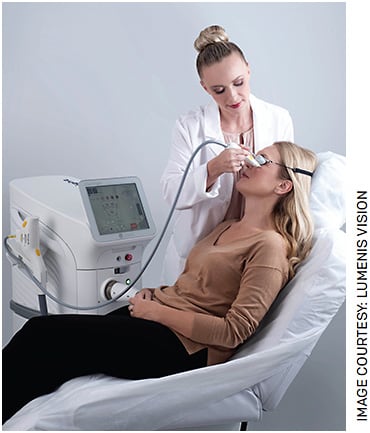
Lumenis’ OptiLight uses intense pulsed light technology to relieve symptoms.
For patients with dry eye disease due to meibomian gland dysfunction (MGD), a new device that uses pulses of light to improve meibomian gland function may provide significant relief.
The Lumenis OptiLight is indicated for patients with moderate to severe signs and symptoms of dry eye disease due to MGD and with Fitzpatrick skin types I-IV. Approved by the FDA earlier this year, the system is designed to provide a consistent, precise and controlled light-based treatment, the company says.
Specifically, the OptiLight uses intense pulsed light (IPL) technology created to address the inflammation of dry eye disease due to MGD. The OptiLight is intended to be applied as an adjunct to other treatment modalities. Lumenis says it is the first and only such device to receive FDA approval for improving signs of dry eye disease.
CONNECTION TO DERMATOLOGY
Lumenis invented IPL technology about 20 years ago for use in dermatology to treat conditions such as rosacea, says Itay Mayer, managing director, Lumenis Vision, based in Tel Aviv. One early adopter was Rolando Toyos, MD, medical director and founder, Toyos Clinic, with offices in Memphis, Tenn., Nashville, Tenn., and New York City. In the late 1990s, he treated rosacea patients with IPL. A few of his patients told him that the treatment was helping not only their rosacea, but also improving their dry eye.
Since then, Lumenis has worked on tailoring OptiLight, its IPL technology innovation, to treat dry eye disease and developed clinical evidence for the safety and efficacy of OptiLight for treating dry eye. In 2017, a 3-year retrospective study on patients who received IPL found clinically significant improvement in tear breakup time. Then, a Lumenis multi-center, double-blinded, randomized controlled FDA trial showed that Lumenis IPL with Optimal Pulse Technology significantly improved tear breakup time, meibum quality and meibomian gland expressibility without serious adverse events.
WORKING WITH WAVELENGTHS
The OptiLight uses a xenon flash lamp that generates specific wavelengths of light. A wavelength of 600 nanometers and greater “does the most to improve the meibomian gland function,” explains Dr. Toyos.
He notes Lemp et al showed in 2012 that more than 80% of patients with dry eye have MGD. The OptiLight addresses dry eye disease due to MGD in various ways, according to Dr. Toyos. First, if a patient has abnormal blood vessels on the epidermis, the device will close those vessels, which decreases the amount of inflammatory mediator being fed to the meibomian glands. Second, these dry eye patients are producing inflammatory cytokines on the skin, and IPL decreases the number of inflammatory mediators on the skin. Third, it provides photobiomodulation, in which the light is stimulating the mitochondria of the meibomian gland cells to produce better meibum.
PATIENT SELECTION
Keeping in mind that the goal is to reduce inflammation, Dr. Toyos will use anti-inflammatory drops as a first-line treatment in a young patient with mild dry eye disease. If the drops don’t improve the dry eye, he then uses OptiLight. For a patient with moderate to severe dry eye disease, or who is older, Dr. Toyos will use both an anti-inflammatory drop and OptiLight.
“There are multiple scenarios among dry eye and MGD patients where we offer OptiLight,” says Laura M. Periman, MD, founder and director of dry eye services and clinical research at Periman Eye Institute in Seattle. “One is patients who desire a drug-free, drop-free approach. Second is patients who are not happy with their level of control. Another is patients who are not experiencing sufficient relief from their current prescriptions and therapy.”
While no cure for dry eye and MGD currently exists, she notes that the OptiLight “not only improves dry eye and MGD, we’ve also observed that it decreases the patient burden of the disease.”
SPEEDY PROCEDURE
Dr. Periman estimates that the treatment could take as little as 3 to 5 minutes if the patient has been already prepped for the procedure “I’m really impressed at how quickly the treatment can be done,” she says.
The device offers two handpieces. The IPL handpiece is designed to treat wider areas, while the OPT handpiece is designed to deliver energy to smaller facial contours, such as those around the eyelids and the orbit. Prior to the treatment, the patient’s cornea must be protected with corneal shields or external stickers or goggles.
Treatment with OptiLight typically entails two passes with the smaller OPT handpiece and then two passes with the larger IPL handpiece in areas not already treated.
The device offers preset settings. “You just pick the right Fitzpatrick skin type, and it will give you suggested parameters,” says Dr. Toyos.
The treatment protocol calls for four treatments, spaced 2 to 4 weeks apart, followed with meibomian gland expression after each treatment. “What you’ll find is with the first two treatments, you get a little bit of increase in tear breakup time and symptom relief. But then with the third and fourth treatments, you get exponential improvement in tear breakup time and symptom relief,” Dr. Toyos explains.
Once a treatment is completed, expression is critical. “IPL generates heat in the dermis that melts secretions and opens up the glands so that you can express these glands much easier and get this abnormal meibum out,” he says. “Now you have a clear path for normal meibum to come out and be part of that fatty layer of the tear film as it should be.”
Patients will need maintenance visits at intervals from 3 months to 1 year, depending on age and the severity of MGD.
NO GETTING AROUND IT
Busy cataract or LASIK surgeons who feel they don’t have time to deal with dry eye, Dr. Toyos says, should keep in mind that performing these other procedures without treating patient’s dry eye means the procedure may well fail.
“IPL is a huge tool in treating these patients and improving their vision,” he says. OM
Disclosures: Dr. Periman is a speaker for Lumenis. Dr. Toyos is a consultant for Lumenis.








