Informed consent for patients receiving IOLs has never been more important — patients need to know their options as well as the risks and benefits. Only after receiving this information can they make a decision on the IOL best for their needs.
So, how does this conversation with patients go in my experience? Here, I discuss my methods for gathering the relevant data for each patient, as well as effective, accurate presentation of that data to the patient.
RESEARCH BEGINS WITH THE FIRST ENCOUNTER
For starters, the IOL option is not mentioned for the first time at my initial visit with the patient. The idea that the patient will need to decide on an IOL has already been planted during my practice’s first interaction with them.
When someone contacts the clinic, whether by phone or email or via the website, a link is sent to the patient for them to submit a medical history form. Along with the usual medical, ophthalmic and medication questions, this form specifically asks what the patient is hoping to achieve from possible surgery.
Are they looking for good distance vision knowing that they would need glasses to read up close? This would suggest a monofocal or monofocal toric IOL with emmetropia as the goal. Are they seeking greater freedom from glasses? If so, are they prepared to wear glasses for small print, suggesting that an extended depth of field (EDOF) IOL or mini-monovision (blended vision) is the best approach? Are they seeking the widest range of vision possible? This suggests a trifocal IOL or blended vision with an extended range of focus IOL.
HOW TO MINE FOR OBJECTIVE DATA
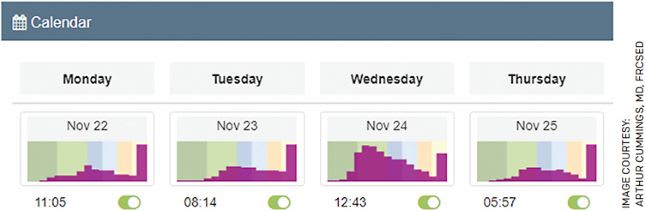
To help the patient make an informed decision, we often use objective visual data obtained with Vivior Behaviour Monitor (VBM) to determine their preferred working distances, head position, the ambient light temperature and intensity and the amount of UV- and blue-light that the patient is exposed to. This data is collected over a 36-hour period using VBM.
Sometimes this is achieved by wearing the Vivior Monitor (Vivior AG) for about 12 hours each day for 3 days, but most times it is collected over 4 to 7 days, or a total of 36 hours. The device consists of sensors measuring distance, ambient light and color, an accelerometer, a gyroscope and a magnetometer; it is worn on prescription or clear glasses.
