Perimetry is an indispensable tool to help both diagnose stage and monitor glaucoma. For the past several decades, we have relied heavily on this technology to determine the functional status of our glaucoma patients — the number of which have grown nearly exponentially and is projected to continue on this trajectory.1
Despite perimetry’s obvious benefits in helping us deal with this influx, its drawbacks as a time-intensive and subjective test are well documented. Doctors who see a high volume of glaucoma patients know first-hand how the visual field machine can create a bottleneck in patient flow.
This problem takes on a greater level of urgency in light of the current pandemic, where minimizing wait times and office crowding are critical.
This article will review the recent updates in testing algorithms and novel technologies that may improve throughput and patient flow.
MAINSTREAM PERIMETRY
Early perimeters quickly made their mark
The first automated perimeter was the Octopus 201 (Haag-Streit), released in 1974. However, computerized perimetry did not gain mainstream acceptance until a decade later with the release of the Humphrey Field Analyzer (HFA, Carl Zeiss Meditec) in 1984. Since then, the HFA has been the mainstream perimeter and has been used in essentially all of the landmark glaucoma trials.
The early iterations of HFA utilized the Full Threshold and FASTPAC strategies and had prolonged test times, which respectively took around 15 and 10 minutes per eye. The immense time commitment in obtaining a visual field limited the number of tests that could be performed; further, patient fatigue often negatively impacted reliability.
SITA cuts test times
The Swedish Interactive Testing Algorithm (SITA) was introduced in the late ‘90s and used complex predictive mathematical models to reduce testing times dramatically. SITA-Standard and SITA-Fast respectively cut testing times to roughly 7 and 5 minutes. Though the rapid testing strategies tended to underestimate scotomas, reproducibility was not compromised, so our ability to accurately detect glaucoma progression was maintained.2
In the 30 years since SITA was introduced, we have learned a great deal about detecting field progression. The Ocular Hypertension Treatment Study (OHTS) showed that presumed field progressions were frequently false alarms warranting repeat testing. Statistical modeling performed by Chauhan BC et al revealed that six field examinations a year were necessary to detect rapid progression (-2dB/year) with 80% accuracy, with a much higher number needed to detect slower progression rates.3 While most glaucoma specialists would agree that a high frequency of testing would be ideal, the prospect of increasing the frequency of fields several-fold in an already resource-strained system is impractical for many.4
Octopus perimeter
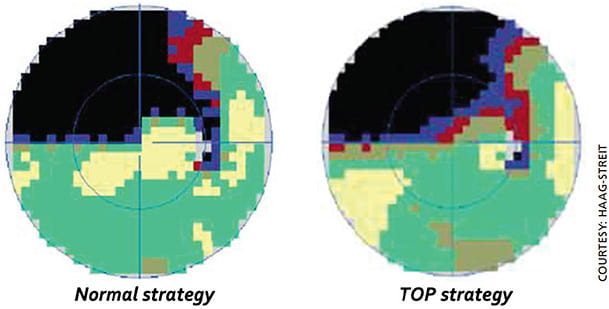
The Octopus perimeter has gone through an evolution of testing strategies in parallel with the HFA. The Octopus’ Normal and Dynamic strategies were analogous to the HFA’s Full Threshold and FASTPAC with comparatively similar testing durations. Tendency-Oriented Perimetry (TOP) was introduced in the late ‘90s, just a few years following the release of SITA.5 The TOP strategy takes advantage of the assumption that thresholds at each location are interrelated with its nearby locations for glaucomatous defects. Compared to bracketing strategies in which each test point is interrogated multiple times, the TOP strategy directly tests each point only once, with answers given at surrounding points modifying the sensitivity outcome.
The drastic reduction in test stimuli allows the test to be completed in 2 to 3 minutes per eye. Though the rapid testing algorithm with TOP affects the accuracy of testing, causing scotomas to tend to appear shallower and with softer edges, reproducibility is maintained (Figure 1).5
Another key feature of the Octopus perimeter is its fixation control features. Fixation loss is one of the primary causes of unreliable fields, which accounted for 70% of unreliable tests in the OHTS.6 The Octopus perimeter continually monitors the patient’s pupil position and head position and does not present a test stimulus if the pupil is not centered or the forehead is not in contact with the headrest. This virtually eliminates fixation losses, thereby reducing the number of unreliable fields and the need for repeated testing.
