Experience is the best teacher. The trust and confidence you have as a surgeon flows over to how much trust and confidence your patients will have in you. This should be a lifelong pursuit.
Gaining experience and exceeding with presbyopia-correcting IOLs (PC-IOLs) and a premium IOL practice is a journey, not something that happens overnight, and there are many building blocks to make this work. Beyond the technology, you need to hone your communication skills and your surgical skills. It is a mindset for you as the surgeon, your office staff and surgical counselor — everyone needs to use the same language when talking to the patient. The things that will make you successful in this realm of ophthalmology fall into several categories; what I call the “comorbidities” of premium IOL surgery, which I will discuss below.
COMMUNICATION WITH THE PATIENT
Communication starts from the moment the patient calls your office for an appointment and continues when they check in followed by their workup with the technician. Before you examine the patient, it is nice to have as much information as possible, but this is not always done in one appointment. Preoperative testing is not done at the initial appointment; patients return for preoperative testing on a different day.
The way you talk and communicate and how you make the patient feel is so important. For example, after the patient is worked up and you explain your findings, you must explain to them the value of treating dry eye and how it will affect the outcome of their cataract surgery if not treated correctly.
In my practice, I explain to the patient that I need their help with preparing them for surgery — the better the condition of their cornea and ocular surface, the better the preoperative testing will be and the better their outcome will be after surgery.
Sometimes the ocular surface must be treated for quite some time. So, as their surgeon, you need to acknowledge to the patient that they may be frustrated but that you want to get it right and give them the best outcome that you possibly can. This initial plan could include nutraceuticals and preservative-free artificial tears along with cyclosporine.
TREATMENT OF ASTIGMATISM
Treating astigmatism was the game changer for me. Astigmatism correction is so important to correct because if it’s not, outcomes will not be good for the patient — they will still be dependent on glasses. A poor ocular surface can cause irregular cornea and induce erroneous astigmatism.
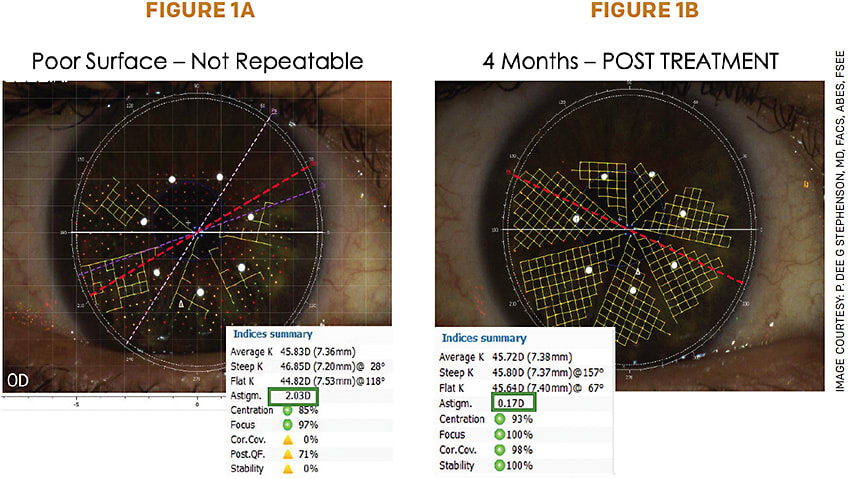
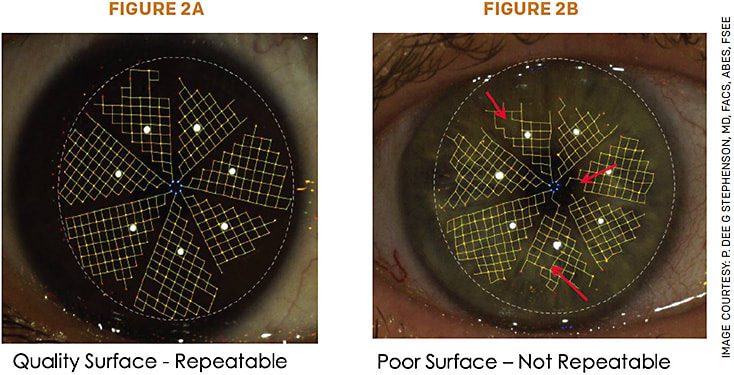
A key aspect of treating astigmatism is repeatable, reproducible preoperative testing. I am a cataract refractive surgeon and do not perform PRK or LASIK, so I need to get it right the first time. One preoperative tool is my topographer (Cassini), which also measures a quality factor of the tear film. (Figure 1, and Figure 2).
