The maturation of FLACS
By Yuri McKee, MD
Until recently, the argument of femtosecond laser-assisted cataract surgery (FLACS) vs. manual cataract surgery had ultimately come down to surgeon preference. Study results were often equivocal between the two methods.
But recent studies now show that FLACS is capable of assisting or completely replacing several crucial aspects of the cataract surgical procedure.1-4
CREATION OF CAPSULOTOMY AND EFFECTIVE LENS POSITION
Capsulorhexis created with the femtosecond laser have been found to be more accurate and reproducible in terms of intended diameter, circularity and centration, ensuring better IOL overlap and minimizing the chances of IOL tilt and decentration vs. manual continuous-tear curvilinear capsulorhexis.5-10
Clinical evidence points to a more consistent capsulorhexis yielding a postoperative IOL position that is more predictive.10,11 Effective lens position (ELP) plays a key role in IOL power formula accuracy as even a 1-mm difference in IOL position results in around 1.25 D change in refractive error.12 As a natural consequence, IOL power calculations may become more predictive, lowering mean absolute error. Conrad-Hengerer et al13 showed a greater percentage of patients achieving postoperative refraction within ±0.5 D of the target at 6 months postoperatively (91% for FLACS vs. 71% for manual). With symmetric capsulotomy and more accurate ELP estimation, FLACS may provide more predictable refractive outcomes.
ENDOTHELIAL CELL LOSS
Corneal decompensation after phacoemulsification surgery is well documented and results in considerable increase in corneal thickness, thereby affecting the postoperative visual rehabilitation.14,15 Longer phacoemulsification time and the higher amount of phacoemulsification energy used are associated with higher endothelial cell loss.16,17
During FLACS, a cataractous lens is pre-treated and softened to shorten the phacoemulsification time and energy.18 This appears to provide the benefit of lesser endothelial cell loss, resulting in less corneal edema and early visual recovery.19-21 Therefore, FLACS can reduce the postoperative endothelial cell loss, which is specifically useful in high-risk groups such as eyes with small anterior chamber depth (shorter eyes), traumatic eyes, mature and dense cataracts, pseudoexfoliation or pre-existing endothelial dysfunction.22
FLACS FOR ZONULOPATHY
Cataract surgery steps like capsulorhexis and phacoemulsification are challenging in eyes with weak zonules. FLACS allows customization of capsulotomy size and location, providing a perfectly sized and shaped capsulotomy. In addition, FLACS decreases the maneuvers required for lens fragmentation by softening the lens with pretreatment. Thus, FLACS allows lesser intraocular manipulations for both capsulotomy and lens fragmentation, thereby decreasing the use of forceps and choppers intraoperatively and leading to reduced stress on already weak zonules.23,24 Better IOL centration in eyes with weak zonules is likely to improve visual outcomes. For example, two case reports documented corrected distance visual acuity of 20/25 or better.24
IOL PLACEMENT
With the introduction of iris registration-guided marking of the anterior capsule, a clear benefit has been defined that delineates FLACS as superior in cases of toric IOL placement.1,2,25,26
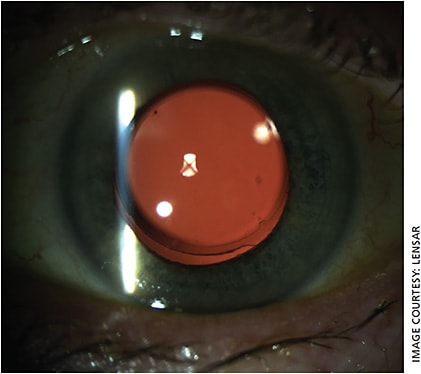
For example, the IntelliAxis (LENSAR) refractive capsulorhexis feature uses iris registration to create femtosecond laser-assisted capsular marks on the capsulorrhexis for guiding toric IOL alignment at the intended axis (Figure 1). The creation of capsular marks perfectly aligned with the steep meridian of the cornea creates a semi-permanent mark of the intended axis of IOL placement. Furthermore, these marks eliminate parallax error when aligning the IOL, which is invariably present with corneal ink marks. This feature makes it easy to recognize postoperative IOL rotation and measure it accurately.
