As a cataract and cornea/external disease specialist, I make it a point to attend as many major ophthalmology conventions as I can. When visiting the exhibit halls, I often feel like a kid walking into FAO Schwarz toy store in New York City. Everywhere on the exhibition floor, there are so many great new “toys” to help diagnose and treat the ocular surface, cornea and cataracts, such as femtosecond lasers, preoperative imaging systems and optical coherence tomography (OCT).
At many booths, I’m sorely tempted to pull out my wallet. But, as much as I revel in all the “latest and greatest” offerings, it is not always possible to have them all. When it comes to furnishing our practice with the latest technology that we need to stay competitive and on the “cutting edge” of cataract and refractive surgery, we have only so much capital to spend. As a result, I strive to take the same deliberative approach to acquiring new technology as I did when I opened my practice three decades ago.
Trained as a specialist in cornea, external disease and refractive surgery, I opened my practice in 1991, relying mostly on preowned equipment because I did not have the money to spend on anything new. At that time, I needed to be selective; as much as I may have wanted, I could not purchase equipment just because of the prestige it might bring my practice. I had to look at what each piece of technology would add to my practice and how that technology could make me a better diagnostician and surgeon.
Our practice has grown considerably since then: we now have three locations across St. Louis and eastern Missouri. Including me, our office comprises 46 staff and clinicians, including two cataract and corneal disease specialists and two optometrists.
Still, whenever considering the acquisition of new cataract surgery technology, I always ask myself the same three questions I did when I started.
1. DOES IT IMPROVE PATIENT CARE?
We invest in new technology primarily when it makes us better clinicians and improves care.
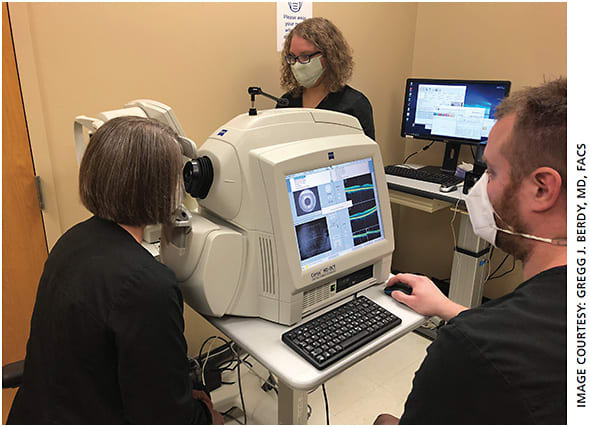
For example, a small percentage of cataract patients present with an epiretinal membrane, retinal swelling or an occult subretinal neovascular membrane. Conditions such as these can lead to sub-optimal results with multifocal IOLs. Oftentimes, these diseases can’t be seen with direct visualization using an ophthalmoscope. But OCT enables us to identify these diseases and explains why we made the decision 7 years ago to acquire a swept-source OCT unit.
Our practice does not treat retinal or macular diseases, but my associates and I recognized that many of our cataract patients want the newer multifocal IOLs, and so we now use our swept-source OCT to evaluate every cataract patient. If we find something amiss, we bill for the test. If not —about 90% of the time — we do not bill. For us, OCT screening is essentially a pro bono service, but if we are planning to implant a multifocal IOL, we want to make sure the patient’s retina is perfect. If there is an abnormality in the retinal findings, we will recommend a different IOL.
2. DOES IT IMPROVE OUR PRACTICE?
We also invest in new technology when it makes our practice better. EHR systems are a case in point. When I was first approached about EHRs about 10 years ago, I was skeptical. Our paper-based system worked just fine, and it was hard for my partner to convince me an EHR would improve our efficiency, make us better clinicians and help us capture more revenue.
Ultimately, the federal government/Medicare required all medical practices to implement EHR systems, and I had no choice but to go along. We experienced growing pains early on, and implementing the system was challenging and time consuming. But, ultimately, EHR dramatically improved our operations. For example, instead of simply noting that a cornea appears “clear with some staining,” we can provide more detail regarding our slit lamp findings, which makes our records more complete and helps us to capture more diagnoses for billing. Our EHR also enables us to capture images; as a result, we can show cataract patients how clouded their lens is and help to better explain why the lens needs to be replaced.
