In our practice, we must decide what type of IOL to place in a patient with glaucoma on a daily basis. As a glaucoma and refractive subspecialty practice, we have significant experience in this area and have learned that certain combinations of glaucoma surgery and premium IOLs tend to perform better than others.
Cataracts and glaucoma represent two of the most common causes of visual disability, and they often coexist and worsen together as an individual ages.1,2 In fact, up to 20% of patients undergoing cataract surgery are estimated to have some form of comorbid glaucoma.2
As glaucoma surgical techniques have advanced, it is now possible to more safely treat glaucoma concurrently during cataract surgery by utilizing a minimally invasive glaucoma surgery (MIGS). Newer, less invasive MIGS coupled with advances in premium IOL technology have made this controversial topic more important than ever.
Here, we explain how we handle these decisions.
MANAGE PATIENT EXPECTATIONS
In today’s world, cataract surgery is considered as much a refractive procedure as a medical one, and patient expectations are higher than ever before. In our practice, a patient is a candidate for a premium IOL until proven otherwise, and patients with glaucoma have just as much desire for an excellent outcome following cataract surgery as everyone else. Deciding which IOL to use can be challenging enough, but this is compounded in patients with glaucoma because of unique anatomical and functional characteristics.
There are several considerations for subjects with glaucoma undergoing cataract surgery beyond the IOL choice alone. This journey begins by listening to the patient, letting them tell you what they expect out of the surgery and understanding what you can deliver.
Patient desire for spectacle independence, age, general health status, glaucoma subtype, stage of disease, current medication burden, ocular surface disease and choice of combined glaucoma/cataract surgery vs cataract surgery alone all play a role.1-3
Just as, or perhaps more importantly, is understanding the things they would like to avoid (eg, increased possibility of nighttime dysphotopsias).
IOL OPTIONS
Aspheric is key
Most modern IOLs have an aspheric design meant to reduce spherical aberration and counteract the natural +0.27 um of spherical aberration of the natural cornea once the crystalline lens has been removed.3,4 This has been shown to increase contrast sensitivity, which is of interest for patients with glaucoma as they have reduced contrast sensitivity to begin with, especially in mesopic environments.5
As the natural crystalline lens becomes cataractous, it begins to produce more positive spherical aberration and can no longer offset the positive spherical aberration of the cornea, so swapping a cataract for an aspheric IOL alone may improve visual function in patients with glaucoma regardless of what type of IOL is used.
Monofocal, toric and accommodating IOLs are generally well accepted in the use of glaucoma given a good understanding of risks and benefits of implantation in different glaucoma stages and subtypes.2-4,6 These lenses do not split light; therefore, they pose less risk and enjoy more use in moderate to severe stage disease. The question is whether extended depth of focus (EDOF) and multifocal (MF) IOLs should be used and in what cases.
EDOF lenses
Current FDA-approved EDOF lenses include the Tecnis Symfony (Johnson & Johnson Vision) and the Acrysof IQ Vivity (Alcon). The Symfony uses an achromatic diffractive pattern to elongate depth of focus and correct for chromatic aberration, thus enhancing contrast sensitivity. Mencucci et al compared the Symfony against two different diffractive trifocal IOLs and found that contrast sensitivity was better in the Symfony group with better near performance in the diffractive trifocal groups consistent with their optical designs.7 The Symfony has been shown to have a dysphotopsia profile similar to a diffractive trifocal however, so the increased contrast provided may come at the expense of reduced near acuity and no improved visual disturbance profile over that of a trifocal IOL.8
More recently approved, the Acrysof IQ Vivity is a non-diffractive EDOF that uses Alcon’s two surface transition element “X-WAVE” technology to elongate and provide an extended range of vision without splitting light, thus improving visual disturbances to the level of a monofocal IOL.9 The pivotal FDA trial demonstrated a clinically significant loss in monocular contrast sensitivity compared to monofocal control; however, this was only at a single spatial frequency in mesopic conditions, and patient satisfaction with the Vivity was still high.9
MF lenses
MF IOLs currently offer a great opportunity for complete spectacle freedom, and we are fortunate to have excellent options available in the United States, including the Acrysof IQ PanOptix (Alcon) and the Tecnis Synergy (J&J Vision). The PanOptix uses Alcon’s diffractive ENLIGHTEN Technology and has been shown to provide excellent visual acuity across a wide range of distances in multiple clinical trials.10,11
The Tecnis Synergy uses a hybrid combination of EDOF and MF diffractive technology in an effort to provide good contrast with excellent unaided acuity through a wide range of vision even in mesopic conditions. Study results have shown a wider range of functional focus compared with other trifocal IOLs.12
The bottom line
We have used all of these IOLs with success when combining them with a MIGS procedure. For well-controlled, mild to early moderate glaucoma, we prefer MF IOLs (trifocals) as these give the patient the widest range of vision and spectacle independence possible. Contrast sensitivity is reduced with these IOLs, but not to a level that is clinically significant and remains in physiologic normal range.11,13 As disease state progresses or we feel that future lack of control will be an issue, we lean more toward EDOF options and enhanced monofocal options such as the Tecnis Eyhance (J&J Vision).
