The biggest fear of implementing EMR/EHR is that your eye examinations will be time-consuming to complete, resulting in longer days or seeing fewer patients per day and, inevitably, a reduction in income. Fortunately, your early-adopting peers have paved the way for those not yet on the paperless bandwagon.
CHOOSE THE RIGHT SYSTEM FOR YOUR NEEDS
In the early 2010s, Ben Lambright, MD, at West Coast Eye Institute in Lecanto, Fla., began researching and comparing EMRs. “Initially, there were 20 to 30 companies, but many were small. Some consolidated, while others simply disappeared,” Dr. Lambright says.
Of these initial options, Dr. Lambright looked for the system that best fit his needs. First, he navigated through various systems that were built for specialties other than ophthalmology and others that were not ideal for clinical practice or outpatient surgery. With ophthalmology-oriented EMRs, “some were better designed for retina specialists, such as MDIntelleSys (a Nextech company), while others were tuned towards comprehensive eye care or glaucoma.”
Dr. Lambright ultimately chose EyeMD Electronic Medical Records in August 2017, primarily due to the desire for a client/server-based solution, which was ideal for his rural practice where the internet is only marginally reliable. EyeMD EMR 2.0, which was released in fall 2019, offers fog computing, which has the benefits of both browser-based cloud and client/server-based systems, depending on a practice’s needs.
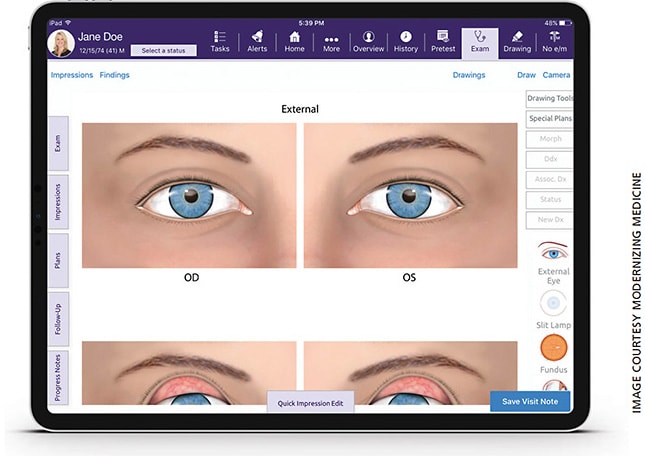
About 5 years ago, Colleen Joseph, MD, a general ophthalmologist at Metropolitan Ophthalmology Associates in Chevy Chase, Md., chose EMA by Modernizing Medicine (ModMed), which is app-based and can run on a PC or iPad, allowing Dr. Joseph to maintain eye contact during her patient encounters. She utilizes the integrated iPad to record her exams and utilizes features such as the microphone for dictating her findings as she peers through the slit lamp, turning Siri into her personal scribe. She also appreciates the ability to take photographs with her iPad, on which she can draw and label her findings.
Daniel Chang, MD, a cataract and refractive surgeon from Bakersfield, Calif., implemented ModMed’s EMA in October 2015. Recently, his clinic adopted the company’s latest offerings, which include ModMed’s Ambulatory Surgical Center (ASC) and Practice Management (PM) solutions, which are integrated to feed information back and forth to EMA and each other. This allows streamlining of his clinical, surgical and financial systems. For example, the patient’s operative report feeds directly from ASC to EMA, which is beneficial when it comes time for the patient’s 1-day postop visit.
Maya Shammas, MD, of Shammas Eye Medical Center, with locations in Los Angeles County, started using Compulink’s Advantage SMART Practice because she wanted an “all-in-one” system that could included practice management, medical records, optical and surgery center interfaces. “In our current climate under the COVID-19 pandemic, we as a field are faced with additional challenges,” she says. “Compulink’s EHR allows me to reach out to my patients using electronic communications and a built-in video chat for telemedicine.” To help with social distancing, she is also using the EHR’s web registration portal for check-in, to limit patient exposure with staff and other patients.

Thomas S. Shane, MD, of Retina Care Consultants, P.A., in Sarastoa, Fla., said his clinic made the switch to Nextech’s IntelleChartPRO after recommendations from colleagues. At first, Dr. Shane avoided EMR “for the longest time, believing it would harm our efficiency.” However, since the transition he’s realized it has made his staff more efficient. “Our imaging, notes and clinic flow are all in one central location that is accessible anywhere, which speeds our flow through the clinic and allows maximum doctor efficiency,” he says.
TRAINING AND CUSTOMIZATION
Thorough training in all aspects of the EMR is essential prior to launch.
“After purchasing the software and installing all hardware, we trained for approximately 3 months by rotating staff members through the training,” says Dr. Lambright. “Moving slowly and deliberately made us successful.”
Dr. Chang, along with his clinic manager, their colleagues and staff, also trained extensively prior to launch, particularly the front office staff members. “It is important that you have enough time to become as comfortable with the system as possible, but you don’t want to train too early, for example, more than 3 months ahead, because you can forget what you learned,” Dr. Chang advises.
