The last 25 years have seen amazing advances in diagnostic tools, surgical instruments, medications and other treatments for ophthalmologic use. So what should we expect to see in the next 25 years?
Although no one has a crystal ball, based on what we’re seeing today, ophthalmologists reveal some of the next key innovations coming to market.
CATARACT/REFRACTIVE ADVANCES
Blake Williamson, MD, MPH, MS, a partner at Williamson Eye in Baton Rouge, La., foresees adjustable IOLs as the future of presbyopia. “In 25 years, ophthalmologists will rely less on preoperative biometry,” Dr. Williamson says. “We’ll still measure the eye, but most lenses will be adjustable and more exchangeable.” For example, he envisions having the ability to take a monofocal lens and using a laser to make it a multifocal in vivo. Adjustments could continue to be made over time as needed.
Mitchell A. Jackson, MD, founder and CEO of Jacksoneye in Lake Villa, Ill., highlighted four accommodating IOL technologies that are in the pipeline.
A fluid-based IOL by PowerVision, which was acquired by Alcon, is implanted into the eye’s capsular bag. It uses the eye’s natural accommodating response to transport fluid into the IOL. The fluid-based design creates a continuously variable monofocal lens, using the natural contraction of the eye’s muscles. The technology provides a continuous range of vision.
Atia Vision’s modular presbyopia-correcting IOL can focus between distant and near objects. Its lens technology features an accommodating base that’s responsive to the ciliary muscles, simulating the natural mechanism of the eye and fixed lens element that allows for subsequent refractive correction.
Another pipeline accommodating IOL is ForSight Labs’ Opira, which is a shape-changing IOL. The haptics are fixed in the capsulorhexis. The lens features a dynamic anterior surface and static posterior surface; it allows for toric correction and other postoperative adjustments, Dr. Jackson says. The lens features two compartments; the front is dynamic and accommodative, while the back is exchangeable.
LensGen’s Juvene is a fluid-filled modular dual design accommodating IOL implant. It’s designed to change curvature like the natural human lens to rejuvenate youthful vision to individuals with cataracts and presbyopia, Dr. Jackson says.
Another noteworthy development to address presbyopia and other eye conditions is Omega Ophthalmics’ Gemini Refractive Capsule (Figure 1). This device is placed in the eye and holds the intracapsular bag open.

“As of now, it’s difficult to exchange lenses postop, especially if you have already done a YAG laser capsulotomy,” Dr. Williamson says. “If you want to keep the bag open, you have to do a risky surgery.”
Along with acting as a space to implant new lenses as technologies improve, this device could serve as a storage unit to place medications for patients with glaucoma, dry eye or uveitis. It could also provide space for artificial intelligence (AI) devices and nano-devices that perform an array of functions, such as a sensor to check IOP.
“The intracapsular bag and posterior capsule are some of the most precious real estate in the eye’s entirety, anatomically speaking,” Dr. Williamson says.
Another development in the presbyopia space is Allotex’s TransForm Inlay, which uses real corneal tissue to create what is essentially a permanent, living contact lens or insert to treat hyperopia and presbyopia. “Synthetic inlays and onlays haven’t worked well; the viability of real corneal tissue is much higher,” Dr. Williamson says. Because allograft tissue is used, implants can be positioned right beneath the eye’s surface.1
Daniel S. Durrie, MD, board chairman of iOR Partners in Kansas City, Mo., predicts that refractive lens replacement will increasingly be performed before the formation of a billable cataract. “Patients are already having surgery at younger ages because lens implants are so advanced,” Dr. Durrie says. “In the coming years, more people will choose to get their lenses replaced when presbyopia sets in.” This would enable them to correct their refractive error and any astigmatism simultaneously, while preventing cataract formation.
And when surgeries are done to correct vision rather than remove cataracts, patients will rely less on their health insurance to pay for surgeries, Dr. Durrie says, which will lower health-care costs.
