Cataract surgery is one of the most impactful surgeries performed in the world. As ophthalmologists, we are fortunate to have such a transformative procedure to offer our patients. With the continual advancement of technology and technique, our ability to provide consistently outstanding refractive outcomes to our cataract surgery patients has continued to improve. As a result, their expectations of near-perfection have continued to grow, along with our anxieties about results. A well-executed preoperative evaluation is critical in setting appropriate expectations, determining an appropriate treatment strategy and delivering the best care we can.
Here, we provide tips and pearls for each step of the preoperative process to help achieve excellent outcomes.
1. HISTORY
As we learned in medical school, the first step to a successful patient encounter is obtaining a targeted history. For cataract patients, this often starts with a questionnaire. The questionnaire may include questions about prior ocular history, current symptoms and visual goals related to cataract surgery (for a sample questionnaire, see the online version of this article). Many practices find it beneficial to ask all patients about history of previous refractive surgery (LASIK, PRK, RK, etc), contact lens use (soft vs. rigid gas permeable), previous monovision, trauma, prostate medication use (eg, tamsulosin) and their ability to lie flat.
All of these historical factors can help the surgeon know how best to counsel the patient and prepare for surgery. A patient’s current symptoms can help the surgeon to determine whether a patient is likely to benefit from cataract surgery or whether waiting may be the best option. A patient’s responses about their visual goals can reveal what type of IOL may be the best choice for a patient as well as whether their expectations are reasonable.
2. EXAM
After obtaining and reviewing an appropriate history, a detailed examination of the eyes should be performed. Below is a list of important things to look for during each part of the exam that can help direct your preoperative and intraoperative approach:
- Eyelids. Meibomian gland disease and/or blepharitis
- Conjunctiva and sclera. Ptergyium (that could affect keratometry), evidence of prior filtering procedures in glaucoma patients
- Cornea. Fluorescein stain for evidence of ocular surface disease (OSD), tear film quality, presence of a LASIK flap or RK incisions, corneal scarring/nodules, anterior basement membrane dystrophy, endothelial guttae
- Anterior chamber. Depth, cell
- Anterior chamber angle (via gonioscopy). In all cases when considering minimally invasive glaucoma surgery
- Iris. Degree of dilation, evidence of prior ocular inflammation (posterior synechiae)
- Lens. Type and degree of cataract formation, evidence of pseudoexfoliation, phacodonesis in cases of prior trauma or pseudoexfoliation
- Posterior segment. Optic nerve cupping or pallor, macular disease (AMD, epiretinal membrane [ERM], macular hole, etc), retinal tears
Careful attention to the health of the ocular surface is especially important in evaluating the accuracy of biometry and the predictability of a desired refractive outcome. Many surgeons use fluorescein during every preoperative exam, which better elucidates the nature and extent of OSD. It is important to not flood the ocular surface with fluorescein, which masks surface epithelial irregularities. Instead, using a tiny dab of fluorescein from a strip is preferred because it highlights clinically significant disease. Delaying a surgery for several weeks or even months to treat the ocular surface can be disappointing to some patients, but this is often a crucial factor to refractive success, especially if a patient will receive a premium IOL (eg, toric, multifocal, extended depth of focus). OSD can (and typically does) worsen in the postoperative period; therefore, addressing the issue preoperatively can lead to improved patient satisfaction and compliance after surgery.
For patients already pseudophakic in the fellow eye, ask whether they have a card indicating what type of lens was implanted. If they don’t have this information, a detailed examination of the IOL can often help you identify it (ie, one- or three-piece, clear vs. yellow color, presence of multifocal rings, presence of toric markers). An examination of the pseudophakic fellow eye may also provide clues about how challenging the upcoming surgery may be (eg, presence of iris defects, open posterior capsule, pseudophakodonesis). Additionally, the refractive outcome of the fellow eye helps to guide an appropriate target for the surgical eye.
3. TESTING
Quality and agreement of preoperative testing is extremely important in refractive accuracy in cataract surgery. Individualizing the surgical plan to your patient’s desires and expectations is also vitally important.
- Topography. Many surgeons obtain topography for every preoperative cataract surgery patient. At the least, topography should likely be performed for every patient with a visually significant amount of astigmatism, a history of refractive surgery or a desire for a premium IOL. An irregular topography should prompt further questions about the patient’s history, including refractive surgery, contact lens wear and dry eye symptoms. Determination of the permanence of the irregular astigmatism is very important with respect to IOL selection.