The data is collected in the patient’s home and office environment and provides more insight into their visual requirements than any questionnaire or conversation may produce. The recorded data are uploaded to the cloud when the system is returned for processing and analysis. Sensor data are converted into patient behavioral data using artificial intelligence algorithms and provided to the surgeon.
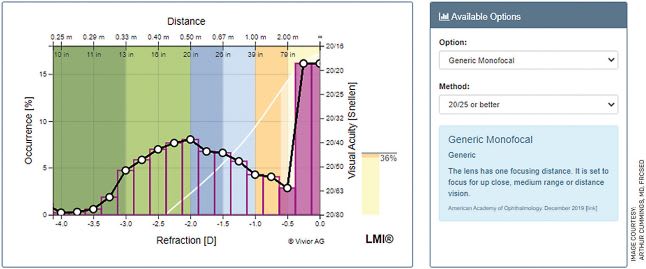
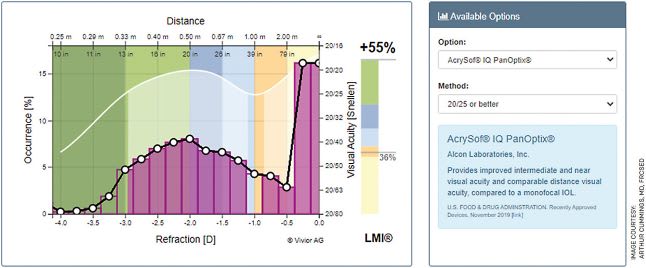
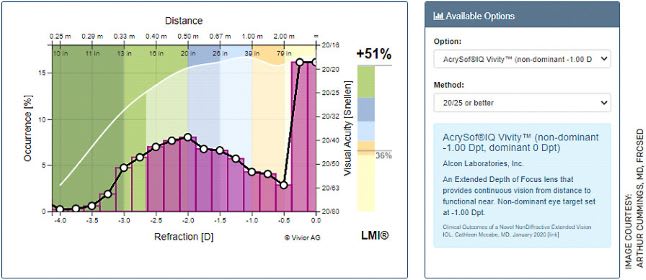
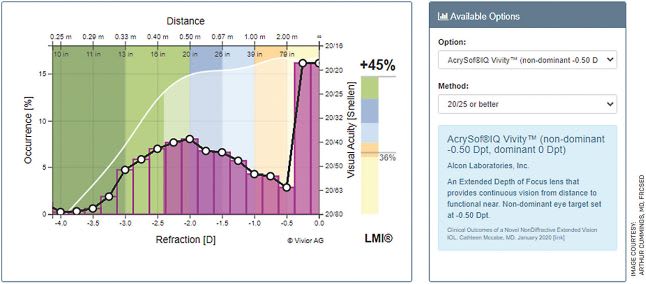
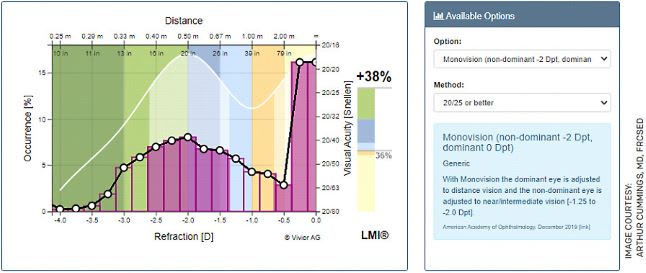
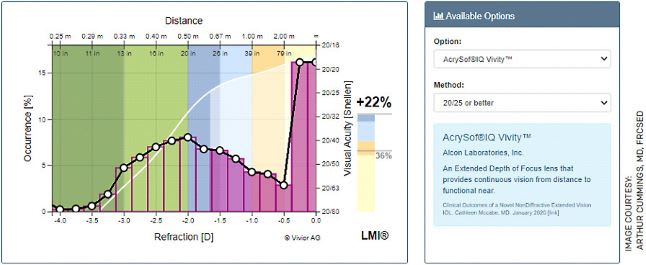
The Vivior software then compares the defocus curves of almost all the available IOLs on the market to be compared to the patient’s personal defocus curve. Additionally, the software also compares this to blended vision with a range of defocus targets for the reading eye including 0/-1, 0/-1.25, 0/-1.50, 0/-1.75 and 0/-2. IOLs like the X-wavefront-shaping Vivity (Alcon) IOL have the Vivity defocus curve in four versions, namely both eyes and emmetropia all the way though 0/-1 in 0.25-D increments of 0/-0.50 and 0/-0.75.
Using the VBM data is the simplest way to select the most appropriate IOL match, but additional issues must be considered as well, such as cost, acceptability of blended vision on testing, aversion to any night-time quality issues such as haloes or glare at night with driving.
PATIENT EDUCATION BY PICTURE
Vision breakdown
Figure 1 is a sketch that I make on every consent form even if we have already made a choice using the VBM data. It simply illustrates and documents the process that we have been through to inform the patient and arrive at the best decision for them.
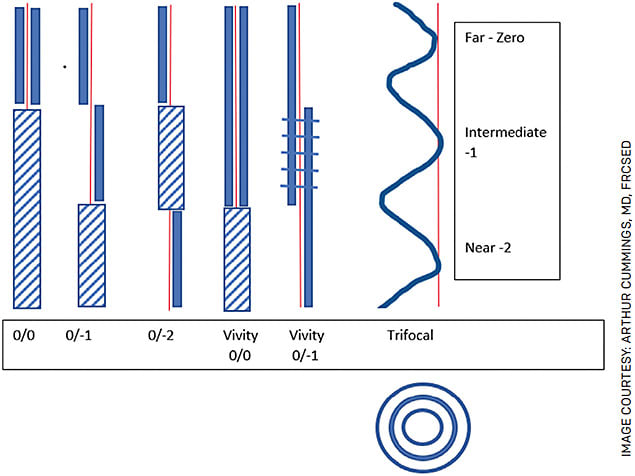
I explain to patients that the thick blue lines represent where they can see without glasses. So, with 0-0, they can see far if we hit target and will need glasses for intermediate and near vision (PC and phone – shaded area).
If they choose 0/-1 with a monofocal IOL, they will see far and intermediate without glasses, but they will need glasses for near (ie, phone, reading a menu or book) shown in the shaded area with diagonal lines.
