Our patient is a 60-year-old male with a past medical history of hypertension, diabetes and tobacco use, who was referred by an outside ophthalmologist for a second opinion of a pigmented spot in his left eye. He first noticed the lesion approximately 1.5 years ago and presented to an optometrist 6 months after first noticing it. The optometrist sent the patient to the referring outside ophthalmologist. Notably, the patient’s family history was significant for cancer in multiple family members, including choroidal melanoma in his paternal grandmother.
THE OCULAR EXAM
We noted the following on the patient’s eye exam:
- Distance visual acuity with correction: 20/20 OD, 20/25+1 OS
- Pupils: PERRL OU, no APD
- IOP: 12 mm Hg OD, 15 mm Hg OS
- Extraocular motility: Full
- Confrontation to visual field: Full to finger counting OU
- Slit lamp exam: Within normal limits OD.
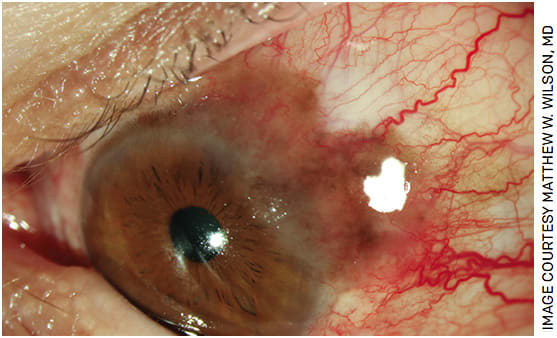
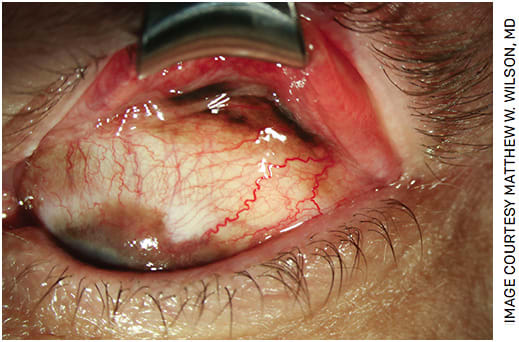
Slit lamp exam of the left eye, however, was significant for the following (Figure 1): 2+ conjunctival injection, an elevated limbal based pigmented lesion with extension of the lesion onto the cornea at 12-4 o’clock and scattered residual bulbar pigment from 10-6 o’clock. The lesion extended in the superior temporal direction from the limbus. Double eversion of the left upper eyelid revealed pigment in the superior fornix abutting the cul-de-sac (Figure 2).
The differential diagnosis of conjunctival melanocytic disease includes: congenital freckle, racial melanosis, primary nevus, primary acquired melanosis (PAM) with atypia, PAM without atypia, extra-scleral extension of a ciliary body melanoma or secondary pigmentation.1
WORK UP AND DIAGNOSIS
Wide local excision of the pigmented areas was performed. Adjuvant cryotherapy was applied to surrounding conjunctiva and sclera base. An amniotic membrane graft was used to reconstruct the ocular surface. Findings on histology were consistent with a focal melanoma extending onto the cornea and scattered PAM with atypia (melanocytic intraepithelial proliferation) inclusive of the superior fornix.