- Biometry. IOL biometers have become much more advanced in recent years, allowing surgeons to better rely on the biometers’ measurements. The latest biometers can obtain an accurate axial length of nearly all eyes except those with the densest of cataracts, thus reducing the need for manual A-scan measurements. Advancements in keratometry have improved outcomes, with current biometers offering anterior and posterior corneal curvature measurements. In addition to offering more accurate results, these machines also give us more information — sometimes more than we know what to do with. Some under-utilized but useful parameters include the light reflex analysis of the ocular surface and the rudimentary macular OCT shown by the IOLMaster 700 (Zeiss, Figure). Like topography, biometry can change dramatically once a dry ocular surface is treated appropriately.
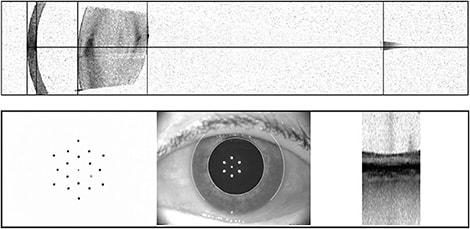
Figure. Patient images from the Zeiss IOLMaster 700. Bottom right: 1-mm macular OCT image. Bottom left: Keratometry image. Note irregularity of spots in this patient with ocular surface disease. These improved upon treatment, and the patient was retested prior to IOL type/power determination. - Astigmatism correction plan. Surgeons differ in their approach to selecting the appropriate type and degree of astigmatism correction for their patients. Three main parameters are usually compared: the topography, the biometer’s predicted K values and the manifest refraction. If these all agree on the amount and axis of astigmatism, the decision becomes simple. If they differ, the surgeon must decide which parameters to rely on or whether repeat measurements should be done. It is important to not rely too heavily on the manifest refraction because this includes lenticular astigmatism, which will be eliminated with cataract surgery. Critically evaluating postoperative residual astigmatism and comparing it with preoperative predictions can be a valuable exercise that allows the surgeon to tailor future treatment decisions.
- OCT macula. Like topography, some surgeons obtain OCT of the macula in every preoperative patient, even if the practice cannot charge for the procedure. For some surgeons, one bad experience relating to a missed ERM or other visually significant macular pathology is the deciding factor in implementing this practice. Despite our best efforts to closely examine the macula of every patient, there is always the possibility that we could miss visually significant macular disease. Properly identifying an ERM, macular edema or drusen can be critical for properly counseling patients about their visual potential and deciding what type of lens to implant. In our practice, we obtain an OCT of the macula in all patients who are interested in a presbyopia-correcting IOL or if there is a pathology that may affect the visual outcome. As previously mentioned, one of the latest biometers shows a small-width OCT of the macula, though the quality of this scan leaves something to be desired. Each practice may need to decide whether obtaining OCTs for every preoperative patient is worth the extra time and resources. Sharing the images of the OCT can be a valuable educational tool for patients with respect to explaining why a certain refractive technology may or may not be a good option.
4. COUNSELING AND INFORMED CONSENT
The informed consent process may be viewed as an opportunity to educate patients about the surgical procedure, lens implant options, risks, benefits and alternatives to surgery. In our practice, we routinely counsel patients that there is no perfect IOL and that we need to choose from what is available to best meet their personal vision goals. This discussion should be tailored to the patient’s comprehension level, and an authorized interpreter should always be used if any language barrier exists.
The consent process is our opportunity to discuss the known risks of surgery with patients while focusing on any complications they may be more predisposed to based on the evaluation. Common postoperative complaints associated with particular lenses should be addressed during the consent process to set appropriate expectations and avoid postoperative surprises. If patients understand that they will have some degree of glare and halos after placement of a multifocal lens, for example, they will likely be more tolerant of them early on. Also, ancillary procedures such as limbal relaxing incisions, laser vision correction or IOL exchange can be mentioned as viable options to help correct residual refractive error postoperatively. This is especially important to discuss with patients who are at higher risk for postoperative refractive surprises, such as patients with a history of refractive surgery.
While a well-rehearsed preoperative counseling discussion with patients is crucial, it is equally important to listen carefully to patients and to address any of their questions or concerns. Most patients have friends or family members who have undergone cataract surgery. As such, they may come to our offices with preconceived notions of cataract surgery based on what they have heard. Our duty as surgeons is to do our best to understand our patients’ expectations and concerns and to tailor our counseling and recommendations accordingly.
CONCLUSION
As cataract surgeons, we have the ability to make a dramatic improvement in our patients’ lives. With this ability comes our responsibility to provide our patients with the best possible experience and care. An integral part of every successful cataract surgery is a well-executed preoperative evaluation. As we utilize the incredible technology available to us, properly counsel our patients and consistently strive to improve, we will often witness great results and have the satisfaction of knowing we are making a positive impact in the world around us. OM