We agree with other colleagues who feel that glaucoma patients are potential candidates for premium IOLs if they have early, well-controlled, stable disease in both eyes and are not considered high risk for future progression.4,14
MIGS DISCUSSION
Confidence in our offerings
In our practice, we often refer to what we call the “20/20 patient experience.” By combining refractive cataract surgery with a presbyopia-correcting IOL and a MIGS procedure, we improve IOP control and potential ocular surface disease in part due to topical glaucoma medication reduction as well as enhance the patient’s quality of vision. With the newer IOL formulas, intraoperative aberrometry, light adjustable lens technologies and even access to refractive laser enhancements, we feel confident that we can offer patients better glaucoma control and better vision than they have ever experienced previously.
MIGS options
To ensure a truly exceptional patient experience, we seek to provide patients outstanding glaucoma control and visual outcomes as quickly as possible. We have found trabecular microstents such as the Hydrus (Alcon) and iStent (Glaukos) technologies to be extremely beneficial to patients when combined with premium cataract surgery. By pressurizing eyes into the mid-20s mm Hg at the conclusion of surgery, trabecular blood reflux is often minimized, which leads to excellent visual outcomes, often on postoperative day one. When performed well, cutting angle procedures such as goniotomy, OMNI (Sight Sciences) and ab-interno canaloplasty all have extremely rapid visual recovery. In patients on oral anticoagulants, trabecular bypass microstents are generally preferred.
Unfortunately, local insurance coverage often plays a role in the MIGS procedure chosen, and prior authorization is often requested. A clear clinic note stating the medical necessity of the procedure along with supporting documentation including visual fields, OCTs and poor tolerance to topical medications if applicable is a requirement. Therefore, the surgeon should have at least two to three MIGS procedures in their armamentarium that they feel comfortable with, both stent and cutting based.
Patient selection
Patient selection is critical to enhancing the chances of happy patients postoperatively. Generally, we only utilize presbyopic IOLs in patients with more mild glaucomas with minimal visual field loss. This minimizes patient concerns about decreased contrast sensitivity with these lenses and optimizes patient outcomes significantly.
In our prospective pilot study evaluating the combination of the Hydrus microstent and a trifocal IOL, patients are consistently pleased with their postoperative vision (See Case Report). We are now even offering refractive lens exchanges utilizing the trifocal technology to patients in their 40s and 50s with minimal lens opacification.
OUTCOMES
Due to the high quality of these IOLs, we feel confident that we are enhancing patient quality of life significantly with well performed combined cataract and MIGS procedures. By reducing glaucoma medication postoperatively, we are not only enhancing glaucoma control and visual outcomes, we are improving patient ocular surface disease significantly and actually reducing patient medication and refractive care costs postoperatively. These are some of the happiest patients in our clinic.
CASE REPORT
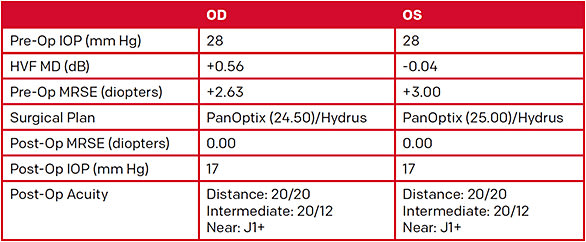
A healthy 50-year-old white male recently diagnosed with early preperimetric glaucoma. He was highly motivated to be completely spectacle free and not overly concerned with nighttime glare/halo.
This patient was referred to our clinic for glaucoma evaluation and was noted to have IOP of 28 mm Hg OU. He reported that his IOP had been monitored in the past but was never treated, and his father had lost vision in one eye from glaucoma. He was significantly hyperopic and very motivated to both eliminate his need for glasses and treat his IOP.