The combination of the TOP strategy and fixation control features have made the Octopus an increasingly popular choice in busy practices looking to maximize efficiency in perimetry.
INNOVATIONS ARE CLEARING HURDLES
SITA faster
Zeiss recently released a new testing strategy called SITA-Faster. Available as an upgrade on the HFA3, SITA Faster incorporates several modifications to the SITA-Fast strategy that ultimately reduce the number of stimuli per test. Some of the notable changes include the removal of fixation loss and false-negative catch trials, no longer re-testing spots that were not able to see the maximum intensity lights and removal of the delay following unseen stimuli.
The culmination of these modifications is a 30% reduction in test time, allowing each eye to be done in 2 to 3 minutes while maintaining accuracy and repeatability.7
Portable perimetry
The bowl perimeters, like the devices discussed above, will likely continue to be the gold standard for many years to come. However, due to limitations in office resources (time, space and staff) and patient factors (availability, attention and fatigue), we are unable to perform visual fields frequently. Fortunately, novel technologies have recently emerged that promise to take perimetry outside of the office and into homes.
Perimetry has been adapted onto digital screens, improving accessibility and potentially allowing patients to get their visual fields from the convenience of their home.
Tablet/computer-based perimeters
The Melbourne Rapid Fields (MRF, M&S Technologies; Figure 2), developed with George Kong, MBBS, BMedSci, PhD, FRANZCO, is one of the more notable tablet-based perimeters. It allows for testing of the central 30° by moving the fixation point to the four corners of the screen. Studies have shown MRF to have a strong correlation with HFA, strong repeatability and similar test speeds compared to SITA-FAST.8 Similar to standard perimetry, MRF records fixation losses, false negatives and positives. Test results are saved to an online database and progression analysis can be performed after at least three tests are completed.

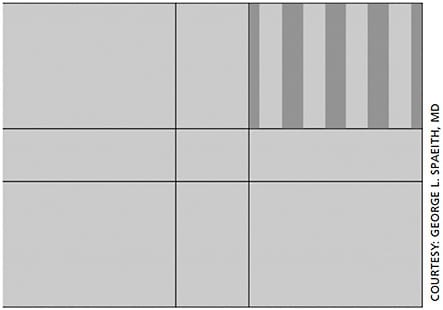
The Spaeth/Richman Contrast Sensitivity (SPARCS, www.sparcscontrastcenter.com ; Figure 3) test is an Internet-based test that measures the contrast thresholds in a patient’s central and peripheral vision. SPARCS has been tested and validated for multiple ocular diseases including glaucoma, cataracts and macular degeneration. When sitting 50 cm away from a 26.5-cm x 22-cm screen, the test occupies 30 x 23.5° of vision. Contrast thresholds are measured in five testing areas (central, superotemporal, superonasal, inferotemporal and inferonasal) using a bracketing technique. Vertical gratings from 100% to 0.45% are presented in each testing area, and a score from 0 to 20 is given for each region. The patient’s de-identified results are stored online for review.
The distinct drawbacks of these unsupervised tests are the challenges in creating the ideal testing environment and in controlling variables such as ambient lighting, viewing distance and distractions. However, the improved accessibility and convenience of in-home testing allows for a high frequency of testing, which can ultimately overcome home-associated variability.