ASTIGMATIC CORRECTION
At the ASCRS 2019 Annual Meeting, Visco1 reported her IntelliAxis outcomes: pre-existing astigmatism reduced from 2.18 ± 0.65 D preoperatively to 0.16 ± 0.19 D postoperatively (P <0.001). She found that 56% of eyes had no residual astigmatism and 100% achieved ≤0.5 D. Also, 85% of eyes had postoperative UDVA of 20/25 or better. Similarly, I reported significant reduction in astigmatism (from 2.2 ± 1.6 to 0.42 ± 0.33 D), with nearly 80% eyes achieving residual refractive astigmatism of ≤ 0.5 D.25 While better UDVA outcomes are expected, Kranitz et al7 reported significantly better corrected distance visual acuity (BCDVA) 1-year following FLACS (P= 0.038) due to lower induction of higher-order aberrations, significantly higher Strehl ratios and modulation transfer function values in the laser group compared to the manual group.27
FLACS-assisted astigmatism correction by arcuate incision construction is a safe and effective treatment option. At the ASCRS 2019 Annual Meeting, I reported significant reduction in astigmatism (from 0.96 D to 0.33 D) following femtosecond laser-assisted arcuate incisions during cataract surgery with more than 96% of the eyes achieving residual refractive astigmatism of ≤0.5 D.25
LENS FRAGMENTATION
Femtosecond laser-assisted pre-fragmentation of the crystalline lens lowers the effective phacoemulsification time and energy,8,28,29 translating into less corneal endothelium damage,4,5,18,20 corneal edema/central corneal thickness4 and aqueous flare.18,30,31 The overall complication rate with FLACS (1.8%)is also reported to be lower than manual cataract surgery (MCS) (5.8%).32
AUTOMATION
FLACS offers other less quantifiable advantages, including the automation of difficult portions of complex cataract surgery. Examples include automated creation of a circular and centered capsulorhexis in the absence of normal zonules and softening of very dense cataracts to reduce phaco energy. The reduction of risk in complex cataract surgery by automation of critical steps is seen as a significant advance by many surgeons.
COUNTERING THE COUNTERS
The primary arguments made by opponents of FLACS tend to revolve around the increased time and money required for the procedure. I have found that FLACS is actually a time and money saver in many cases.
Take, for example, the placement of a toric IOL. Prior to FLACS, I had to mark the patient’s cornea in an upright position prior to any sedation being given. The marking device required sterilization between each patient. The logistical effort to coordinate multiple toric IOL placements in one day was sometimes monumental. With iris registration and capsular marking done by the femtosecond laser, I now need no additional consideration for the surgical flow of a patient receiving a toric IOL. No pre-operative marking, no changing the flow for the anesthesiologist or fading or smearing corneal ink marks are involved.
Furthermore, when aligning the toric IOL, there is no guess work or attempting to “split the difference” due to parallax error. The IOL is either perfectly lined up with the capsule alignment tags or it obviously isn’t.
Additional time-saving steps include the automated capsulotomy and the pre-fragmentation of the lens. In my experience, the femtosecond laser typically requires less than 2 minutes of total applied patient interface time — and the automated capsulotomy, perfect toric IOL alignment and pre-fragmented cataract save additional time.
In terms of cost, the opponents of FLACS often quote a mythical “half-million dollars.” Sadly, this is a misinformed fallacy. There are numerous opportunities from purchase to lease FLACS technology that require little or no money up-front.
In our practice, we do not charge extra for FLACS. We include this technology with all premium cataract packages. The advanced technology included in all premium cataract packages is recognized as valuable by patients and increases our premium conversion rate.
