Lid margin disease has long been the bane of eye-care professionals. This disease has presented us with frustrated patients who were difficult to successfully treat because they suffered from a condition that was not well understood.
More recently, we have come to better appreciate the importance of lid hygiene and the impact of meibomian gland health on tear film stability. Consequently, we have started to recommend lid wipes, at-home cleansers and in-office procedures. However, due to a lifelong commitment to prescribed treatments, many of our patients are still searching for a magical cure to make their disease go away.
The effects of this indolent disease, such as endophthalmitis, are even more pronounced in our postop cataract patients. They expect a return to their vision from years gone by, but their actual postsurgical results fail to meet their high expectations. We often share in this frustration — our inability to meet or exceed visual expectations, refractive surprises or worsening ocular surface disease are the typical underlying culprits.
However, those days may as well be behind us. Here, I’ll discuss the role of biofilm in lid margin disease and how it affects strategies to treat these patients.
BIOFILM’S ROLE
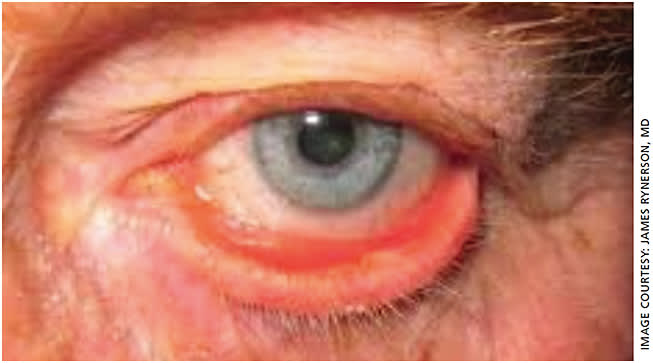
Thanks to a theory of dry eye disease proposed by James Rynerson, MD, we may finally have a better understanding of this ubiquitous disorder.
This theory is that it is simple and easy for our patients to grasp; it explains most clinical presentations of lid margin disease from madarosis to aqueous insufficiency. And, once understood, it makes lid margin disease easy to treat.
It turns out the cause of this way-too-common malady is biofilm, a basic substance that has been known to the medical community for decades. Biofilm, also known as plaque, is what dental hygienists remove from our teeth. It makes chronic wounds chronic, allowing bacteria to resist the most determined effort to eradicate them. A full discussion of this theory and subsequent disease that Dr. Rynerson refers to as the DEBS (Dry Eye Blepharitis Syndrome) can be found in a 2016 white paper published in collaboration with Dr. Hank Perry in Clinical Ophthalmology.
Biofilm is nothing new to eye doctors. We see it every day in our clinics but use a non-medical term to describe it — scurf, a benign-sounding term that hides its true nefarious intent and obscures the long-term damage that may result if not removed. Most eye-care providers continue to disregard biofilm at their patients’ peril.
According to Dr. Rynerson, biofilm is more than just crusting on the lids and lashes. It is a nearly invisible layer that covers the entire lid margin. Over time, biofilm seals off the meibomian gland orifices and eventually creeps into every gland structure within the eyelid, from the lash follicles early in life to the lacrimal glands late in life. This makes ocular surface disease chronic and progressive. Unless addressed, it leads to the slow, insidious destruction of whatever the biofilm invades — lash follicles, glands of Moll, goblet cells, meibomian glands or the lacrimals. In turn, it results in unhappy patients with less than ideal refractive surgical outcomes.
A critical component of Dr. Rynerson’s theory is referred to as Quorum-Sensing Gene Activation, which was discovered by Dr. Hastings at Harvard in 1968. This is what makes the biofilm relatively benign in early life but results in chronic inflammation much later in life once the biofilm “matures” and allows genes to activate. These genes produce the virulence factors (toxins) responsible for the inflammatory changes, the underlying culprit of dry eye disease.

