Premium lenses are a phenomenal option for patients who wish to have spectacle independence. Likewise, they are a source of great satisfaction for surgeons involved in refractive cataract surgery. In spite of their remarkable potential benefit, however, it is puzzling to see the relatively low growth of premium IOL adoption. Surgeons often dwell on cases that do not go according to plan, then become a little gun-shy.
Rather than concentrate on how to manage patients when things do not go right, it is far better to avoid troubles in the first place. I have been involved in refractive surgery for more than 30 years, and perfect refractive and visual outcomes have always been a driver, first with radial keratotomy then graduating to laser eye surgery, cataract surgery, lens replacement and corneal transplantation. I have used premium lenses since 2002 and have a premium lens rate (mainly trifocals) of more than 95% of all cataract and refractive lens procedures over the last 10 years. We have performed in excess of 8,000 trifocal lens implants with a zero explantation rate. This rate makes many colleagues wonder if we are stretching the truth, but we are not alone with this success as many colleagues in Europe have similar statistics.
How do we accomplish this rate and maintain a high level of satisfaction? In this article, I hope to provide you with some of the most important pearls to achieving a successful high level premium practice.
SETTING EXPECTATIONS
As a fellow to Dr. Richard Lindstrom in 1991, I recall his comment about happy patients and have always kept this in mind: Patient satisfaction = patient outcome – patient expectation. As an organization, we set high standards in terms of patient outcomes. And while patients naturally have high expectations, we temper these to be realistic, even underselling what can be achieved.
At every point of contact, we make clear to our patients that we expect to provide them with a reduction in dependency on glasses, preferably none at all. This is reflected in our literature, website, communication with our enquiries team, and during the evaluation and consultation process. We make it clear that they must be suitable, which depends on the results of myriad tests as well as the evaluation by the operating surgeon. If they are deemed suitable candidates, we offer them premium lenses. Examples of patients who are not suitable include those with a poor ocular surface, asymmetric aberrations, glaucoma with visual field changes, diabetes and macular degeneration.
We also keep things simple and offer trifocal lenses — in other words, good vision at all distances — as the gold standard. We do not discuss many lens options at this time, because we find doing so confuses patients and makes them anxious and indecisive. Also, we do not promote some of the poor terminology used, such as extended depth of focus (EDOF), and have worked towards revising this terminology at AECOS Europe.1
My philosophy is that patients come to us and trust that we will get them where they want to be. We make the choice based on their needs, desires, activities and expectations. Of course, our discussions include some of the transient issues, like adaptation and halos, and we do not mince words explaining that they are in for the long haul and there is a subgroup of patients that will take a while to adapt. Our job is to optimise their outcome (good refractive correction) so that they are in an optimal position to adapt. For instance, leaving a patient with a residual astigmatic error of more than 0.75 D will not permit good vision and successful adaptation, and it is best to correct this at the time of surgery or without delay when stable if present postoperatively.
PRE-CONSULTATION
During the pre-consultation process, our team does an excellent job of quizzing patients using a checklist and considering their suitability based on age, refractive error, medical conditions, expectations and overall wellbeing. Patients also fill out a “Your information” sheet very much like any other practice, which includes questions derived from Dr. Steven Dell’s clever questionnaire.2 Should they have any relative contraindications (like dry eye, glaucoma or medical conditions), patients are advised beforehand so that this is not a surprise or distraction at consultation. They also receive an information pack along with links to informational videos on trifocal lenses reinforcing the gold standard at our centre.
TESTING
Patients are provided with a consent form for trifocal lenses and urged to read this while waiting between testing and asked to generate questions for the consulting surgeon. The usual battery of tests performed include unaided vision at distance, 40 cm, 60 cm and 80 cm as a base line. We also perform contrast sensitivity testing, IOP and perform retinal imaging (widefield and maculae). Our testing includes:
- OPD-Scan III (Nidek). We perform this on every patient. The “Daya overview” that we developed with Nidek contains considerable information (Figure) on a single page for each eye, including Placido corneal topography, overall aberrometry, derived internal aberrometry, autorefraction and keratometry as well as average pupil power along with surface regularity and asymmetry indices, Q and e values, corneal and internal contributions of spherical aberration and coma as well as point spread function (PSF). Additionally, aberrometry-derived magnitude of corneal and internal cylinder is provided and very useful in considering the magnitude and axis of correction required.3,4 This information allows us to figure out patient suitability for premium lenses and any necessary further investigations, some of which I have listed below.
