We are privileged to operate in an industry that is innovating rapidly. Investments into R&D span the gamut from patient-experience customer relationship management software to diagnostic instruments and certainly to ophthalmic lasers and IOLs used in cataract surgery.
Given the rapid innovation we are experiencing in our field, it should come as no surprise that as ophthalmologists and CEOs of ophthalmology practices and ASCs, we are constantly faced with decisions on when to add new technology to our organizations. When making these decisions, we have to maintain discipline not to chase shiny new toys if they are not better for patients and prudent for the organization.
We also have a responsibility to our stakeholders when making big and sometimes frequent capital investments. How will it impact the patient experience, employee experience, efficiencies of operations, education efforts with our communities and ease of use for our physicians and surgeons?
Here, I walk you through my decision-making process when faced with the prospect of a new technology purchase.
CLINICAL OUTCOMES ALWAYS COME FIRST
When I consider adding a new technology to my practice, the patients’ best interests are paramount. If I look at the data, clinical outcomes, recommendations from trusted colleagues and trust in the people running the firm that is manufacturing the new tech, the first and most important question I ask myself is whether the contemplated investment will result in better outcomes for patients. If the answer is yes, I often feel a moral imperative as not only a CEO, but also a physician-CEO, to find a way to make the numbers work.
PATIENT AND EMPLOYEE EXPERIENCE MATTER TOO
Going beyond surgical outcomes and 20/20 rates, another important factor to consider relates to the patient’s experience with the technology — how will they perceive the value of the technology they are getting? Does it make a procedure faster, more comfortable during the surgical experience and possibly even during the preop workup and postop clinical experience?
Oftentimes, the employee experience with a new piece of technology is equally important to the patient experience. If it is easy for the team to use, their excitement about delivering it to the patients will reflect accordingly.
In addition, we have been very intentional about defining the brand we want to present to our patients and our community. Sometimes adding a new piece of technology can improve the patient experience, even when it is not used as our primary technology for the majority of our patients. For example, we’ve found it important for our patients to be confident they have access to every advanced technology out there, so that they never question whether we are just recommending something because it is the only thing we have.
One example of this is the Light Adjustable Lens by RxSight. We have found that a subset of patients really benefits from this technology, so we are happy to be able to offer it, even though it is not our most frequently recommended IOL. By adding this technology, we’ve elevated the value of our practice to patients by building trust — they see that if there’s a technology they really need, they’re going to be able to get it with us.
WHEN TO PUT UP THE CASH
Once patient outcomes and experience objectives are satisfied, the next thing to consider is the economics of the technology for the practice. With all the innovation occurring in our space, it is common that one vendor’s superior product will be challenged by another competitor before long. For example, many companies are innovating around new presbyopia-correcting IOLs and lasers. Sometimes, the newest laser or lens is clearly better than the others. Other times, clinical outcomes are equivalent, so the decision comes down to financial considerations.
Some of the issues we have experienced that lead us to evaluate whether to make a new expenditure include dated technologies. Sometimes a technology has been solid for years, providing amazing outcomes and experiences for patients, but eventually it reaches the end of its useful lifespan and it is time to upgrade to newer versions of the same technology. This can occur due to manufacturer decision to no longer support and service the technology, and the lack of parts and equipment to maintain them.
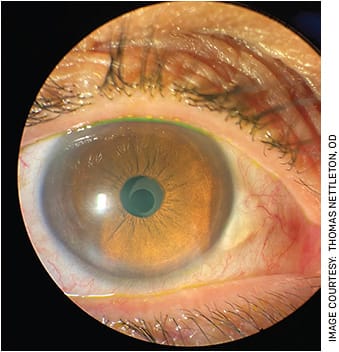
Other examples include operational efficiencies that can be achieved by moving to a new technology because it is faster and/or renders office visits no longer necessary. Heads-up surgical displays help surgeries run more quickly and smoothly and, just as importantly, save wear and tear on the surgeon’s neck and back. The EVO ICL (STAAR Surgical) represents another such case. The addition of a central fenestration in the phakic IOL completely eliminated the need for a presurgical step, resulting in many hours of saved preoperative staff and doctor time.
MEASURE AND CALCULATE
When considering new technology to replace an existing solution, we run pro formas that look at projected procedure volume, reimbursement per projected case, amortization and depreciation of the capital equipment being used, the likelihood of reimbursement per procedure as well as rebates that might occur per volume and instances of insurance denials. This goes along with calculations as to the more difficult-to-measure benefits of patient experience, staff experience and impact on the brand and overall value to the organization.
Here is a recent example from my practice, showing the numbers that determine whether adding a new piece of capital equipment was worthwhile in the glaucoma space. We are currently performing eight to 10 micro-invasive glaucoma surgery (MIGS) procedures per month using a combination of MIGS devices and goniotomy. The cost of some MIGS devices when bought in bulk is approximately $1,475 per stent. The organizations experience 6% additional info/denials and recuperate an average of $1,759.64 in revenue through third-party reimbursement.
If we were to move our combination cataract and MIGS procedures to endoscopic cyclophotocoagulation (ECP), we estimated we would perform roughly 100 cases per year. Given that this is a long-established procedure and CPT code with consistent third-party reimbursement, we expect to generate $2,553.21 per case with minimal third-party denials. At a capital equipment cost of $66,826.10, not factoring in trade-show discounts and promotions, rapidly depreciated and amortized over 7 years, we expect to be profitable by month 13.
When looking at a 5-year projection, the practice would be 37% more profitable doing cataract and glaucoma surgery with ECP compared to doing combined cataract and glaucoma surgeries with the stent.

BENEFITS FOR ALL INVOLVED
Physicians and CEOs of ophthalmic practices and ASCs are inundated with decisions about when and if to add new technologies for the benefit of their patients.
We live in an age and space of rapid innovation, and patient interest is always paramount. Clinical outcomes must trump financial considerations when making these complex decisions. When medical and clinical outcomes are in parity with the status quo, decisions around adding technology go to patient experience, employee experience and profitability of the practice. This creates an environment for further investment and innovation — all for the benefit of patients.
It’s exciting to operate in a space with so much opportunity for patients, physicians, practices and all stakeholders to deliver high-quality outcomes to those who need ophthalmic care. OM