Many systems offer a “sandbox” in which to explore and practice before going live. It is basically a trial version of the program that can be used with fake patients or with real patients and then paper copies can be printed and put in their charts. The sandbox is emptied when the system launches, so these exams are not saved.
When preparing to launch, you must be organized, Dr. Chang says. “If you aren’t fully committed, you’ll end up with some paper records and some digital records, which can turn into a bigger problem. The more integrated at the start, ultimately, the less work.”
West Coast Eye Institute’s assistant office manager and technician supervisor were responsible for customizing the EMR prior to launch. “We dedicated our assistant office manager to work full-time on the project to ensure its success,” says Dr. Lambright. “There should definitely be one expert in the office through whom all questions are funneled so the education and implementation are standardized.”
Finding the right person to lead the transition is crucial, says Dr. Chang. “They must be motivated and flexible. Reach to their strengths.”
Customization is another key to EHR success. For West Coast Eye Institute, this included the building of templates or prepopulated notes, called “fast plans” in EyeMD EMR. “Our scribes would gather approximately 10 charts for a specific type of case, a 1-day cataract postop for example, and then customize the fast plan based on the customary slit lamp findings, medications and follow-up instructions,” says Dr. Lambright. “These fast plans can be easily modified during actual patient exams. Most were created before we went live, but we continued to build them for the first year or so.”
Regional Eye Associates in Morgantown, W.Va., adopted Eye Care Leaders’ myCare Integrity in 2015. April O’Brien, special projects coordinator, helped prepare for the transition. “I began customizing the product and adding our keywords and workflow about a month ahead of launch,” she says.
Most companies offer onsite training as well. The physicians and technicians at Dr. Joseph’s practice chose remote training that their EHR company offered in 2-hour sessions, two to three times per week for 3 weeks.
IMPLEMENTATION
“Be deliberate about implementing,” says Dr. Lambright. Implementation is a balancing act of efficiency, productivity and personal comfort. At his practice, physicians staggered their implementation, such that only one MD applied the EMR at a time.
“I implemented first, increasing the number of patients on whom I used the EMR by 25% per week,” Dr. Lambright says. “The first week, 25% of my patients were seen using the EMR and 75% of charting was done on paper. The next week was 50/50, followed by 75/25. By the fourth week, I was using the EMR 100% of the time.” This approach saved him from reducing his patient volume.
Regional Eye Associates had a gradual implementation process for its six locations. “After go-live, we entered a couple of patients into myCare Integrity each day, but we ramped up much more quickly than we anticipated,” says Ms. O’Brien. “Three or four weeks after go-live, we were completely on myCare Integrity. Six weeks after launch, our first doctor was completely paperless. Six months after launch, over half of our doctors were completely paperless in most of our offices.”
When Dr. Joseph went live, she started at 50% EMR and 50% paper, building up slowly over a few months. “There was definitely an initial loss of efficiency but a gain in detail,” she says.
To help with EMR implementation, Dr. Joseph strongly suggests preloading patient charts into the EMR before their visit. For example, an 80-year-old patient’s 20 years of history at your practice can be very time-consuming to input on their exam day. Because of this, Dr. Joseph’s clinic hired a technician to enter returning patient data. As time went by and efficiency improved, this was done for patients a week before then a month in advance, until all the data were uploaded.
Dr. Chang found that rapid and accurate communication within the office was critical during and after implementation to ensure that system use was consistent.
WORKFLOW
Ideally, the workflow of your EMR should be the same as that of your practice, and if not be sure to adapt accordingly and quickly.
“The efficiencies we have appreciated are mostly in transitioning the patient from point to point within the office,” Dr. Lambright says. “For example, the patient’s information is sent directly to pretesting instead of the technician having to enter it manually. ICD-10 coding and Merit-based Incentive Payment System (MIPS) reporting are done at the point of care and transmitted into the practice management system. Communication with outside providers is sent immediately by fax.”
Many physicians find that, within the exam room, EMRs are very efficient for returning patients but can be bulky and cumbersome for new patients because of the quantity of data to be entered. This can be streamlined with third-party kiosks, where new patients use a tablet to enter their personal health history and medications prior to entering the exam room.
Dr. Lambright finishes about 95% of his charting during the exam. He may need to revisit ancillary tests, such as visual fields and OCTs, after the visit. Dr. Joseph finishes her charting on her iPad as she walks her patients out of the exam room.
Dr. Chang’s experience is slightly different. He continues to use scribes to do his charting, which allows him to have a face-to-face approach with his patients rather than burying his face in a tablet. If needed, he will review the file again later in the day on his EMR, which he says is “like seeing the patient twice.”
POWER OF POSITIVITY
Dr. Lambright’s final advice for implementing a new EMR: remain positive. “Emphasize to all staff, especially the physicians, to keep negative comments quiet. Pessimism is much more contagious than optimism. For a smooth transition, everyone needs to be on board.” OM








