Treating astigmatism at the time of cataract surgery is one of the most rewarding things I do. The results are pleasing to the patient, to my staff and to me. But to achieve these results, there are rules to follow and technology to use, just as with everything else we do. I have been using toric IOLs to treat astigmatism for more than 10 years. I started with the STAAR Surgical toric IOL, then became the lead surgeon in the TECNIS Toric I (AMO) trial in 2010. Most recently, I was one of the surgeons in the offshore IOL study of what became the TECNIS Toric II (Johnson & Johnson Vision). In between, I have implanted every toric IOL available in the United States and some others currently available only in Central America. All worked, and worked well. Of course, there are differences in the various toric IOLs, and you should learn each toric IOLs strengths and use them to your advantage. The biggest influence on a toric IOL is you, the surgeon, and how you use your technology.
Using toric IOLs involves several possible pitfalls, and I will discuss all of the do’s and don’ts of astigmatism treatment with toric IOLs in this article. This includes a review of some of my errors from my professional journey treating astigmatism, along with a couple of critical issues that are rarely discussed with toric IOLs.
KNOW THE “ADD-ONS”
The autobody shop analogy
Imagine your car needs repairs (car surgery to your mechanic). You want the mechanic to use the best tools and do the best job possible for your car, because your car provides both transportation and protection for you and your family (similar to the eyes of your patients). Of course, you have options. Do you want to spend extra money to have the 50,000-mile tires with the special tread to help you avoid unexpected obstacles in the road?
Likewise, cataract surgery today comes with options. Our job as surgeons is to know the options and when and how to apply them.
Surgeons and their staffs understand the transactional nature of cataract surgery today. We offer a great basic service with monofocal IOLs with or without add-ons. We also offer some wonderful, optional add-ons to the surgery at the patients’ and the doctors’ discretion.
Toric IOLs: the ultimate add-on
Perhaps the most effective add-on is treating astigmatism with a toric IOL.
Toric IOLs are a very successful treatment for astigmatism. The mechanism for charging the patient for their astigmatism treatment is clearly defined, so rules to provide the service are clear. The market, however, tells us the story is more complicated.
As many as 70%-90% of all of our cataract patients could benefit from some level of astigmatism treatment. However, about 34% of patients have preop astigmatism between 0.5 D and 1.0 D.1 We do not have an approved IOL for treating that level of astigmatism, so the potential pool of eyes having cataract surgery with astigmatism treatable by toric IOLs is about 36% to 56% of all eyes. Yet approximately 7% to 9% of all eyes undergoing cataract surgery receive toric IOLs.2 What is the disconnect?
PERSPECTIVE IS IMPORTANT
What you can’t expect the patient to understand
When using toric IOLs, it is critical to look at the process from the patients’ perspective. The typical patient has no clue about sphere, cylinder and spherical aberration beyond the fact that they may or may not have “stigmatism,” as it is often called by our patients. If they do have “stigmatism,” they know it because their doctor has blamed their poor vision on it for decades. The typical patient knows astigmatism is not optimal. They want it gone, and they are often willing to pay for its elimination or, more realistically, significantly decreasing their astigmatism.
Do not get confused on this point. The patient does not understand astigmatism — they just know they have it. They want to see better and, from their perspective, treating astigmatism will make them see better. Additionally, the typical patient will pay extra to see better without glasses after cataract surgery.
So, will treating “stigmatism” improve their vision after cataract surgery? It depends on the details.
My cautionary tale
Here is my first and most important astigmatism doctor error story. It demonstrates a number of errors in one case. Some time ago, I saw a 40-something female patient present with bilateral cataracts, bilateral astigmatism and low amounts of myopia bilaterally. She needed cataract surgery and I discussed treating her astigmatism at the time of surgery with a toric IOL. She was all in. “Surgery went great in both eyes,” I told her afterward. I had eliminated her astigmatism with the toric IOL.
Not so fast. The patient was furious with me postop. She was so mad that she eventually asked the Attorney General of Indiana to investigate me and take away my license to practice medicine because of how I had treated her.
What happened? I had left her approximately +0.75 D sphere OU with an otherwise perfect surgical result. In my mind, I did her a service. Her astigmatism was eliminated, and I had reduced her sphere.
Before surgery, she had a bit of myopic astigmatism and early stage presbyopia in her early to mid 40s. In her mind, I made her vision worse with cataract surgery, after she paid me extra to do an especially good job for her. She used to be able to see a bit better at distance with her glasses and much better at near without her glasses. Postop, she could not see well at distance and her vision at near was much worse. She was furious. She did not care that I treated her astigmatism. She cared that she could not see the way she expected based on my preop discussion.
She was right. I had not done a good job in setting expectations and a worse job in her postop management. I had even argued with her about how well I fixed her astigmatism. What a mess.
Put yourself in the patient’s shoes
To avoid the above scenario, recognize that the patient has the most important perspective, and it is likely different from the surgeon’s perspective. The patient does not care that you eliminated their astigmatism unless you also fix their spherical error in a beneficial manner. Patients are unfamiliar with presbyopia.
If you leave a patient hyperopic and presbyopic when they were previously myopic astigmats, they will likely find the situation distressing.
