Most patients starting their search for refractive surgery initially consider LASIK, PRK, or SMILE. That said, corneal pathology, such as epithelial basement membrane dystrophy, Fuchs’ endothelial dystrophy, keratoconus, pterygiums, RK scars and Salzmann’s nodules, can eliminate these patients as ideal candidates for some procedures. The good news: The implantation of lenses (or “lens refractive surgery”) is a group of procedures that patients who have concurrent corneal disease can often benefit from.
Phakic IOLs
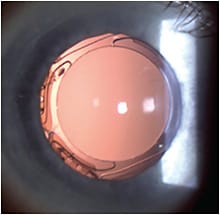
In my practice, we find that phakic IOLs, including the Visian Implantable Collamer Lens (ICL) (Staar Surgical) and the Visian Toric Implantable Collamer Lens (TICL) (Staar Surgical) are options to consider for young myopes who have corneal disease. Phakic IOLs bypass an otherwise compromised cornea in a way that does not cause the corneal disease to worsen.
Typically, we implant ICLs in myopic, or nearsighted, patients who are between 21 to 45 years of age and have more than -3.00 D, but less than -15.00 D of sphere, as ICLs are FDA approved for these refractive errors. We implant TICLs in patients who have myopic astigmatism and 1.0 D to 4.0 D of cylinder at the spectacle plane.
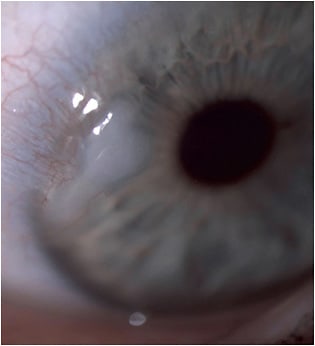
We have successfully treated patients who are highly myopic, have a large amount of astigmatism and keratoconus, or other causes of stromal thinning and protrusion, who need options other than glasses, contact lenses, or laser vision correction to help them see their best. Something else to consider: Due to reduced image minification, correction of refraction near the nodal point of the eye, it is not rare to observe patients gaining lines of best-corrected visual acuity (BCVA). In fact, in a subset of a report of our first-year experience using the TICL post-FDA approval, we looked at 31 eyes that were not correctable to 20/20 preoperatively, most due to corneal abnormalities, and found a statistically significant improvement in BCVA of one line of visual acuity on average.1 Furthermore, many of these eyes had postoperative Uncorrected VA that exceeded preoperative BCVA. Based on these results and other published reports of ICLs in the setting of corneal disease, we believe ICLs are safe and effective at correcting myopia with and without astigmatism when corneal disease, such as keratoconus and corneal scars, are present.
Oftentimes, we see patients seeking a second opinion because they’ve been told they aren’t candidates for LASIK, but still have the desire to reduce their need for contact lenses and glasses. The majority of the patients we see are thrilled when informed that lens refractive surgery may be suitable for them.
Cataracts, Corneal Disease, and Toric IOLs
It is common for us to use toric monofocal and toric trifocal IOLs, depending on a variety of clinical parameters and patient preferences. We believe our role is to inform the patient of every option possible to provide the best visual outcome, while taking into account whether corneal disease (or other ocular disease, for that matter) is present.
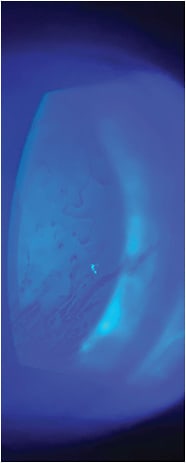
To ensure a satisfactory surgical outcome for these patients, we take multiple corneal topography images to check for abnormalities on the anterior surface of the eye. If there are abnormalities, such as Salzmann’s nodules or pterygia, we typically recommend removing those surface irregularities first; then bringing the patient back for a series of repeat scans and topographies before discussing with the patient which IOL we feel will best fit their needs.
In the case of Salzmann’s nodules or pterygia, we have experienced that corneal topography images before and after removal can decrease the amount of astigmatism drastically, affecting not only the power of toric IOL needed, but also the spherical power of the lens. Furthermore, some of these patients have a desire to have not only their distance vision corrected, but also their near. However, not all patients adapt well to monovision; and we typically do not recommend multifocal or trifocal IOLs to patients if they have significant corneal disease.
We’ve implanted the Crystalens AO (Bausch + Lomb) IOL and the Trulign Toric IOL (Bausch + Lomb), which provide excellent optics, particularly for distance and intermediate vision, but may still require reading glasses. (See “On the Horizon”.)
ON THE HORIZON
For patients who have concomitant corneal disease, an inability to adapt to monovision, and a strong desire to have spectacle independence, including for reading, we are working on an additional lens option.
Specifically, we have been investigators for an accommodating lens called the SC-9 IOL. This IOL is comprised of a large diameter, a hinge design and mechanism of accommodation that may provide large amplitudes of accommodation.
Another IOL we have experience with, both after implanting the lens outside of the country, as well as being investigators with the technology as part of the FDA clinical trial, is the IC-8 lens (Acufocus). This lens increases the depth of field via a pinhole effect. The dark circular annulus is embedded in the IOL. Over the past year, we have implanted nearly 80 subjects with one of these new IOLs that may be on the horizon for patients and surgeons in the U.S. Although we are not permitted to disclose statistical analyses, we have generally found that patients have been happy with the range of vision that these new IOLs provide.
Match Making
Most patients entering our offices seek surgical solutions for not only pathology, like corneal disease and cataract, but also a wide range of refractive errors they may present with. As corneal physicians, we are fortunate to have the technologies and surgical techniques to match a wide variety of patient needs and desires. We believe it is our job to diagnose and treat pathology, and also to help meet the desires of our patients as they relate to dependence on external optical aids, such as contact lenses and glasses. Utilizing lens refractive surgery, we have many options to mask corneal abnormalities to help our patients and provide good, quality vision. CP
Reference
- Mueller BH, Parkhurst G, Saenz B. Toric implantable collamer lenses: Early United States experience. Paper presented at: ASCRS Virtual Annual Meeting: May 16-17, 2020.










