Today’s retina practice continues to be challenged with increasing complexities due to the ongoing COVID-19 pandemic. Incorporating new technologies such as telemedicine, automated check-in/out, virtual waiting areas and updates to the EHR to the already complex clinical retina practice may seem intimidating. However, to provide outstanding patient care, it is important to have a relentless focus on quality and safety. The leading medical practices seamlessly adapt to the patients’ needs to deliver the best possible service.
The following article provides clinical care strategies to help optimize your practice during — and after — the COVID-19 pandemic.
CLINICAL VOLUME
An overall decrease in clinical volume has characterized the pandemic. Many vitreoretinal practices have experienced a volume reduction of more than 75%. However, most retina services are essential, and our practices need to adapt and ramp up to the pre-COVID-19 clinic volumes.
Understanding the individual characteristics of your practice will maximize the efforts to adapt to this new reality. Established practices may acclimatize differently than new ones. Surgically driven physicians may also employ different strategies to evaluate patients safely and in a timely fashion compared to medical retina practices.
Similar to pre-COVID-19, one of the most critical aspects that define resource use of any practice is clinical volume. Small (25 patients/day), medium (50 patients/day) and large (75 patients/day) volume practices have different staffing, imaging and clinical support requirements. It is important to continually reassess clinical volume (new evaluations vs. follow-up vs. procedures) and resource allocation as clinic volumes increase to pre-COVID-19 times.
VIRTUAL CHECK-IN & CHECK-OUT
Traditionally, many practices experience a significant bottleneck at the front desk. In small practices this may be due to limited staff, insurance verification, data entry and preauthorization. Larger practices may also experience front desk holdup due to patients arriving at unscheduled times and/or rapid turnover of follow-up patients. During the COVID-19 pandemic, optimization of check-in and check-out may be performed either online or by phone. Small practices may prefer having patients call the reception to check-in as soon as they are in the parking lot or outside the office. Medium or larger practices may consider an online automated receptionist. Once the patient’s physical presence is required, communication can be performed via the designated platform to have them then walk into the clinic.
Check-out may also be adapted to minimize physical proximity with the front desk staff. In general, cash payments should be avoided during the COVID-19 pandemic. Copays and deductibles can be performed electronically without the patient being physically at the front desk. Follow-up times may also be communicated by phone, email or online application.
VIRTUAL WAITING ROOMS
A packed waiting room may be terrifying for patients with multiple comorbidities. The classic waiting room setup with rows of chairs stacked next to each other may not be practical during these times. Signage to limit certain chairs in the waiting room can help employ social distancing inside the office.
However, the most powerful tool to minimize the time patient’s wait and potential exposure to infection inside medical offices is to have a virtual waiting room. Having patients wait in their car may be the best strategy to decompress the office space. A critical component of an efficient virtual waiting room is to know how much time it takes for patients to get into your physical office once the staff contacts them. The existing waiting room in your practice may be repurposed using social distancing for patients that are awaiting dilation, have particular mobility problems or are next in line for physical evaluation.
Training the staff to properly manage the virtual waiting room may take some time. However, once in place, this process may allow some practices to grow beyond their pre-COVID-19 volumes. Large-volume practices may consider investing in a coordinator who focuses on keeping the virtual waiting room in synchrony.
MEDICAL RECORD
Several ophthalmology focused EMRs are available and may help optimize your practice during the pandemic. The most advanced EMRs provide up-to-date government and insurance compliance with seamless optimization of billing.
Recent updates in many EMRs have integrated new features, including specific screening questions regarding COVID-19. New and follow-up patients should undergo telephone triage to ensure that the face-to-face evaluation is appropriate, to ensure that the patient is not at high-risk of COVID-19 infection or has had contact with any known or suspected COVID-19 patient. Specific questions regarding fever, shortness of breath, cough and malaise during the last 14 days should be performed.
Prepopulating of the EHR prior to physical check-in may also help minimize encounter time and exposure risk. This may be particularly important to new patients. Having the staff inquire and electronically upload any neuro-imaging, biopsy results, electroretinograms, genetic results and previous medical records may also help eliminate handoffs at the front desk.
Although multiple excellent EMRs are on the market, a common pitfall is to assume that because the practice EMR is compliant with government and insurance standards, the EMR provides excellent quality to your patients. Patients and referring physicians value when you display and provide an exceptional personalized service. To that end, try to tailor the EMR to each patient to fill the needs of each individual as much as possible. At this time, specifics regarding missed or delayed therapies, medical appointment and diagnostic studies due to the COVID-19 pandemic should be documented.
MULTIMODAL IMAGING
In the clinic, we routinely use spectral-domain optical coherence tomography (SD-OCT). Some practices may consider limiting how many patients undergo SD-OCT testing at peak times during the pandemic; however, to individualize care, it is important to reassess patients with SD-OCT regularly. Consider tailoring your SD-OCT utilization depending on prevalence of COVID-19 in your community.
To decrease the total office physical encounter time, assess if an imaging bottleneck is present for the utilization of SD-OCT. This occurs if patients need to wait in the office for the SD-OCT platform to become available. Ideally, patient flow should be streamlined so that patients move from one station to the next without waiting.
If your practice is bottlenecking, consider hiring a dedicated ophthalmic photographer to speed the process and minimize clinic COVID-19 exposure. Large-volume practices will undoubtedly need two SD-OCT platforms and one or more dedicated photographers.
Practices that have not upgraded to OCT angiography (OCTA) should consider doing so. This could potentially decrease the time allotted to contrast-based angiography and in some situations may provide the dual benefits of standard macular SD-OCT and fluorescein angiography. However, considerations regarding computer hardware demands should also be undertaken since OCTA studies require exponentially more hard drive space and imaging processing to display the vascular reconstructions.
