeling after femtosecond laser-assisted high myopic LASIK: comparison of stand-alone with LASIK combined with prophylactic high-fluence cross-linking. Cornea. 2014;33(5):463-469.
- Kanellopoulos AJ, Asimellis G. Longitudinal postoperative lasik epithelial thickness profile changes in correlation with degree of myopia correction. J Refract Surg. 2014;30(3):166-171.
- Kanellopoulos AJ, Chiridou M, Asimellis G. Optical coherence tomography-derived corneal thickness asymmetry indices: clinical reference study of normal eyes. J Cataract Refract Surg. 2014;40(10):1603-1609.
- Kanellopoulos AJ, Asimellis G. Clinical Correlation between Placido, Scheimpflug and LED Color Reflection Topographies in Imaging of a Scarred Cornea. Case Rep Ophthalmol. 2014;5(3):311-317. Published Oct 1, 2014.
- Kanellopoulos AJ, Asimellis G. Clear-cornea cataract surgery: pupil size and shape changes, along with anterior chamber volume and depth changes. A Scheimpflug imaging study. Clin Ophthalmol. 2014;8:2141-2150. Published Oct 24, 2014.
- Kanellopoulos AJ, Asimellis G. OCT-derived comparison of corneal thickness distribution and asymmetry differences between normal and keratoconic eyes. Cornea. 2014;33(12):1274-1281.
- Kanellopoulos AJ, Asimellis G. OCT corneal epithelial topographic asymmetry as a sensitive diagnostic tool for early and advancing keratoconus. Clin Ophthalmol. 2014;8:2277-2287. Published Nov 18, 2014.
- Kanellopoulos AJ, Asimellis G, Karabatsas C. Comparison of prophylactic higher fluence corneal cross-linking to control, in myopic LASIK, one year results. Clin Ophthalmol. 2014;8:2373-2381. Published 2014 Nov 27.
- Kanellopoulos AJ, Asimellis G. Hyperopic correction: clinical validation with epithelium-on and epithelium-off protocols, using variable fluence and topographically customized collagen corneal crosslinking. Clin Ophthalmol. 2014;8:2425-2433. Published Dec 2, 2014.
- Kanellopoulos AJ. Reporting acuity outcomes and refractive accuracy after LASIK. J Refract Surg. 2014;30(12):798-799.
- Kanellopoulos AJ, Asimellis G: Rate of change of curvature of the corneal stromal surface drives epithetlial compensatory changes and remodeling: Reply. J Refract Surg 2014 Dec; 30(12):800-05.
- Kanellopoulos AJ, Kontos MA, Chen S, Asimellis G. Corneal collagen cross-linking combined with simulation of femtosecond laser-assisted refractive lens extraction: an ex vivo biomechanical effect evaluation. Cornea. 2015;34(5):550-556.
- Kanellopoulos AJ, Asimellis G, Salvador-Culla B, Chodosh J, Ciolino JB. High-irradiance CXL combined with myopic LASIK: flap and residual stroma biomechanical properties studied ex-vivo. Br J Ophthalmol. 2015;99(6):870-874.
- Kanellopoulos AJ, Asimellis G. Combined laser in situ keratomileusis and prophylactic high-fluence corneal collagen crosslinking for high myopia: two-year safety and efficacy. J Cataract Refract Surg. 2015;41(7):1426-1433.
- Kanellopoulos AJ. Topography-modified refraction (TMR): adjustment of treated cylinder amount and axis to the topography versus standard clinical refraction in myopic topography-guided LASIK. Clin Ophthalmol. 2016;10:2213-2221. Published Nov 3, 2016.
- Li N, Peng XJ, Fan ZJ. Progress of corneal collagen cross-linking combined with refractive surgery. Int J Ophthalmol. 2014;7(1):157-162. Published Feb 18, 2014.
- Kanellopoulos AJ. Ten-Year Outcomes of Progressive Keratoconus Management With the Athens Protocol (Topography-Guided Partial-Refraction PRK Combined With CXL). J Refract Surg. 2019;35(8):478-483.
- Kanellopoulos AJ, Vingopoulos F, Sideri AM. Long-Term Stability With the Athens Protocol (Topography-Guided Partial PRK Combined With Cross-Linking) in Pediatric Patients With Keratoconus. Cornea. 2019;38(8):1049-1057.
- Stojanovic A, Zhang J, Chen X, Nitter TA, Chen S, Wang Q. Topography-guided transepithelial surface ablation followed by corneal collagen cross-linking performed in a single combined procedure for the treatment of keratoconus and pellucid marginal degeneration. J Refract Surg. 2010;26(2):145-152.
- Tamayo GE, Castell C, Vargas P, Polania E, Tamayo J. High-resolution wavefront-guided surface ablation with corneal cross-linking in ectatic corneas: a pilot study. Clin Ophthalmol. 2017;11:1777-1783. Published 2017 Oct 3.
- Gore DM, Leucci MT, Anand V, Fernandez-Vega Cueto L, Arba Mosquera S, Allan BD. Combined wavefront-guided transepithelial photorefractive keratectomy and corneal crosslinking for visual rehabilitation in moderate keratoconus. J Cataract Refract Surg. 2018;44(5):571-580.
- Kanellopoulos AJ: Novel Intraocular lens power calculation in keratoconus using a topography-guided ablation simulation. Presented as a paper at the 2021 AAO meeting in New Orleans, LA, November 2021
- Camellin M, Guidotti JM, Arba Mosquera S. Corneal-Wavefront guided transepithelial photorefractive keratectomy after corneal collagen cross linking in keratoconus. J Optom. 2017;10(1):52-62.
- Mrochen M, Bueeler M, Donitzky C, Seiler T. Optical ray tracing for the calculation of optimized corneal ablation profiles in refractive treatment planning. J Refract Surg. 2008;24(4):S446-S451.
- Kanellopoulos AJ. Initial Outcomes with Customized Myopic LASIK, Guided by Automated Ray Tracing Optimization: A Novel Technique. Clin Ophthalmol. 2020;14:3955-3963. Published Nov 17, 2020.
- Kanellopoulos AJ. Keratoconus Management With Customized Photorefractive Keratectomy by Artificial Intelligence Ray-Tracing Optimization Combined With Higher Fluence Corneal Crosslinking: The Ray-Tracing Athens Protocol. Cornea. 2021;40(9):1181-1187.









