Lens allows surgeons to finalize vision acuity after surgery

Getting RxSight’s Light Adjustable Lens (LAL) has been a life-changing experience for my patients. Many can now see and function without eyeglasses for the first time in decades. They’ve ranked being able to see clearly among their happiest moments in life, right up there with getting married or having a baby. Some have even been in tears over the astounding results.
What differentiates RxSight’s LAL from other “fixed shape” intraocular lenses (IOL) is that it’s the first IOL that can be adjusted postoperatively to improve uncorrected visual acuity. Instead of trying to figure out or guess what IOL power is best for a patient, the lens allows surgeons to first implant the lens and then change the power afterward. The refractive surprise disappears.
PERSONAL SUCCESS
My first experience with RxSight’s LAL was back in 2012, when I participated in FDA clinical trials. In the last 12 months, I have implanted the lens in almost 200 patients, and none of them have needed glasses for distance vision. Less than 10% of patients required glasses for reading and other close-up tasks, such as computer work. In the first 160 eyes I implanted, 80% could see 20/20 or better for distance and read 20/20 or better without glasses.
These results make the LAL the most accurate IOL in the world.
The LAL is indicated for patients who have a cataract or a corneal astigmatism that is at least 0.50 diopters, or both conditions. Patients who don’t have either condition, but aren’t candidates for LASIK or photorefractive keratectomy surgery due to cataracts or presbyopia, are also good candidates. Patients should not have any significant preexisting macular disease and have good visual potential. Additionally, their pupil needs to dilate greater than 6.5 mm, which I check before scheduling the surgery.
HOW IT WORKS
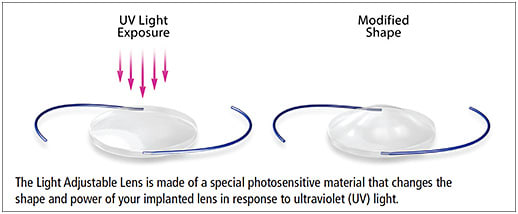
The LAL is a three-piece silicone IOL with additional silicone macromers (microscopic particals) inside the lens. These movable macromers polymerize together with a photo-active component when exposed to UV light delivered by RxSight’s light delivery device (LDD). During the first 48 hours after a light treatment, the macromers move in the IOL. This movement changes the IOL’s shape, and either increases or decreases the optical power and treats astigmatism. The LAL is approved for adding or subtracting up to 2.0 D of sphere and up to 2.0 D of astigmatism per light treatment.
The LAL can be adjusted up to three times to fine tune distance, intermediate, or near vision. Additional patterns, such as extended depth of focus to treat presbyopia, are also possible and are currently undergoing an FDA trial.
The procedure is performed like any other cataract surgery. If a patient has an astigmatism, you don’t have to make any special markings on the cornea to mark the axis of astigmatism for use with a toric or multifocal IOL. After surgery, the patient heals for three weeks and then returns to the office to have their lens shape adjusted. After a patient’s eyes are dilated, we place their chin into the LDD (a slit lamp with an integrated UV light delivery device) and I push a foot pedal to activate the LDD. It focuses a blue light on the lens for about 60 seconds, which activates the movement of the macromers and monomers. This movement changes the lens shape over the next 24 to 48 hours.
Patients try out their new lens shape for one week. Then, I evaluate their distance, intermediate, and near vision, and change the lens shape again to improve their desired results. This method of obtaining the patient’s feedback allows the patient to dictate the visual results that work best for their individual needs.
We can change the shape of the IOL up to three times. With one week between adjustments, this timeframe allows the patient to try the new lens shape in the real world and choose the ideal shape before I lock in the IOL with a final light treatment so no more changes in shape can occur. Once locked in, the lens won’t drift or change. I have followed patients for eight years, and their refraction has been stable over time.
RISKS AND POTENTIAL SIDE EFFECTS
Potential risks associated with LDD light treatments include mild, temporary alterations to color perceptions; temporary scratchiness, irritation, or dryness to the front part of the eye; and activation of a herpes eye infection. Certain medications can cause patients to be extra-sensitive to light, so patients should stop these medications before any light adjustment.
Longer-lasting and serious adverse events related to UV light exposure are possible. Fortunately, I have not seen or heard of any of these types of complications. Following surgery, patients must wear special UV-protective glasses during all waking hours for about four to five weeks and comply with their doctor’s schedule of LDD light treatments.
A patient's failure to wear the UV-protective glasses can result in unwanted exposure of the IOL to the sun’s UV light. This exposure could cause unpredictable changes to the IOL shape, producing unwanted visual changes or loss of vision quality. This may require a second surgery to remove the LAL from the eye and replace it with a new one.
There is a small chance that a patient’s vision could worsen or that they may require additional surgery, a risk that exists with any cataract surgery. The risk of needing additional surgery is actually less with the LAL compared with a fixed-shape IOL. This reduction is because the most common reason for additional surgery is that a patient isn’t happy with their refractive outcome. With the accuracy of the LAL, the need for surgery to improve refractive outcomes has been eliminated in my practice.
CLINICAL STUDY FINDINGS
FDA approval in 2017 was based on results of a U.S. randomized, pivotal study1 comparing the LAL to a commercially available monofocal lens in 600 patients with preexisting astigmatism at 17 investigational sites. Patients receiving the LAL, followed by light treatment with the LDD, achieved UCVA of 20/20 or better at six months postoperatively at approximately twice the rate of patients receiving a monofocal lens.
Almost 92% of the LAL patients also achieved a result that was within 0.50 D of target manifest refraction spherical equivalent, which is similar to the refractive accuracy seen in recent LASIK studies. Study safety parameters were based on a comparison to the safety and performance endpoints for intraocular lenses (ISO 11979-7), and results showed that 100% of study eyes had a best corrected visual acuity of 20/40 or better at the 6-month postoperative visit. The approved device allows for correction of up to 2 diopters of postoperative sphere and/or -0.50 to -2 diopters of residual postoperative refractive cylinder.
My most recent data showed that 80% of patients achieved distant vision that was 20/20 or better, and near vision J1 or better without the use of glasses.
I plan to present these findings at the next AAO and ASCRS meetings.
FOOD FOR THOUGHT
More work is involved when using RxSight’s technology, but if you’re a surgeon looking for the best results, this will give you exactly that.
You already have the skills to implant the LAL; the only thing you’ll need to learn is using the LDD—which is as easy as using a YAG laser—so the learning curve is minimal.
I think this is the most accurate IOL that the world has ever seen. It’s the future of how we will be able to come up with the most perfect lens shape for each patient. There are probably designs we haven’t even thought of yet for IOL technology which would push the limits of what we currently believe is the best visual potential for the human eye. ■
Reference
- Summary of safety and effectiveness data. Available at: https://www.rxsight.com/media/smdgdhqa/rxsight_ssed.pdf . Accessed March 1, 2021.