We also use Meibom Pens (JFC) to perform meibography, which is helpful in the diagnosis of and following treatment for meibomian gland dysfunction/ocular surface diseases. Since these conditions can affect patient outcomes, it is very important to document prior to cataract and refractive surgery.
In the surgery center, femtosecond lasers are vastly important to outcomes with respect to cataract surgery. Femto lasers are very large investments — between $300,000 and $500,000 — but they are exceptionally beneficial to obtaining better outcomes for patients receiving toric or multifocal IOLs. Our current surgical group trialed lasers from three companies; there were pros and cons to all of them, and we have had the one we ultimately chose for more than 5 years. It has vastly improved our cataract procedures. Capsulotomies are incredibly more accurate and reproducible; by softening up the nucleus, the laser shortens surgical time, which improves safety, and gives better optical results. Another example is Optiwave Refractive Analysis (ORA, Alcon). This technology provides real-time measurements of the eye during cataract surgery; it helps to ensure that nearsightedness, farsightedness or astigmatism is appropriately corrected during cataract surgery. These devices can cost upwards of $100,000.
Advice for acquiring new technology
- Be willing to fail. Like anything else in life, medicine is the practice of an art, and you will make mistakes when it comes to purchasing technology. But, hopefully, you will learn from them. It helps to be comfortable with experimenting and risking failure.
- Listen to colleagues (no matter their age). My partner, Ranjan Malhotra, is 15 years younger than I am. But even in that small difference in age, he is more comfortable than I am when it comes to accepting early advances in technology. I have always tried to keep an open mind and listen to others who might see the usefulness of a technology that I might not have seen. Sometimes listening and taking their advice can be advantageous.
- Do your due diligence. Research everything before you buy. Read the peer-reviewed journals and trade magazines. Pay attention to what your peers are saying, and make sure it all makes sense for you and your practice. You need to know what you’re getting into before you purchase a piece of equipment — how you’re going to utilize the technology, how you’re going to pay for it and how it will add value to your practice and patient care. It’s easy to get overwhelmed by salespeople who pitch “the latest and greatest” and then jump in instead of should thinking it over.
- Believe in yourself. One of the things I learned when I first went into practice is the importance of investing in yourself — and that includes the equipment in your practice. Almost three decades later, I still have the same energy and enthusiasm, because I love what I do and I see the value in what my practice and I bring to people. New technology enhances that.

3. DOES IT MAKE FINANCIAL SENSE?
This brings us to financial considerations. Regardless of how helpful a new technology may be to cataract surgery, a practice must have the financial wherewithal to acquire it. For the first 10 years of our practice, we took out several $100,000 loans to help finance equipment. Loans can be a good way to build a practice, especially when interest rates are low. But now we try to purchase equipment out of capital on hand. Ideally, the equipment should also be reimbursable by Medicare or private insurance.
New technology must also deliver a solid return on investment (ROI) within a reasonable amount of time. How much time is a matter of individual preference.
Depending on the technology in question, it can take 6 months to a year or more for equipment to pay for itself. At the end of the day, ophthalmology practices are businesses, and decisions should be made with that thought in mind. We strive to give high-quality care and practice excellent medicine, but we also have to practice fiscally responsible medicine.
BETTER PATIENT CARE = BETTER ROI
Still, there is more than a financial component to ROI. It’s true that large investments in technology can take months or years to recoup through such steps as increasing procedure costs. But ROI can, and should, also be calculated in terms of its impact on treatment accuracy, safety and patient care.
In other words, the payback to the surgical center is also reputational, in that investments in advanced technologies can bring about better outcomes, which can lead to higher patient satisfaction and higher referrals.
When eyeing new equipment, it isn’t always easy to balance the needs of your surgery center, patients and finances. But, ultimately, our primary goal as cataract and refractive surgeons should always be to invest in technology only when it makes us better surgeons and provides our patients with the best possible treatment. If our patients do well, then hopefully they will tell their friends and refer more patients to us.
And that’s always a good ROI. OM