Be prepared
Astigmatism treatment is refractive surgery during cataract surgery. The patient is paying for a spherocylinder refractive outcome — not just astigmatism treatment. They want and expect the whole package. Thus, the surgeon needs to have an enhancement strategy and a plan in place to treat postop surprises and disappointments. Your plan can be a variety of options, but should be in place prior to performing the surgery. Usually, the easiest and most cost-effective enhancement after a toric lens implant is LASIK or PRK. Yes, laser vision correction (LVC) after a toric IOL implantation is off-label, but it has been done very successfully for more than 20 years. The original surgeon does not need to perform the LVC enhancement but ideally has established a relationship with an appropriate surgeon who can provide the service.
The presurgical take-aways
From this case, we can state some clear rules to follow. Listen to the patient and try to understand their perspective. Remember that treating astigmatism with a toric IOL is a spherocylinder refractive treatment, not just a toric treatment. Have a written, signed refractive enhancement policy in place that is well defined for you, your staff and the patient. Ideally, that policy will include a refractive enhancement for the toric IOL patient as required at no cost to the patient. The cataract surgeon need not perform the refractive enhancement but should have some type of formal relationship with the refractive surgeon prior to the implantation of the toric IOL. This gives the surgeon, the staff and the patient confidence in the process.
NOW FOR THE SURGICAL PEARLS
Technique tips
Great surgical technique is always a plus. Understand that some extra rules are involved with toric IOLs. You want an anterior capsule that covers the anterior IOL edge for 360°. This discourages postop toric IOL rotation and encourages predictable effective lens position and a more predictable refractive spherical equivalent result. If you have difficulty achieving this manually, consider a femtosecond laser assist or a Zepto (Centricity Vision) assist for the capsulotomy.
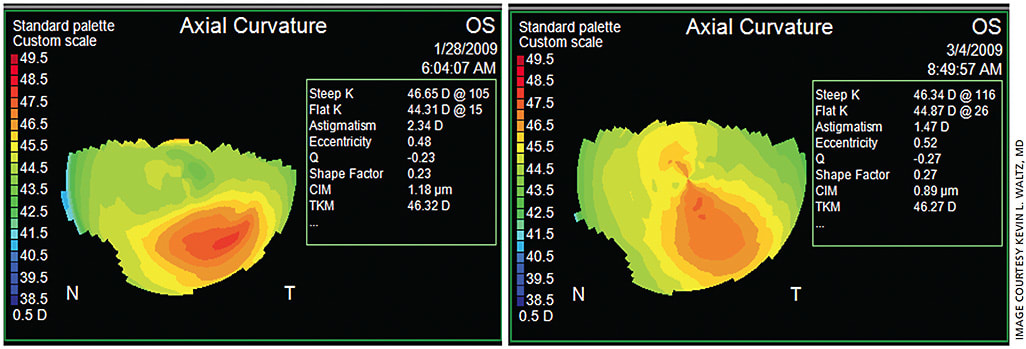
Work diligently to measure the preop corneal surface, including any necessary treatment to stabilize it prior to determining IOL power calculations. This includes topography on every eye being considered for a toric IOL. You are being paid for the extra outcome and the extra effort. In Indianapolis, I have found that I defer surgery to treat the ocular surface for as many as 20% of the patients referred to me for routine cataract surgery, especially in the winter months when the cold, dry weather often results in drier ocular surfaces (Figure 1).
Tools of the toric trade
Once you have a stable astigmatic axis, you need to accurately mark that axis for toric IOL placement. It is more difficult than it seems at first, but technology can help. After you have administered any necessary treatment to the ocular surface, you may take your preop measurements. It is common to manually mark the desired axis, but this method is fraught with imprecision. The width of a manual mark is easily 5°, even when accurately placed on the correct axis.
A number of helpful technologies are available to assist with accurate toric IOL axis placement. Two that help determine the correct toric axis are the Alcon ORA system, an intraoperative wavefront system, and the LensAR IntelliAxis laser system. The LensAR uses preop and intraop iris registration to determine the correct axis and marks the corresponding axis on the capsule (Figures 2 and 3). Also, the Zeiss Callisto eye system uses preoperative measurements to provide a very accurate intraoperative guide.


Finishing touches
It is very important to remove the ophthalmic viscosurgical device from behind the toric IOL during surgery. This can be done by a variety of methods. It is also a very good idea to examine the eye for correct and stable IOL placement after you believe the surgery is over. Sometimes something as simple as hydrating the incision one more time will cause an IOL to propeller from the force of the irrigation. In addition, look at the toric axis placement one more time after you think the case is over, just to be sure it has not rotated at end of the case.
SUMMARY
Toric IOLs are underutilized in the United States, considering the number of patients with pre-existing corneal astigmatism. By following the rules I’ve described, you can help more patients achieve better vision and do it in a way that is comfortable for you, your staff and your patients. OM
REFERENCES
- Hill W. Distribution of corneal astigmatism: Normal adult population. https://www.doctor-hill.com/iol-main/astigmatism_chart.htm . Accessed Aug. 28, 2020.2.
- Beltz J. The premium IOL pipeline. Ophthamology Management. Feb. 2020:34-40. www.ophthalmologymanagement.com/issues/2020/february-2020/the-premium-iol-pipeline . Accessed Aug. 28, 2020.