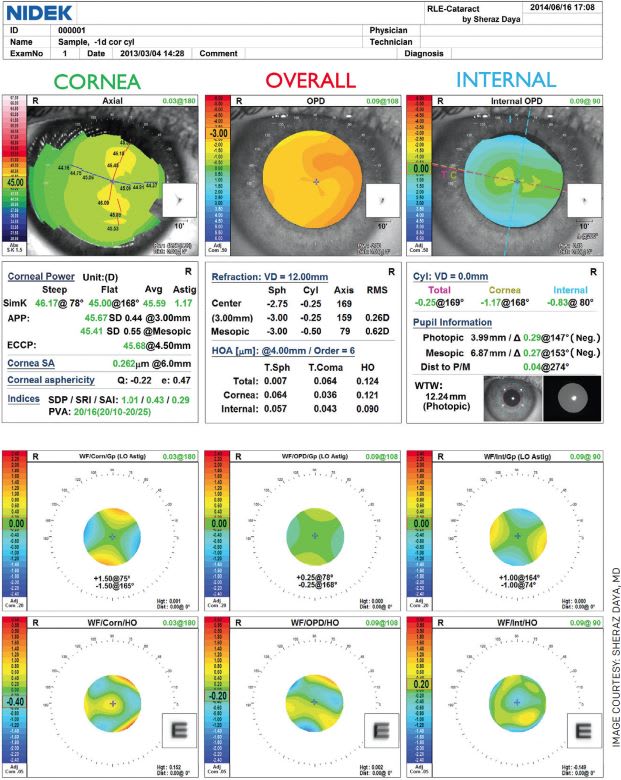
Figure. OPD-Scan III (Nidek) Daya overview - Lens calculations. We use the IOLMaster (Zeiss) to derive lens calculations. Although the Barrett formula has been demonstrated to be the better lens calculation method,5 we have found the Holladay 2 formula works best in our hands.
- Pentacam HD (Oculus). For those with more than 1.00 D of corneal astigmatism on OPD-Scan III, we perform Pentacam to substantiate the magnitude of astigmatism. Although some excellent reports have demonstrated the value of looking at posterior astigmatism,6 we do not pay much attention to this as the magnitude is small and makes calculations more complex with little if any benefit. With newer additions to lens calculation devices, the process is being made simpler and may become the gold standard in time.
- HD Analyzer (Visiometrics). We perform this on every patient in whom we plan lens surgery and pay special attention to the tear film information in those who have an abnormal surface regularity index or PSF on OPD-Scan III. The ocular scatter index (OSI) provides us with information regarding the overall ocular performance of each eye, which is influenced by the tear film, lens opacity and, in some cases, the vitreous. Tear film stability can be determined objectively and is useful to show patients if they need preoperative care with regards to underlying meibomian gland disease (Omega 3 supplements and intense pulsed light). The device also images meibomian glands, though we hardly use this feature. The presence of a good tear film and a poor OSI suggests an internal optical issue and a “dysfunctional” lens, and often substantiates the benefit of undergoing lens replacement rather than any other refractive procedure.
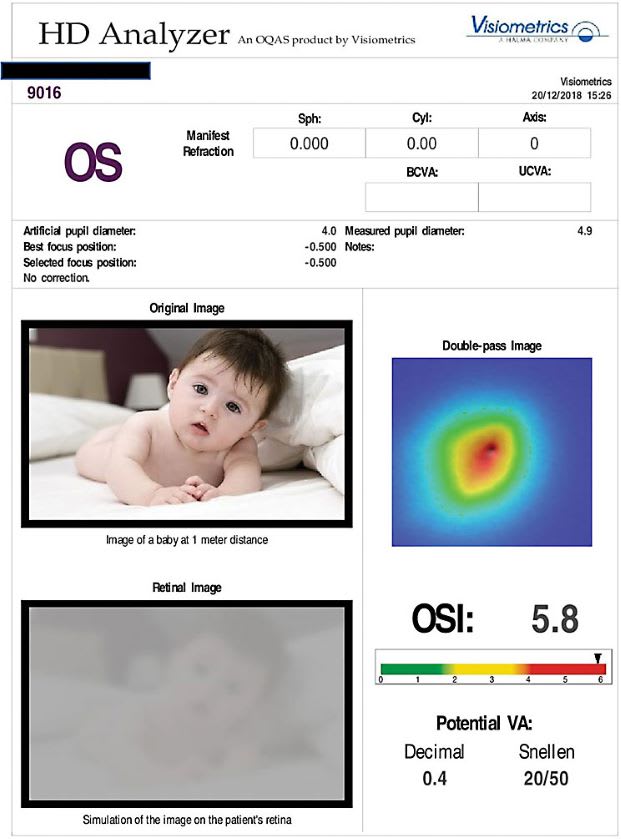
Figure 2a 
Figure 2b - Anterion (Heidelberg)/Advanced Corneal Explorer (ACE, Bausch + Lomb – Technolas). I have recently had access to this phenomenal device, which is not yet available in the United States. I am still working to understand its individual characteristics and how these might differ from what I use presently. The device uses OCT to provide a very high resolution image of the anterior segment along with three dimensional corneal tomography, as well as biometry for IOL calculations. Hopefully the device will in time have epithelial thickness mapping and overall aberrometry included, which may make the overall investigative process of the patient evaluation considerably shorter.