CLINIC SPACE
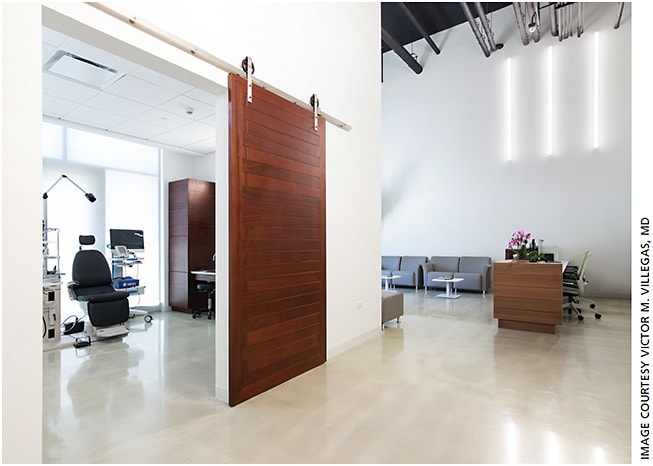
Another key aspect to consider is improved utilization of the current physical space. Small volume practices may benefit the most from multifunctional rooms because they also typically have less physical space (Figure). Cross-training staff to perform ophthalmic technician and photographer roles increases the staff medical care abilities and allows continuity of care for each patient. Accommodating an SD-OCT or ultra-widefield imaging platform into a cross-trained staff room may facilitate this task and may increase office efficiency by decreasing the time walking between rooms. This may also open existing imaging space for other uses, such as fundus photography or visual field platforms. Large practices may not benefit as much from multifunctional rooms; however, a clinic coordinator that aids in patient flow between technician rooms and imaging may be an enormous asset. This would ensure that patient flow is optimal and minimize wait times between different clinical and imaging stations. The clinic coordinator may also educate patients who are not wearing face masks appropriately as well as facilitate hand sanitizer use between encounters.
Ultimately, patients appreciate the efforts to decrease their risk of COVID-19 exposure. Optimizing clinic space to achieve this may provide an easy way to add value to your practice.
INTRAVITREAL INJECTIONS
Intravitreal injections may be performed in the physician evaluation room or may be performed in a separate room. Small-volume practices with limited space may benefit from performing intravitreal injections in the evaluation room. However, large-volume practices will decrease the bottleneck effects of intravitreal injections by using one or more rooms exclusively for intravitreal injections. Also, this allows for dedicated nurses who monitor and educate the patient before, during and after injections.
Select patients with stable visual acuity and no new complaints may undergo intravitreal therapy without extensive testing or dilation to improve efficiency and minimize exposure risk during the COVID-19 pandemic; however, the ability to individualize therapy and extend between treatment is reduced with this strategy. Therefore, the physician should weigh the risk of additional testing in the office against the potential to extend therapy. Switching patients to longer-acting intravitreal agents may provide additional safety. It is important to emphasize that patients undergoing treatment with brolucizumab should continue to be monitored for intraocular inflammation, including a thorough anterior and posterior segment examination immediately prior to each intravitreal injection.
SUBSPECIALTY CARE
Understanding the idiosyncrasy of your individual or group practice will enhance your ability to provide exceptional care. For example, ocular oncology practices have a high demand for ultrasonography. Although small-volume practices may use multifunctional rooms that allow the performance of ultrasonography, investing in an ocular ultrasonographer may increase the time dedicated to patients in face-to-face discussion.
Practices that focus on pediatric retinal disease will benefit the most from training the staff on pediatric ophthalmic examinations, especially in the evaluation of visual acuity. Special IOP and refraction instrumentation may also be needed, such as pediatric autorefractors and fixation devices. Practices with a uveitis subspecialist should evaluate the total time spent performing fluorescein and indocyanine green angiography. Investing in a second or third angiography platform may potentially increase the number of patients that can be seen in a given day.
SYNCHRONY and CLINIC FLOW
Perfect synchrony between patient and physician availability minimizes wasted time. However, several unaccountable factors can interfere with ideal flow, such as late or early patients, emergencies and equipment and staffing availability.
The best way to decrease inefficiency in the clinic is to allow for staff input. Due to the increasing number of details associated with operating a safe clinic during the COVID-19 pandemic, all the members of the clinical team should help identify the weaknesses associated with reaching synchrony, minimize COVID-19 exposure and help generate solutions. This form of team-oriented organizational assessment should be performed regularly. This may become particularly important as prevalence of COVID-19 evolves, staff availability changes or new technology is introduced into the practice.
PATIENT FOCUS
Focus the practice on the patient’s process during a visit. The ideal evaluation room allows the clinician to portray all data to the patient seamlessly. Having the patient easily understand the clinical scenario will provide vital reassurance of your expertise. Well-educated patients will unquestionably be invested in compliance and optimal clinical outcomes. Adding a scribe to the practice to free the physician from unnecessary time spent during the encounter may be the most valuable step toward increasing the time allotted to patient education.
After the organization identifies the areas it values, improvements should be made one at a time. This approach decreases the chances that the practice may run into an inadvertent bottleneck or new unsought problem. Changing many variables at the same time may make it difficult to assess the results. To gauge outcomes, it is important to monitor patient satisfaction directly with surveys or indirectly via web-based analyses to continue to shift the goals of the practice according to the patients’ needs.
CONCLUSION
During these unprecedented times, providing excellent care requires a patient-centered systematic approach that prioritizes safety and efficiency. Understanding the details in your practice and anticipating the problems as the practice evolves, especially as the COVID-19 pandemic begins to resolve, is an ongoing but important challenge in maintaining outstanding care. The best medical practices constantly reassess the changing inefficiencies and address them in a team-oriented approach without losing track of their passion for medicine and patient care. OM
About the Authors










