Leading any business in 2022 is not without challenges. Take the issue of costs alone. These are changing swiftly, and if you don’t keep an eye on costs of goods you can quickly find yourself in a deficit with some services.
PRESSURES ON ALL SIDES
I recently had a panel discussion with a couple of amazing surgeons. From that discussion, it was clear that physicians/surgeons don’t want their hands tied when it comes to new technologies, especially by the absence of or very low reimbursements for the procedures using these technologies. The surgeons also “need what they need” to make sure that they provide the premium patient a premium outcome.
All administrators want surgeons to provide the best care for the best outcomes to their patients. Administrators, though, need every case to be a profitable one as we navigate the ever-changing economic impacts.
Staff want to be paid more (And why not? Everything costs more!), patients want to pay less, the electric company expects payment, rent hasn’t been lowered, etc. We must work together to investigate new technologies not only for the impact they have on care but for the economic challenge they create when implemented. Sadly, many of the manufacturers in our space are also dealing with staffing issues, supply issues and increased costs to provide their goods.
So, between rising costs and inadequate reimbursements, it’s a challenging time. We must all work together to find “work arounds” for providing care to the patient — the party we all work for — and remain profitable.
There are two specific areas I cover in this article. First is the costs associated with premium/refractive cataract surgery. The second area, which has caused some degree of confusion and financial stress for every ASC and clinical practice, is MIGS reimbursement.
PREMIUM CATARACT SURGERY
I applaud the practices and facilities that have embraced refractive cataract surgery. At Bowden Eye & Associates, we have many success stories and testimonials from our patients. Being able to offer a premium service requires a dedication to education on the part of the surgeon, the clinical staff and the surgical teams. This is an added overhead for the practice and the facility, but the profitability becomes clear once everyone is educated.
Early concerns for my ASC team and me were the added Malyugin Rings (MicroSurgical Technology), the added iris hooks and the occasional double pass for the femtosecond laser to get that pupil “just right.” I had to remind my team (as I was reminded by my surgeons) that these people were paying upgraded fees for the use of the femto, ORA (Alcon), upgraded IOLs, etc; therefore, the added costs were easily covered within the collected fees.
The ASC facility that participates in premium procedures should always have the supplies on hand that are necessary to provide the surgeon (and ultimately the patient) with the tools necessary to get the best possible visual outcome.
2022 MIGS REIMBURSEMENT
As you likely have heard, the professional fee for implanting a trabecular meshwork (TM) stent during cataract surgery saw a dramatic reduction this year. What do these fee reductions mean for your practice?
These procedures have been a key revenue driver for many practices since Glaukos introduced the iStent in 2012. Prior to Jan. 1, 2022, surgeons and facilities billed for these joint services using the standard cataract code (CPT Code 66984) along with the new technology CPT Code 0191T. As this latter code is classified as “Category III” for emerging technology, administrators often had to get payer pre-authorization before consenting a patient for the procedure. Thankfully, this step will no longer be required in a vast majority of circumstances beginning this year, as the code assigned for the procedure transitioned to “Category I” with the new CPT Code 66991, which covers both the cataract procedure and TM stent implantation.
Unfortunately, this transition also resulted in reductions in the professional and facility fees associated with these services. Surgeons will now receive $663.57 for performing both procedures, which is only $134.73 more than the professional fee for standard cataract surgery.* Additionally, ASC facility fee reimbursement was reduced by more than $100.
PRACTICAL, PROFITABLE ALTERNATIVES
How can our practices continue to serve our patients and protect our financial viability? These reductions have left many practices seeking options to ensure that we are still providing patients the care they need while simultaneously weathering constantly escalating revenue challenges. Thankfully, there are alternatives — implant-free MIGS procedures with substantiated safety and efficacy in the form of goniotomy and canaloplasty.
Goniotomy, which is associated with the greatest 2022 professional fee of all MIGS procedures, earns the surgeon $1,078.17 per procedure. This represents additional income of $414.60 for each surgery. While the facility fee for these procedures is $795.19 greater for TM stents, this is more than offset by the fact that they often cost more than $1,000 over excisional goniotomy devices. (See Table 1 for a full comparison.)

|
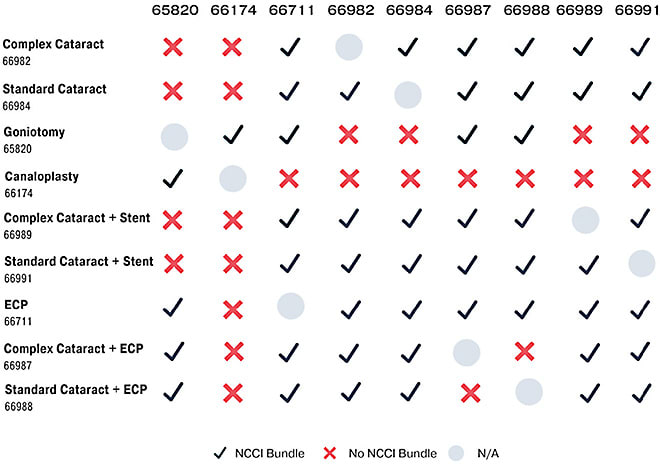
Table 2, based on material from CMS, demonstrates the 2022 bundles that have been implemented, including reimbursement differentials. This is a helpful aid to have available for your surgeons as well as your billing teams.
|
|
After reflecting the estimated cost of devices, this translates to an additional $600 of revenue per case for a surgery center. Goniotomy and canaloplasty procedures empower ASCs to continue to offer MIGS procedures to their patients and potentially preserve tens of thousands of dollars of revenue.
This type of review should be done on every case your ASC performs. It is critical to present the surgeons with the options that make sense without trying to step on toes when it comes to care.
In closing, make sure you negotiate your cost of goods with your industry partners. Your profitability per case is always important. OM
*All professional and facility fee amounts are based on CMS’ 2022 National Fee Schedule.