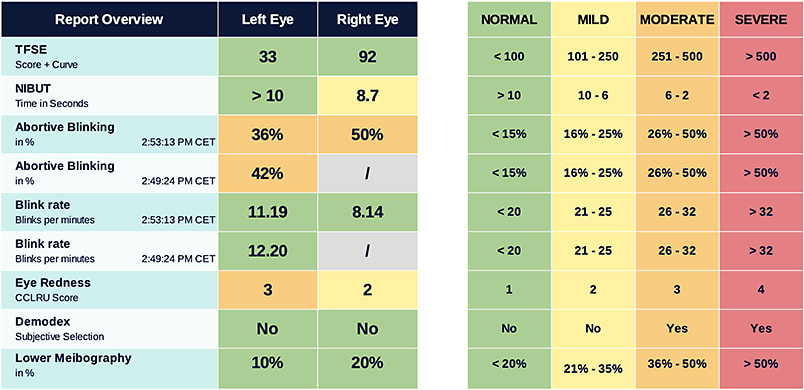
In addition, I have recently implemented the Tearcheck dry eye diagnostic and analyzing tool (I-MED Pharma), which does nine dynamic tests and a report overview with photos of the patient’s eyes. (Figure 3). The patient can see the scan, which helps them understand the disease process. I explain and actually show them the honeycomb pattern on the Cassini and the Tearcheck prints out a report card for the patient of all diagnostic tests done.
Soon, Tearcheck will have topography, which will add more helpful information. Dry eye can cause astigmatism, so repeating all these tests allow you to not treat something that is not really there.
In addition, I have used the intraoperative aberrometer ORA (Alcon) for more than 10 years with much success. This allows me to treat low amounts of astigmatism with the new low astigmatism enVista toric MX60PT (Bausch + Lomb). I recently presented the great results that I have obtained at the Caribbean Eye Meeting in Puerto Rico. I reported on 101 patient outcomes, achieving 100% reduction to 0.50 D or less (43% no residual astigmatism and 64% 0.25 D or less).1,2
TREATING DED, BLEPHARITIS, DEMODEX, MGD
Overall prevalence of dry eye disease (DED) is approximately 30 million people and only about 14.5 million are actually diagnosed with DED. DED increases with age and is more common in women; however, this is changing with the usage of hand-held devices.3-6 There is a subset of patients who are asymptomatic — this is when preoperative diagnosis testing is so important, because if it is not diagnosed before surgery and they become symptomatic after surgery, the patient will think the surgery caused the DED.
Blepharitis, rosacea, Demodex and meibomian gland dysfunction are so important to diagnose and treat before cataract surgery is performed. I treat all patients before preoperative testing for blepharitis with hot compresses and hypochlorous acid spray or Oust Demodex with tea tree oil (OCuSOFT) for the treatment of Demodex. If need be, I also treat my patients with thermal pulsation via iLux (Alcon) or TearCare (Sight Sciences) — LipiFlow (J&J Vision) is also available. In addition, I recently started using intense pulsed light (E>Eye, I-MED Pharma) with expression of glands to improve the patient’s meibomian functions.
DIAGNOSING MACULAR DISEASE
Pre-existing macular disease, epiretinal membranes, mild drusen or dry macular degeneration are all things you must diagnose before surgery. If patients have a suboptimal outcome because of any pathology, you will be liable because you didn’t tell them prior to surgery. Macular OCTs are a great diagnostic tool and should be a part of your cataract workup.
Having this information will enable you to recognize what contraindications of certain pathology will affect your patient’s outcome in order to offer only particular IOLs, especially PC-IOLs, to the patient. For example, macular disease would give a suboptimal outcome with multifocal IOLs.
KNOW THE PC-IOLS
I use several PC-IOL technologies, including PanOptix (Alcon) and Vivity (Alcon).
In particular, I have extensive experience with the accommodating IOLs (Crystalens/Trulign, Bausch + Lomb), both of which I have used for more than 15 years. There is a real learning curve with these lenses, but once conquered they give great predictable results. Accommodating IOLs have become my go-to premium PC-IOL for post-refractive patients, which are a big part of my practice.
I do the non-dominant eye first, set for -0.50 D and wait 2 weeks. Then, I do the dominant eye and set for plano or first minus. The patient is atropinized for 3 days post-surgery and instructed to do one near-far reading exercise for 6 months to a year (change font size to help with retraining the near).