HOW WE CAN ADDRESS THE BIOFILM
Once armed with the understanding that dry eye is due, in part, to a bacterial biofilm, something that all bacteria produce to survive their environment, then the solution becomes clearer. Remove the biofilm! Remove it early, and remove it often. Remove it every 6 months in young patients to prevent lid margin disease, just like dentists do for prevention of gingivitis. Remove it before cataract surgery for a healthier lipid layer, a more stable tear film and to obtain more reliable pre-surgical measurements. And, remove it in every dry eye patient — whether evaporative, aqueous insufficient or a combination — to save the remaining eyelid glands.
The biofilm can be removed via microblepharoexfoliation (MBE) with a handheld device called BlephEx. This device is simple to use either by the physician or a trained technician as an in-office cash pay treatment. Its disposable tips are dipped into a lid cleansing product, such as hypochlorous acid, then moved along the lash base to mechanically remove the built-up debris.
Performing the 10- to 15-minute MBE at the office not only avoids the potential compliance issues seen with at-home remedies, it often works synergistically with recommended home remedies.
PATIENT EDUCATION
A physician has to be prepared to invest a fair amount of time on the front end educating patients about biofilm-induced dry eye. Education is a critical component for patient acceptance of a chronic, progressive, obstructive gland disease. It also helps with acceptance of the non-insurance covered procedures. Because the biofilm is easy to explain and easy for patients to understand, most eye-care providers get little push back that MBE is a private-pay procedure. Commit to spending a little extra time explaining details to patients and staff, and everyone will reap rewards down the road.
MBE AND SUPPLEMENTAL TREATMENTS
Educating patients on the importance of treatment before the symptoms ensue is key. Using the dental hygiene analogy, MBE is comparable to the “deep clean” performed by the professional, and at-home remedies are comparable to daily brushing and flossing. So, recommend patients follow up the in-office BlephEx MBE with hot moisture masks and/or with a handheld lid margin cleansing device at home.
The patients who benefit most from MBE are dry eye patients who have already suffered damage to their tear glands and pre-cataract surgery patients to ensure better preop measurements. When a heat and express technique such as iLux (Alcon), TearCare (Sight Sciences) or LipiFlow (J&J Vision) is paired with MBE, patients feel the difference. Perform these heat and express procedures immediately following the BlephEx on the same day. Most patients feel an improvement from their chronic suffering and readily return for their repeat treatments. Once the tear film is stabilized, MBE is typically repeated every 6 months, and meibomian gland heating and expression procedures are usually recommended on an annual basis.
The total treatment time for the combination approach is about 30 minutes. Typically, patients are asked to return in 2 to 4 weeks to assess their response to the MBE, or MBE plus a heat and expression treatment. If planning for upcoming cataract surgery, the combo treatment (BlephEx followed by a heat and express procedure) should ideally be performed at least 6 weeks before surgery, according to Dr. Rynerson. Depending on the ocular surface disease severity, some patients may take longer and require multiple treatments before adequate optimization is achieved and the surgeon is comfortable with the repeatability of the tear breakup time, placido disc images and ocular staining scores.
The charge for BlephEx is around $250, and a heat and express procedure can vary from $450 to $850. Most practices that offer in-office dry eye treatments, make CareCredit financing available for those who need it. According to Dr. Rynerson, more than 80% of his patients readily agree to have the combination treatment of BlephEx and iLux, understanding that, if performed on the same day, removing the “Saran Wrap” covering the meibomian gland orifices aids in expressing the impacted meibum from within their meibomian glands.
CONCLUSION
It is time we took biofilm lid margin disease seriously. It slowly wreaks havoc on our patients’ tear film and causes much consternation and disappointment after an otherwise pristine cataract surgery. Your patients deserve the incredible benefits that biofilm removal provides.
Within a few weeks, pretreatment with a combination of MBE plus a heat and expression procedure may achieve tear film homeostasis with reliable measurements for successful cataract surgery and astigmatism management planning. Consequently, “20/unhappy” may be significantly reduced. OM