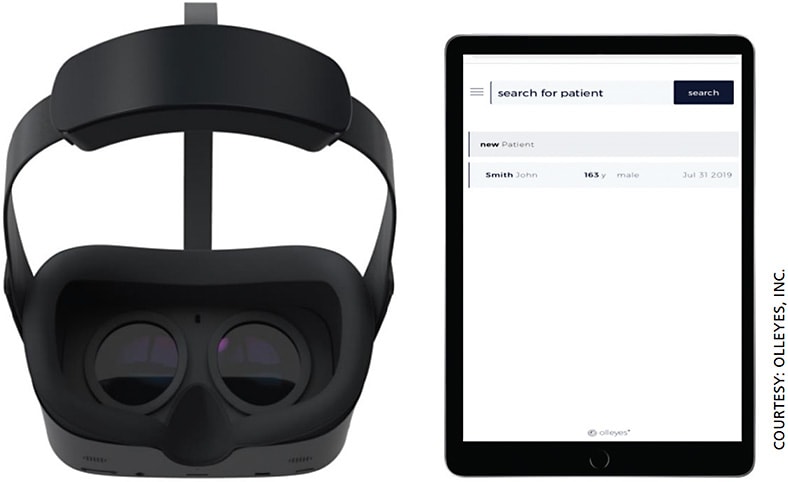
Head-mounted perimeters
Several virtual reality perimeters are on the market, with many more in production. These head-mounted devices solve many of the issues associated with perimetry. For instance, patients may be tested in any position, thus allowing patients with physical incompatibilities with standard bowl perimetry to get visual fields. Gaze-tracking technology is available in some devices (Figure 4), which enables an adjustable fixation point, reducing fixation losses. Additionally, the device’s full coverage of the eyes provides a more immersive experience and allows testing to occur in any lighting condition. Studies have found virtual reality glasses to have a strong correlation with the Humphrey perimeter.9,10
CONCLUSION
Glaucoma specialists are faced with a growing problem: The incidence of glaucoma has grown at nearly an exponential rate and is projected to continue in this trajectory. While new guidelines recommend an increased frequency of visual fields, the COVID-19 pandemic is driving the issue of efficient patient flow to the forefront as doctors strive to minimize crowding in waiting areas and maintain social distancing.
Though automated perimetry has been a major bottleneck in the past, recent updates to testing strategies and algorithms have significantly improved efficiency — now, a test that used to take 15 minutes per eye is down to 2 minutes each. Portable perimetry is a new and exciting field that may liberate visual field testing from the office. The improved accessibility will revolutionize glaucoma screening, and the ability to perform more frequent testing will improve our quality of care by detecting progression earlier. OM
REFERENCES
- Tham YC, Li X, Wong TY, et al. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. 2014;121:2081-2090.
- Sharma AK, Goldberg I, Graham SL, Mohsin M. Comparison of the Humphrey swedish interactive thresholding algorithm (SITA) and full threshold strategies. J Glaucoma. 2000;9:20-27.
- Chauhan BC, Garway-Heath DF, Goni FJ, et al. Practical recommendations for measuring rates of visual field change in glaucoma. Br J Ophthalmol. 2008;92:569-573.
- Malik R, Baker H, Russell RA, Crabb DP. A survey of attitudes of glaucoma subspecialists in England and Wales to visual field test intervals in relation to NICE guidelines. BMJ Open. 2013;3: e002067.
- Morales J, Weitzman ML, Gonzalez de la Rosa M. Comparison between Tendency-Oriented Perimetry (TOP) and octopus threshold perimetry. Ophthalmology. 2000;107:134-142.
- Johnson CA, Keltner JL, Cello KE, et al. Baseline visual field characteristics in the ocular hypertension treatment study. Ophthalmology. 2002;109:432-437.
- Heijl A, Patella VM, Chong LX, et al. A New SITA Perimetric Threshold Testing Algorithm: Construction and a Multicenter Clinical Study. Am J Ophthalmol. 2019;198:154-165.
- Prea SM, Kong YXG, Mehta A, et al. Six-month Longitudinal Comparison of a Portable Tablet Perimeter With the Humphrey Field Analyzer. Am J Ophthalmol. 2018;190:9-16.
- Tsapakis S, Papaconstantinou D, Diagourtas A, et al. Visual field examination method using virtual reality glasses compared with the Humphrey perimeter. Clin Ophthalmol. 2017;11:1431-1443.
- Razeghinejad MR, Gonzalez AM, Myers JS, Katz LJ. Virtual Reality Perimetry with Eye Tracking Compared with Standard Automated Perimetry. Poster presented at: American Glaucoma Society Annual Meeting, Feb 29, 2020, Washington, D.C.









