“Would you want a finger stuck in your eye every day?”
Such was the response from a patient to Inder Paul Singh, MD, when he asked whether a Weiss ring floater was bothersome during a postcataract follow-up visit. For Dr. Singh, president and head of the glaucoma division of Eye Centers of Racine and Kenosha, Wis., this brought home how much floaters can impact a patient’s visual acuity and quality of life. It was, he says, a “poignant moment.”
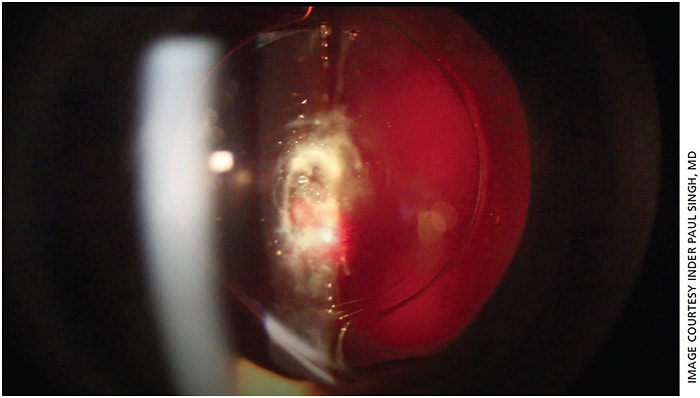
For patients who have had cataract surgery, visual opacities or floaters may be an unexpected outcome of their improved vision. With the cataract removed, your patient is likely seeing more clearly than he or she has in a long time. But with more light coming into the eye and greater contrast, your patient may now notice floaters that were masked by the cataract prior to surgery. Nearly 80% of patients without a posterior vitreous detachment going into cataract surgery develop one within 5 years after cataract surgery, according to the study “Posterior vitreous detachment and retinal detachment after cataract surgery,” by Ripandelli et al and published in Ophthalmology. And with today’s patient expectations for near-perfect vision, this can easily lead to dissatisfaction with the cataract surgery outcome — especially for patients who have paid for a premium IOL (Figure 1).
“From a patient’s perspective, it’s a real complication when floaters become symptomatic after surgery,” even though the doctor may not consider it significant, says John Hovanesian, MD, at Harvard Eye Associates in California and spokesperson for the AAO.
“What got me so passionate about this procedure was the ability to help the quality of life for patients who have floaters,” says Dr. Singh. “You realize that some of these patients are suffering and unable to perform many daily activities.”
In this article, we provide details on YAG vitreolysis technology for your cataract surgery patients. Let’s start with setting expectations.
EARLY WARNING
Prior to cataract surgery, you should set the correct expectations with patients about visual opacities. If you don’t alert the patient beforehand about the potential of a troublesome floater, “then it’s your problem postcataract surgery,” says Karl Stonecipher, MD, of Laser Defined Vision in Greensboro, N.C., and clinical associate professor of ophthalmology at the University of North Carolina.
Not all floaters are going to be so bothersome that they require intervention. For instance, your patient may neuroadapt.
“Many patients notice them, but the brain has an amazing ability to tolerate floaters,” says Dr. Hovanesian.
The floaters that mainly bother patients are those that are in line with the central visual axis, according to Dr. Stonecipher. Many times, you can see the floaters on the OCT exam.
Historically, patients with floaters were managed in one of two ways. The first was to tell them they simply had to live with the floaters. The second was to have them undergo a pars plana vitrectomy, with its attendant costs of several thousand dollars and risks of retinal tears and detachments, macular injury, and infection.
Now, a third option, in the form of specialized laser floater treatment, can help your patients with visual opacities.
STEPWISE APPROACH
To address a patient with a symptomatic floater, consider a stepwise approach, says Dr. Hovanesian. “I think it’s reasonable, based on current results, to offer a stepwise approach that would include laser floater treatment, and then failing that, or if that’s unavailable, to consider small-gauge vitrectomy.”
Laser floater treatment, or YAG vitreolysis, is meant for a specific population of patients with floaters and therefore is not necessarily a competitor to vitrectomy, notes Dr. Singh, who estimates he has performed some 5,000 laser floater treatments during the last 7 years. Instead of being a replacement to vitrectomy for floater treatment, YAG laser vitreolysis is another tool for ophthalmologists when treating patients with symptomatic and disabling floaters. When YAG vitreolysis is an option, physicians should refer to the classification chart developed by the International Ophthalmic Floater Society (IOFS), says Bill Swaim, president of Ellex, Inc. (To view the chart, which indicates when vitreolysis is appropriate for a patient, visit https://bit.ly/3dsjhEe .)
In laser floater treatment, visual opacities are vaporized with a YAG laser. The laser energy converts collagen and hyaluronic acid molecules inside the floater into a gas, notes Dr. Stonecipher. The gas is then resorbed into the eye.
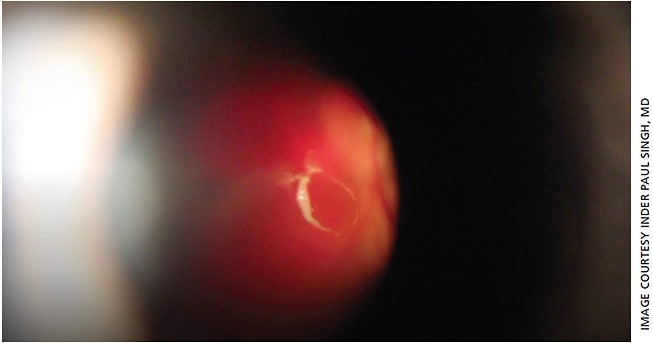
Not all postcataract surgery patients, of course, will benefit from this new technology. Good candidates for this laser floater treatment are patients who have a solitary opacity where it is easy to correlate signs and symptoms, says Dr. Singh, who adds that he only performs the procedure on patients who have symptoms affecting daily life. With a solitary Weiss ring floater, the opacity is easy to see and responds well to the laser, says Dr. Singh (Figure 2). A poor candidate, by comparison, is a patient whose floater is close to the retina or lens.