PAM WITH ATYPIA AND CONJUNCTIVAL MELANOMA
Unlike PAM without atypia, PAM with atypia is a precancerous, rather than benign, lesion. It is characterized histologically by nesting of atypical melanocytes and pagetoid extension.2 Conjunctival melanoma, which is malignant, most commonly arises from PAM with atypia, although it can also arise de novo or from nevi. It is characterized histologically by subepithelial invasion of melanocytes.2 Pathologic features on histology include a high mitotic rate, angiolymphoid invasion, positive surgical margins and increased thickness. Once diagnosis is confirmed on histology, PET-CT scan, abdominal imaging with CT, MRI or ultrasound and brain MRI are indicated to look for metastases.3 The cervical lymph nodes, brain, lungs and liver are the most common metastatic sites.3
The mainstay of treatment for conjunctival melanoma is wide local excision using a dry-field “no touch” technique. This avoids contact of surgical instruments with cancerous cells to minimize the risk of seeding them in the subconjunctival space, which increases the risk of disease recurrence.4,5 The surgery should be done at an ASC or hospital. Communication with the pathologist regarding orientation of the biopsy and fixative applied should be completed beforehand. After the lesion is excised, adjuvant double freeze thaw cryotherapy is applied to the adjacent conjunctiva and the scleral bed of all margins and visible areas of pigment dispersion.3 Amniotic membrane grafting is then used to repair the defect in the conjunctiva.3
Finally, patients with PAM with atypia commonly undergo adjuvant treatment with a topical chemotherapy, most commonly mitomycin C (MMC).6 Side effects of MMC are usually transient and include conjunctival injection, tearing and keratoconjunctivitis.7 While long-term complications are less common, they tend to be more serious and include limbal stem cell disease and keratopathy.7 MMC is administered on an intermittent schedule to prevent the depletion of limbal stem cells.8
BACK TO OUR PATIENT
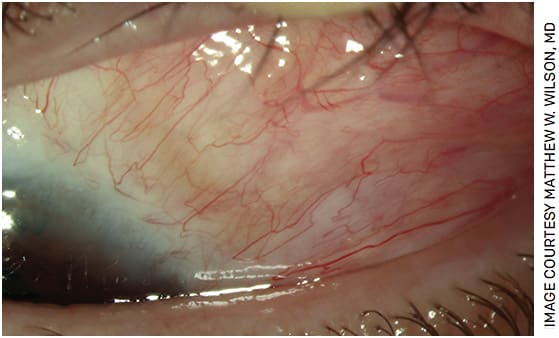
MRI and PET-CT scan performed on our patient were negative for metastases. At the 3-week postoperative visit, no residual disease was noted (Figures 3 and 4). However, our patient experienced foreign body sensation in his left eye. Artificial tears were prescribed. All biopsy margins were positive for PAM with atypia. One drop four times daily of topical MMC 0.04% was initiated on an intermittent schedule of 1 week on followed by 1 week without it for three cycles.

At the 3-month postoperative visit, the patient reported that he had experienced redness and swelling during the last 4 days of his cycles and still experienced a mild foreign body sensation. Significant (4+) punctate epithelial erosions of his left cornea were noted on slit lamp exam; however, no recurrence of conjunctival melanocytic disease was observed. The patient was instructed to increase his use of artificial tears, and loteprednol and prednisolone acetate were prescribed.
At the 5-month postoperative visit, the patient’s left eye irritation had improved; steroid eyedrops were no longer needed. His visual acuity was 20/20 in the treated eye. The amount of punctate epithelial erosions on slit lamp exam was trace.
As of the writing of this article, the patient’s eye exam has remained free of clinical signs of recurrence for 10 months postoperatively. He will be monitored for signs of disease recurrence for life.
TAKE-HOME POINTS
When examining a patient with a conjunctival pigmented lesion under the slit lamp, it is crucial to double evert the upper eyelid to check the fornix for pigment. Early referral and prompt initiation of MMC are important for minimizing risk of local recurrence. Patients with PAM with atypia require lifelong surveillance. OM
REFERENCES
- Kenawy N, Lake SL, Coupland SE, Damato BE. Conjunctival melanoma and melanocytic intra-epithelial neoplasia. Eye (Lond). 2013;27(2):142-152.
- Jakobiec FA, Folberg R, Iwamoto T. Clinicopathologic characteristics of premalignant and malignant melanocytic lesions of the conjunctiva. Ophthalmology. 1989;96(2):147-166.
- Vora GK, Demirci H, Marr B, Mruthyunjaya P. Advances in the management of conjunctival melanoma. Surv Ophthalmol. 2017;62(1):26-42.
- Shields JA, Shields CL, De Potter P. Surgical management of conjunctival tumors. The 1994 Lynn B. McMahan Lecture. Arch Ophthalmol. 1997;115(6):808-815.
- Shields JA, Shields CL, De Potter P. Surgical management of circumscribed conjunctival melanomas. Ophthalmic Plast Reconstr Surg. 1998;14(3):208-215.
- Fernandes BF, Nikolitch K, Coates J, et al. Local chemotherapeutic agents for the treatment of ocular malignancies. Surv Ophthalmol. 2014;59(1):97-114.
- Ditta LC, Shildkrot Y, Wilson MW. Outcomes in 15 patients with conjunctival melanoma treated with adjuvant topical mitomycin C: complications and recurrences. Ophthalmology. 2011;118(9):1754-1759.
- Wilson MW, Hungerford JL, George SM, Madreperla SA. Topical mitomycin C for the treatment of conjunctival and corneal epithelial dysplasia and neoplasia. Am J Ophthalmol. 1997;124(3):303-311.