Again, it is a “contract” with the patient as it involves them in the success of their outcome, with a vested interest — both financially and a known time commitment — that will make for a better success. These lenses are aspheric, the same power from center to edge and do not induce any unwanted dysphotopsias on an already irregular cornea. They are not affected by mild tilt or decentration. The Trulign lens is very stable rotation wise as it has four-point fixation, so it stays where you put it.
In addition, I have great success with the PanOptix IOL (Alcon), both toric and non-toric. Patients understand they will have a tradeoff, being eyeglass independent but possibly experiencing halos and glare at night. Some patients think it is a small price to pay for not having to wear glasses at all.
All of my surgeries go into a data bank. There, I can follow my outcomes and update my A-constants as well as note my surgically induced astigmatism for right and left eyes for every IOL I use.7
DISCUSSING THE LENS OPTIONS WITH PATIENTS
Never assume patients understand what you tell them. However, there are many tools you can use to educate and review with the patient what, in your opinion, is the best lens with the best outcome designed for them.
We start off with a brochure showing all of the options available through our office. Each of these options are explained thoroughly, and a recommendation is made. We show videos, give pamphlets of the different lenses and show the corneal topography with their total corneal astigmatism that was just captured during their diagnostics.
We also discuss with the patient what their goals and expectations are and look at their lifestyle to help determine what lens will meet those expectations. The best pearl to tell a patient is, “If you do not get a PC-IOL, you will still have to wear glasses to read.”
As for those patients who have astigmatism, they have to understand that they will have to wear glasses for everything, near and far, if they want to see the very best they possibly can. They must understand this before they even sign their surgical consents.
My recommendation is that you have to start with one premium lens and use it on the appropriate patients. Learn all the characteristics about the IOL, the good and the bad, and make that lens work in your hands. Know what patient will benefit from it and learn how to tell a patient that they are not a candidate for the lens due to their comorbidities or their unmet needs.
CONCLUSION
Remember that no matter how hard you try and how well you calculate your measurements and communicate, you will inevitably have an occasional unhappy patient. Do not let it ruin your day or lose too much sleep over it, but learn from it.
Hone your skills, know how to repeatedly correct astigmatism and treat dry eye, do not rush into surgery and know the lens. You should also refine skills of IOL removal and exchange, as well as have access to LVC as needed for refractive misses or surprises. Start slow, then when all the stars align you will know when the right time is to take on a premium IOL practice.
For young surgeons with limited experience, I recommend reaching out to a mentor for advice in creating a premium IOL practice. Also use resources from ASCRS, AAO Young Ophthalmology, etc.
I have continued to try to implement the best and get rid of things that don’t work. Now, my practice has an 87% conversion rate for premium IOLs. Be present, be patient and continue to learn what will make your practice grow and survive in this climate. You, as the surgeon, will also survive in this competitive market. Doing the best for your patients, being their advocate and ally, letting them know you are in this journey together to give them the best outcome possible will make you stand out as an excellent ophthalmologist. OM
REFERENCES
- Stephenson PDG: Improving Outcomes with Low diopter Toric Intraocular Lenses. Presented at: Caribbean Eye Meeting; February 4-7, 2022; San Juan, Puerto Rico.
- Stephenson PDG: Correction of Low Levels of astigmatism during Cataract Surgery with the Glistening free Monofocal Toric IOL with Enhanced Delivery Optics. Presented at: ASCRS Annual Meeting; April 22-26, 2022; Washington, D.C.
- Farid M. Dry Eye Disease: Let's Start Thinking Outside of the Artificial Tear Box. Ophthalmology. 2017;124(11S):S1-S3.
- Paulsen AJ, Cruickshanks KJ, Fischer ME, et al. Dry eye in the beaver dam offspring study: prevalence, risk factors, and health-related quality of life. Am J Ophthalmol. 2014;157(4):799-806.
- Epstein AB, et al. DRY EYE DISEASE What We Know About It Today and Its Importance for Optometry. Review of Optometry. https://www.reviewofoptometry.com/CMSDocuments/2016/5/ro0516_shiresuppi.pdf . Updated March 2016. Accessed March 19, 2019.
- Farrand KF, Fridman M, Stillman IÖ, Schaumberg DA. Prevalence of Diagnosed Dry Eye Disease in the United States Among Adults Aged 18 Years and Older. Am J Ophthalmol. 2017;182:90-98.
- Stephenson PDG. One-year evaluation of the performance of the Trulign toric intraocular lens implanted in eyes using intraoperative aberrometry to determine sphere, cylinder and position. J Clin Ophthalmol. 2019;3(2):162-165.