If they choose 0/-2, they will see far and near but will find there is a gap in the centre, around where a computer display would likely be. The patient may require glasses for the computer, and they may find that dealing with the anisometropia with one eye at 0 and the other at -2 is more than they can comfortably manage. If they do have issues with night glare, glasses can correct this for night driving.
Vivity can correct two distances without any dysphotopsia (glare or halos). So with both eyes at 0, distance and intermediate vision is good and the patient needs glasses up near (shaded area).
Vivity at 0/-0.50, 0/-0.75 or 0/-1 provides a significantly extended range of vision without dysphotopsia. Now, instead of a gap in the middle like with monovision 0/-2, there is now overlap (horizontal bars).
The trifocal provides the most certainty at freedom from spectacles, but this technology also results in increased dysphotopsia and potential issues with driving at night that spectacles cannot remedy.
Trifocal vs EDOF
The next thing that I tell patients tends to help with making the decision on the trifocal vs an EDOF. I start by saying, “There is no free lunch in optics.” What that means is that if we start stretching the range of vision, it will cost us in terms of the quality of vision and possibly in the sense of balance between the two eyes. If you want the most complete range of vision, it may cost you in quality-of-vision terms, especially concerning driving at night.
If you are a taxi driver who drives at night and you cannot risk not being able to drive at night, then Vivity with one eye at 0 and the other at -0.50 or -0.75 significantly increases the range while preserving good night vision. So, the more complete the range, the lower the night vision quality. The better the night vision quality, the less the range of vision.
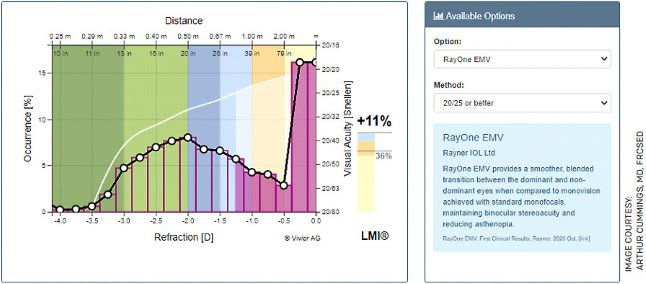
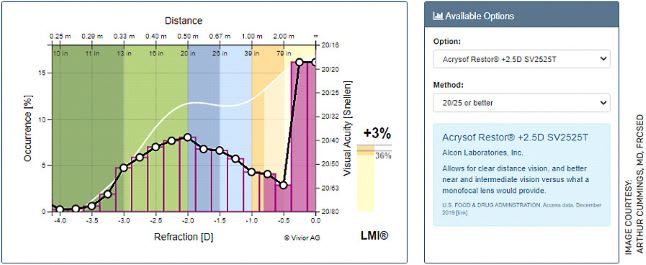
Vivior’s dashboard provides the ultimate insight into the patient’s visual requirements and how an IOL may address them. The examples in Figures 2-11 illustrate the LMI or Lifestyle Match Index.

DON’T FEAR THE COST FACTOR
The final hurdle we discuss is typically cost. I have learned along the way that we underestimate patients’ willingness to pay. If I sense any resistance to cost, I usually revert to the analogy of hearing aids. In Ireland and most of Europe, the additional cost for advanced technology IOLs or presbyopia-correcting IOLs is less than €1000 per IOL more than a monofocal IOL. I tell patients, “This is a once-off cost and provides you with the increased functionality on a permanent basis, every waking minute. With hearing aids, the costs are closer to €4000 to €6000 per set of hearing aids, and these are typically updated every 4 to 6 years.”
Patients have no problem paying this, yet we think that they may be resistant to this one-time charge. There is also a modest cost of €100 to €150 (about $113 to $169) for the use of Vivior, but the explanation that VBM data provides the very best method of selecting the most appropriate IOL for their visual needs is usually well accepted, once they realize that IOL surgery is typically permanent.
A COMPREHENSIVE CONSENT
Consent for cataract or custom lens replacement has evolved into the typical consent around the risks and benefits of the surgery itself, plus an additional consent for the IOL design or refractive target offset or both. As with any consent, patients need to know their options and understand the risk/benefit and the cost/benefit ratios for each.
I have found that following the above protocol serves these purposes well. OM









