TAKE-HOME POINTS
- Scrupulous staff training is essential. Technicians should not just know how to push the buttons — they should also know how to recognize results that seem off.
- For accurate assessment, take measurements at least twice.
- Obtain readings from multiple to get a full, accurate picture of the patient’s corneal condition.
- Be aware that color values or the scale can vary with device and be manually changed by individual practices, so develop the habit of double-checking the scale.
- Do not perform topography on the same day IOP-measuring devices are used. The anesthetic drops that accompany their use contain preservatives and alter blink patterns, which can affect results by introducing epithelial changes.
- Advise patients not to wear contact lenses for a period of time prior to topography measurements, as they can distort the curvature of the cornea.
Accurate corneal topography is an important factor in successful refractive cataract surgery. Additionally, corneal diseases, such as keratoconus, pellucid marginal degeneration and post-LASIK ectasia, are contraindications of refractive cataract surgery and can be ruled out with the help of corneal topography.
Still, inaccurate topographic measurements can occur, typically due to not using the right equipment, insufficient staff training, inaccurate measurements or even routine issues such as overlooking the scale and failing to take patients off contact lenses.
“We always have to step back and remember, the two primary readings that go into our formulas for picking lens implants, whether they be traditional, toric astigmatism correcting or premium lenses, are the cornea curvature and the length of the eye obtained by biometry,” says Jeffrey Whitman, MD, president and chief surgeon at Key-Whitman Eye Center in Dallas. “They’re both equally important, so if you’ve got bad information going in, you’re going to have bad information coming out.”
Getting accurate topography can mean the difference between excellent outcomes and poor outcomes that leave patients literally seeing stars — or worse.
Herewith, three ophthalmic surgeons offer a brief compilation of advice from for getting accurate topography the first time, every time.
START WITH THE RIGHT TOOLS
As recently as 20 years ago, keratometry was the standard of care in assessing the cornea in preparation for refractive procedures. Then along came the first generation of premium lenses, and the first corneal topographers arrived soon after. Unlike keratometers, which only measure corneal curvature at three or four points, topographers and tomographers measure thousands of points, resulting in magnitudes of greater accuracy. Today, ophthalmologists have many such devices at their disposal, including Orbscan (Bausch + Lomb), Atlas (Zeiss), OPD (NIDEK), Pentacam (Oculus), Galilei (Ziemer), Sirius (CSO) and TMS-4N (Tomey).
Owing to the “digital revolution” in health care, moreover, devices are becoming more advanced every year and demonstrating growing interoperability with other devices in the surgical suite and electronic patient records. The result: reduced risks of errors.
“Some topography units will integrate with certain femtosecond lasers, so you can take the topography of the patient and even capture a photo of the patient’s iris and then import that data into [those] femtosecond lasers,” says Jennifer Loh, MD, of Loh Ophthalmology Associates in Miami. “The devices are talking to one another and reducing that necessity for paper, because that’s where things can get lost in translation.”
TRAIN FOR SUCCESS
Today’s devices are advanced, but they still require staff fully trained who know how to use them and interpret the results. It’s not enough to know how to push the buttons; technicians should also know how to recognize results that seem off, says Kendall E. Donaldson, MD, MS, a professor of clinical ophthalmology and medical director at Bascom Palmer Eye Institute in Plantation, Fla.
“Ideally, they should be able to understand how to read the results and determine whether they should potentially repeat them [and/or] whether they should go discuss with the doctor,” Dr. Donaldson says. “Even our most advanced technologies, such as the IOLMaster 700 [Zeiss], require much less skill than biometry did 20 years ago, but they still require attention to detail.”
Many vendors offer on-site training, but Dr. Whitman emphasizes the need for trainees to be shadowed by a veteran technician.
“The techs at our practice are not permitted to start readings on their own until they’ve gotten to do it numerous times with somebody who’s fairly expert at it,” Dr. Whitman says. “I’d rather them come to me and say, ‘Hey, this looks bizarre, something is not right.’ And I might tell them right then, ‘Put a teardrop in there, let them sit for 5 minutes, then do another one.’”
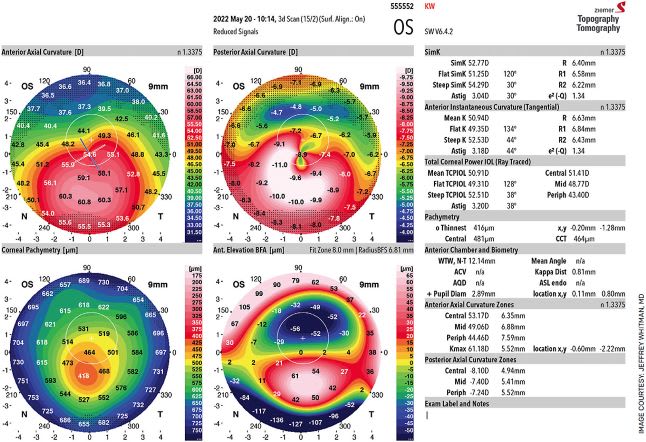
This topography demonstrates classic changes from keratoconus in a 24-year-old male. Note marked steepening and thinning in the inferior temporal area.