GENE THERAPY FOR RETINAL DISEASE
Gene therapy has been under development for more than 50 years; it’s not a new idea, says Daniel Kiernan, MD, FACS, a vitreoretinal surgeon with The Eye Associates in Sarasota, Fla. However, in 2017, the FDA approved Spark Therapeutics’ Luxturna (voretigene neparvovec-rzyl) for patients with Biallelic RPE65 mutation-associated retinal dystrophy. This was the FDA’s first approved gene therapy for a human disease, and 7-year follow-up data of the clinical trial participants have shown continued functional efficacy after a single treatment in each eye.
More gene therapies for retinal diseases are currently under development. “They have the potential to offer a much longer-lasting treatment for common causes of vision loss, such as macular degeneration and diabetic eye disease, than current and even imminent therapies demonstrate,” Dr. Kiernan says.
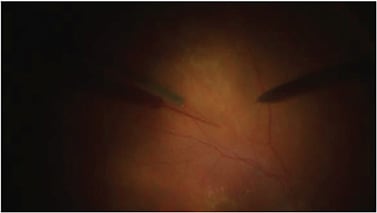
Regenxbio’s gene therapy product candidates deliver genes to cells that produce anti-VEGF molecules similar to ranibizumab to treat wet AMD using adeno-associated virus (AAV) vectors, which are non-replicating viral delivery vehicles that are not known to cause disease. The treatment involves performing a vitrectomy surgery and then administering a subretinal injection of the same AAV vector (Figure 2). Another study by the same company involves a suprachoroidal injection of an AAV vector to treat wet AMD.
Adverum Biotechnologies’ ADVM-022 uses a propriety vector capsid, AAV.7m8, carrying an aflibercept coding sequence under the control of a proprietary expression cassette. It’s administered as a single, one-time in-office intravitreal injection in each eye and is designed to deliver long-term efficacy, reduce the burden of frequent anti-VEGF injections and improve vision outcomes for patients with wet AMD.
DEVELOPMENTS IN AI
“AI is pushing the envelope for a lot of what we do in ophthalmology,” says Uday Devgan, MD, FACS, who is in private practice in Los Angeles and is a professor at University of California, Los Angeles.
For example, despite scientists and physicians developing many different algorithms to calculate an IOL’s power, these formulas typically have only an 80% accuracy rate at best.2
An AI approach to lens power calculations from the IOLcalc.com group, called the Ladas Super Formula 2.0, is reporting up to 95% accuracy.3 Headed by John Ladas, MD, PhD, the company is developing an algorithm to calculate an IOL’s power using AI data from more than 4,000 ophthalmologists who use IOLcalc.com .
A SHIFT TOWARD OFFICE-BASED SURGERIES
Ophthalmologists have realized increased revenue and improved efficiency by performing surgeries at ASCs rather than hospitals, Dr. Durrie says. Given this success, he foresees the next trend to be performing ophthalmic surgeries at an ophthalmologist’s office, rather than having a separate location and business.
This would be ideal for practices with 40 or fewer surgeries per month that can’t afford to operate an ASC. Ophthalmologists could still use the employees, equipment, waiting room and so forth for both surgeries and patient exams, Dr. Durrie says.
CONCLUSION
Reflecting on the developments to come, Dr. Kiernan borrows from the title of Kirk Packo’s, MD, FACS, 50th anniversary lecture at The Retina Society, saying that when we look back in another 25 years we'll realize again that we are standing on the shoulders of ophthalmic giants. OM
REFERENCES
- Allotex. Allotex — Allograft Inlays & Onlays. www.allotex.com . Accessed Sept. 30, 2021.
- Darcy K, Gunn D, Tavassoli S, Sparrow J, Kane JX. Accuracy of IOL power calculation formulas. CRST Europe. October 2020. https://tinyurl.com/4bu74yju . Accessed Sept. 30, 2021.
- Ladas J, Ladas D, Lin SR, Devgan U, Siddiqui AA, Jun AS. Improvement of Multiple Generations of Intraocular Lens Calculation Formulae with a Novel Approach Using Artificial Intelligence. Transl Vis Sci Technol. 2021;10(3):7.