- Casia 2 (Tomey). Similar to the Anterion/ACE, this device has excellent preoperative cataract reports, detailing anterior and posterior corneal astigmatism and anterior chamber depth. Also, by entering the axial length, it provides lens calculations using a variety of formulas. I find the information particularly useful in patients who are potential outliers with extreme anterior chamber depths and lens thicknesses influencing me to alter the lens power a little to suit.
CONSULTATION
By the time patients see the consultant, they usually feel we have been very thorough. In case they do not absorb the content of our discussion, we provide a copy of the letter to their general medical practitioner, which serves as a report along with salient points discussed. They are evaluated at the slit-lamp along with a 78-D and indirect fundus evaluation. All previous investigations are reviewed, paying specific attention to any issues raised.
If patients are suitable (most are, including post-laser refractive surgery patients), a frank discussion takes place about the most important aspects of the surgery. We use the Victus femtosecond laser (Bausch + Lomb) in every case along with limbal relaxing incisions for those who have corneal astigmatism of 0.75 D to 1.25 D and toric lenses for those above 1.25 D. This process is explained along with the risks and benefits of the actual procedure. For middle-of-the-road patients, such as those who do not have dense cataracts, glaucoma, extreme refractive error (long or short eyes), we discuss bilateral immediate sequential cataract/lens surgery.
Then, we make special reference to the process of adaptation and the need to be patient and allow this to happen within a time frame of 3 to 6 months. However, more than 90% of patients get most of their visual requirement right away. These patients are ecstatic to have their expectations are exceeded.
We also make very clear that they may get halos (10%) bad enough to affect their ability to drive at night. In our experience, this phenomenon recedes (if not disappear completely), and takes 3 months to noticeably reduce, possibly longer. We also reassure these patients that of approximately 8,000 trifocals since 2011, no patients have had their lenses replaced because of night driving issues.
LENS CHOICE
For hyperopes, I tend to aim for a slightly plus outcome, as they hate being shortsighted and complain about the lack of crisp vision at distance. With myopes who have a long axial length and are more forgiving in terms of refractive error, I choose a lens that makes them plano or slightly myopic. I always explain to hyperopes that distance will not be what they are used to, but they will adapt in time, and myopes the same for near.
From our experience, the ability to see near as well as distance correlates well with patient satisfaction. Thus we advise and use trifocal lenses where possible. In those who may not be suitable, our preference is to use a monofocal plus lens, in particular the Isopure (Physiol/BVI) which in our experience more than meets the American National Standard for Ophthalmics and AAO so-called EDOF standard.
We offset the non-dominant eye by -0.75 D, which provides patients with fairly good spectacle independence. Also, we emphasise prior to surgery that we are attempting to reduce their need for glasses but they will need reading glasses for fine print and prolonged near activity. Again, we set the expectations to ensure they are realistic and lower than what we believe can be achieved. They are often amazed when they are able to read a newspaper without their glasses.
POSTOPERATIVE
With the process above, we find we do not have many patients with major postoperative issues. Problems may be result from:
- Residual refractive error (spherical equivalent or astigmatism). We correct by PRK as soon as stable. Our PRK enhancement rate following premium lens surgery is about 1% and is a quality standard we report internally each month.
- Exacerbation of dry eye from drop or preservative toxicity. We resolve this by provision of artificial tears and occasionally switching to preservative-free drops.
- Slow adaptation. This requires a bit of hand-holding and reassurance.
CONCLUSION
We are grateful to have a very successful refractive cataract and lens practice with a high uptake of premium lenses. Key aspects of this success are good clear communication, setting expectations and ensuring patients needs and desires are realistic.
Complete diagnostics, thorough evaluation and a very frank discussion along with the reassurance that we will look after them well after surgery provides patients with the confidence and right frame of mind to proceed with premium lens surgery. OM
REFERENCES
- Daya S. Let’s Speak Lenspeak. https://crstodayeurope.com/articles/feb-2021/lets-speak-lenspeak . Accessed Dec. 21, 2021.
- Dell S. The New Dell Questionnaire https://crstoday.com/articles/2017-may/the-new-dell-questionnaire/ . Accessed Dec. 21, 2021.
- Daya S. OPD-Scan III: Powerful Informatics Helps Guide Preoperative Planning https://www.nidek-intl.com/archives/004/201909/5d897d00961b8.pdf . Accessed Dec. 21, 2021.
- Daya S. Clinical utility of OPD Scan III and RLE-Cataract report. https://eyetube.net/spotlight/nidek/clinical-utility-of-opd-scan-iii-and-rle-cataract-report . Accessed Jan. 4, 2022.
- Melles RB, Holladay JT, Chang WJ. Accuracy of Intraocular Lens Calculation Formulas. Ophthalmology. 2018;125:169-178.
- Koch DD, Jenkins RB, Weikert MP, Yeu E, Wang L. Correcting astigmatism with toric intraocular lenses: effect of posterior corneal astigmatism. J Cataract Refract Surg. 2013;39:1803-1809.