MEASURE TWICE — AT LEAST
Everyone is familiar with the carpenter’s aphorism, “measure twice, cut once.” The same advice applies to the assessment of corneal topography. In practice this means measuring at least twice — possibly more — and some using multiple devices.
“If something doesn’t look exactly the way it should, it’s never a bad idea to ask the patient to come back. A lot of times part of the issue is that the person has dry eye,” says Dr. Loh. “I have a very low threshold for asking the patient to come back and treating their dry eye.” Even if the initial scan looks perfect, she notes that erring on the side of caution by bringing the patient back for another never hurts.
Dr. Donaldson agrees, particularly when measurements of axial length or corneal curvature differ significantly between eyes. “Everyone who has a really long eye or a really short eye should be measured more than once. In patients who’ve had prior radial keratotomy or have a history of a penetrating keratoplasty, their measurements are very difficult to take, and they oftentimes would benefit from repeat measurements.”
USE MULTIPLE SOURCES
Dr. Whitman obtains readings from three devices to get a full, accurate picture of the patient’s corneal condition.
“We have the astigmatic value that comes off our biometer, whether it be Argos [Alcon], Lenstar [Haag-Streit] or IOLMaster. We have our astigmatic values that come off our Nidek OPD, and then we have our gold standard topographer, which for us is our GALILEI G4,” he says, adding that he considers agreement between two devices appropriate for proceeding with treatment.
“If [the readings are] very different, we know there’s probably something going on. There may be dry eye, there may be MAP dystrophy, and at that point we decide what we’re going to do” with respect to pre-surgical treatment, says Dr. Whitman, whether it’s a regimen of artificial tears, inserting tear drainage plugs or scraping the central surface epithelium.
Dr. Donaldson follows a similar protocol but acknowledges that not every practice can do so. “Most practices don’t have three to five devices like we may have in academics or in high-volume private practices. Most practices have two devices, on average — one that’s a topographer/tomographer and a second that does biometry. But I do agree that two devices that you’re very familiar with is really the minimum that should be used, especially for premium IOL technology, and even more for complex cases.”
CROSS YOUR T’S, DOT YOUR I’S
Clues for the color scale
Several routine details may go missed or overlooked, leading to inaccurate topography results. For example, every topography printout displays a color map that corresponds to the patient’s actual magnitude of astigmatism or corneal steepness. Dr. Loh notes that the values or the scale can vary with device and be manually changed by individual practices; developing the habit of double-checking the scale is important. Occasionally, surgeons who get used to their topographer may move to a different practice with a different device, and, even if the device is identical, its settings may be different.
“The color gradation could be a little more subtle because the scale’s different,” she says. “You can have 0.5-D steps or 1.0-D steps or 1.5-D steps, and that will change the color of gradation in the topographic map. Sometimes, as a surgeon, you get used to the certain color pattern of a topography, so you say, ‘Oh, this scan looks normal.’ But it’s important to double-check the scale and the actual numbers.”
Beware blink-altering tests
Another mistake that can lead to inaccurate topography results consists of taking measurements on the same day IOP-measuring devices are used. Such devices may touch the eye, and the anesthetic drops used to make these measurements contain preservatives and alter blink patterns, which can affect results by introducing epithelial changes.
“Technicians have to be aware that if drops are put in, it’s not a good day to make these measurements,” says Dr. Donaldson.
Keep them out of their lenses
A third avoidable mistake is neglecting to advise patients not to wear contact lenses, which can distort the curvature of the cornea, for a period of time prior to topography measurements.
Distortions can persist for weeks, requiring the patient to return multiple times to ensure the topography is stable and thus delivers accurate measurements for lens choice, Dr. Donaldson notes. She says standard operating procedure is to keep patients off soft contacts for one week and off hard contact lenses for one week for every decade of wear.
“Some of our patients have been wearing rigid contact lenses for 50 years and may need to be out of those lenses for more than a month before we can get accurate results,” she says. “So having reproducible results on multiple occasions is key with contact lens wearers and patients with more advanced ocular surface disease. Even a very small change in shape can translate into a very dramatic error in the IOL power. That’s a very big issue with multifocal lenses, which are very unforgiving of residual refractive error.”
ULTIMATE OUTCOMES LIE WITH THE SURGEON
While mistakes and oversights with respect to measuring corneal topography don’t happen often, they do occur. And as Dr. Whitman reminds, the ultimate responsibility for outcomes lies with the surgeon, so it’s worth paying extra attention to detail when a patient’s eyesight depends on accurate data.
“We need to be obsessive about obtaining the information, evaluating the information and making the front of the eye as pristine as possible so we can get the best vision possible,” Dr. Whitman says. “There’s a responsibility as an ophthalmic surgeon not just to operate, but to make sure we get the best readings and have the eye in the best condition possible so we can get the best result possible.” OM