In our practice, this is an excellent candidate for a combined premium IOL/MIGS procedure. He had very early preperimetric glaucoma, and we felt that we could adequately control his IOP and give him the refractive outcome he desired.
The patient underwent bilateral implantation of a PanOptix IOL (Alcon) along with a Hydrus Microstent (Alcon). Three months postoperatively, he was spectacle free with binocular acuities of 20/20, 20/12 and J1+ at distance, intermediate and near, respectively. His IOP was 17 mm Hg OU with no topical glaucoma medication.


CONCLUSION
Combining MIGS and presbyopic IOLs is becoming an increasingly more viable option in our patients with both cataract and glaucoma. In those who have more mild open-angle glaucomas with healthy corneas and no significant macular pathology, we believe this combination ultimately is in the best interest of the vast majority of these patients.
In the past, glaucoma patients were not even considered for presbyopic IOLs due to progressive glaucoma concerns. With the continued advances in both IOLs and MIGS technologies, we believe that this option should be strongly considered in many patients with both glaucoma and cataract. OM
References
- Law SK, Riddle J. Management of cataracts in patients with glaucoma. Int Ophthalmol Clin. 2011;51(3):1-18.
- Shah M, Law G, Ahmed IK. Glaucoma and cataract surgery: Two roads merging into one. Curr Opin Ophthalmol. 2016;27(1):51-57.
- Fabunmi A, Sarkisian SR. Update on the Use of Premium Intraocular Lenses in Glaucoma. Curr Ophthalmol Rep. 2019;7:182-186.
- Teichman JC, Vold SD, Ahmed IIK. Top 5 pearls for implanting premium IOLs in patients with glaucoma. Int Ophthalmol Clin. 2012;52(2):65-71.
- Hawkins AS, Szlyk JP, Ardickas Z, Alexander KR, Wilensky JT. Comparison of contrast sensitivity, visual acuity, and Humphrey visual field testing in patients with glaucoma. J Glaucoma. 2003;12(2):134-138.
- Rabin RL, Rabin AR, Zhang AD, Burney EN, Rhee DJ. Co-management of cataract and glaucoma in the era of minimally invasive glaucoma surgery. Curr Opin Ophthalmol. 2018;29(1):88-95.
- Mencucci R, Favuzza E, Caporossi O, Savastano A, Rizzo S. Comparative analysis of visual outcomes, reading skills, contrast sensitivity, and patient satisfaction with two models of trifocal diffractive intraocular lenses and an extended range of vision intraocular lens. Graefes Arch Clin Exp Ophthalmol. 2018;256(10):1913-1922.
- Monaco G, Gari M, Di Censo F, Poscia A, Ruggi G, Scialdone A. Visual performance after bilateral implantation of 2 new presbyopia-correcting intraocular lenses: Trifocal versus extended range of vision. J Cataract Refract Surg. 2017;43(6):737-747.
- ACRYSOF VIVITY Directions for Use.
- Sudhir RR, Dey A, Bhattacharrya S, Bahulayan A. AcrySof IQ PanOptix Intraocular Lens Versus Extended Depth of Focus Intraocular Lens and Trifocal Intraocular Lens: A Clinical Overview. Asia Pac J Ophthalmol (Phila). 2019;8(4):335-349.
- Modi S, Lehmann R, Maxwell A, et al. Visual and Patient-Reported Outcomes of a Diffractive Trifocal Intraocular Lens Compared with Those of a Monofocal Intraocular Lens. Ophthalmology. 2021;128(2):197-207.
- Ferreira TB, Ribeiro FJ, Silva D, Matos AC, Gaspar S, Almeida S. Comparison of refractive and visual outcomes of 3 presbyopia-correcting intraocular lenses. J Cataract Refract Surg. 2022;48(3):280-287.
- PMA P040020/S087: FDA Summary of Safety and Effectiveness Data SUMMARY OF SAFETY AND EFFECTIVENESS DATA (SSED). www.accessdata.fda.gov/cdrh_docs/pdf4/P040020S049B.pdf . Accessed January 24, 2022.
- Ichhpujani P, Bhartiya S, Sharma A. Premium IOLs in Glaucoma. J Curr Glaucoma Pract. 2013;7(2):54-57.