Although theoretically standard YAG lasers can visualize and treat opacities in the anterior vitreous, specific YAG laser technology, Ellex’s Reflex laser portfolio, is able to treat mid to posterior vitreous, where the majority of floaters are located, using enhanced visualization technology.
Besides the standard YAG laser indications for procedures such as “HD Cap” capsulotomy and iridectomy, the Ellex Reflex™ laser carries a 510(k) indication for “posterior membranectomy”, according to Mr. Swaim. This indication differentiates the Ellex Reflex laser portfolio from other YAG lasers and enables the treatment of membranes within most of the vitreous using certain precautions, according to Mr. Swaim. The two Reflex laser models are the Tango Reflex and the Ultra Q Reflex.
TRIO OF ABILITIES
One of the most important aspects of treating eye floaters in the vitreous involves improved visualization. Historically, YAG lasers, says Dr. Singh, have been designed to visualize the anterior segment and not behind the capsule. But the majority of floaters are located in the mid to posterior vitreous.
The Ellex laser has a specially designed coaxial illumination tower, along with a mirror that flips out of the way during laser delivery. This design means the surgeon does not have to be off-axis or oblique with illumination, as is likely with standard YAG lasers. “The visualization part of it was probably the most important differentiation between safety now and efficacy now versus previous YAG lasers,” says Dr. Singh.
This technology, he continues, provides spatial context, allowing the surgeon to identify the floater as well as the position of the floater in relation to the retina. This helps decrease the chance of hitting the retina with the laser during treatment. For instance, if the floater is in focus and the retina is obscured, the surgeon is far enough away from the retina to safely fire the laser.
Another advance in this technology is a truncated energy beam, meaning a sharper rise and fall of the energy delivery, says Dr. Singh, which is more efficient with “less scatter, less potential collateral damage.” To efficiently vaporize the vitreous opacity, the laser will often need to fire at 4 to 5 mJ, he notes, as opposed to the 1 or 2 mJ that are normally used for YAG capsulotomy. The laser can be fired up to 6 or 7 mJ per shot if the floater is of denser opacity or one that is more posterior in the vitreous cavity. Instead of breaking tissue, as in YAG capsulotomy, notes Dr. Singh, the goal is to vaporize the floater, necessitating higher energy settings on the laser.
But, this additional energy is not a cause for concern. There’s a non-linear relationship between how much energy is on the laser “and how much dispersion of energy in the eye, or what we call the shock wave or convergence zone,” Dr. Singh says. A shockwave for 1 mJ is about 110 µ; for 10 mJ, it is 210 µ. With this energy profile, as long as the retina is not in focus, there should be no worry about the shockwave hitting the retina, he says.
Finally, to ensure constant cooling, a system circulates air throughout the laser cavity. This provides a consistent level of laser energy and helps prevent interruptions in treatment from the laser pausing to cool, as would take place with standard YAG laser technology, says Mr. Swaim.
CONSIDERATIONS
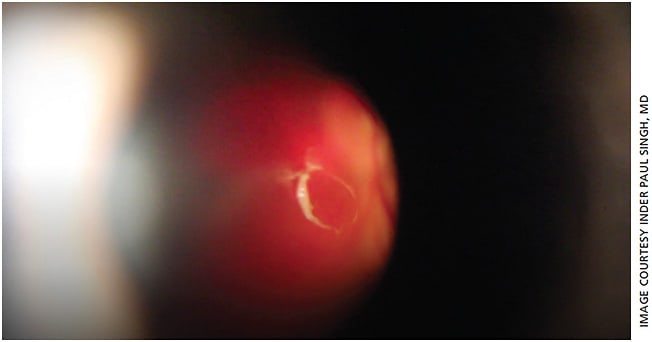
Vaporizing visual opacities may take more than one treatment. Dr. Stonecipher estimates that he needs 1.3 sessions, especially if he is vaporizing a large amorphous cloud-type floater (Figure 3). Dr. Singh presented the results of his study, “Treating Vitreous Floaters: Patient Satisfaction and Complications of Modern YAG Vitreolysis,” at the 2016 ASCRS meeting. His findings: an average of 1.2 sessions were needed to treat Weiss ring floaters. In other words, he notes, 20% of the time you may need a second session to remove small, leftover pieces of the floater. Also, for surgeons who are beginning to try laser floater treatment, Dr. Stonecipher recommends they walk before they run. “You want to do those easy cases that are easily visualized. You want to first do the easy cases like the Weiss ring in the mid vitreous.”
Dr. Singh recommends that surgeons who are just starting out limit the number of shots and have the patient return in a few weeks to monitor for pressure spikes. He limits the number of shots per session to around 350.
IMPROVING SATISFACTION
Although still relatively new, laser floater treatment merits consideration to help improve satisfaction for your postcataract surgery patients. After all, no one likes a finger in the eye. OM
Dr. Singh and Dr. Stonecipher disclosed financial relations with Ellex.