CONCLUSION
The maturation of FLACS has brought consistency, safety and innovation to premium cataract surgery. Iris registration for astigmatism correction, perfection of the capsulorhexis and significant reduction of phaco energy due to nucleus pre-fragmentation are all significant advantages that cannot be achieved by manual surgery.
Constant innovation and improvements to the technology promise even more refined technique and improved patient results.
REFERENCES
- Visco DM, “Iris registration-guided femtosecond laser-assisted capsular marks to guide toric IOL alignment during cataract surgery,” presented at the ASCRS.ASOA annual meeting, San Diego, California, USA, May 2019.
- Jackson MA, “Toric IOL alignment: Femtosecond laser-assisted capsular marks versus intrastromal corneal marks,” presented at the ASCRS.ASOA annual meeting, San Diego, California, USA, May 2019.
- Tran BD, “Arcuate incisions or Toric IOLs for correction of pre-existing corneal astigmatism: A comparative study,” presented at the ASCRS.ASOA annual meeting, San Diego, California, USA, May 2019.
- Popovic M, Campos-Moller X, Schlenker MB, Ahmed, II. Efficacy and Safety of Femtosecond Laser-Assisted Cataract Surgery Compared with Manual Cataract Surgery: A Meta-Analysis of 14 567 Eyes. Ophthalmology. 2016;123(10):2113-2126.
- Abell RG, Kerr NM, Vote BJ. Toward zero effective phacoemulsification time using femtosecond laser pretreatment. Ophthalmology. 2013;120(5):942-948.
- Daya SM, Nanavaty MA, Espinosa-Lagana MM. Translenticular hydrodissection, lens fragmentation, and influence on ultrasound power in femtosecond laser-assisted cataract surgery and refractive lens exchange. J Cataract Refract Surg. 2014;40(1):37-43.
- Kranitz K, Mihaltz K, Sandor GL, Takacs A, Knorz MC, Nagy ZZ. Intraocular lens tilt and decentration measured by Scheimpflug camera following manual or femtosecond laser-created continuous circular capsulotomy. J Refract Surg. 2012;28(4):259-263.
- Mayer WJ, Klaproth OK, Hengerer FH, Kohnen T. Impact of crystalline lens opacification on effective phacoemulsification time in femtosecond laser-assisted cataract surgery. Am J Ophthalmol. 2014;157(2):426-432 e421.
- Reddy KP, Kandulla J, Auffarth GU. Effectiveness and safety of femtosecond laser-assisted lens fragmentation and anterior capsulotomy versus the manual technique in cataract surgery. J Cataract Refract Surg. 2013;39(9):1297-1306.
- Toto L, Mastropasqua R, Mattei PA, et al. Postoperative IOL Axial Movements and Refractive Changes After Femtosecond Laser-assisted Cataract Surgery Versus Conventional Phacoemulsification. J Refract Surg. 2015;31(8):524-530.
- Mastropasqua L, Toto L, Mattei PA, et al. Optical coherence tomography and 3-dimensional confocal structured imaging system-guided femtosecond laser capsulotomy versus manual continuous curvilinear capsulorhexis. J Cataract Refract Surg. 2014;40(12):2035-2043.
- Krarup T, Holm LM, la Cour M, Kjaerbo H. Endothelial cell loss and refractive predictability in femtosecond laser-assisted cataract surgery compared with conventional cataract surgery. Acta Ophthalmol. 2014;92(7):617-622.
- Conrad-Hengerer I, Al Sheikh M, Hengerer FH, Schultz T, Dick HB. Comparison of visual recovery and refractive stability between femtosecond laser-assisted cataract surgery and standard phacoemulsification: six-month follow-up. J Cataract Refract Surg. 2015;41(7):1356-1364.
- Ganekal S, Nagarajappa A. Comparison of morphological and functional endothelial cell changes after cataract surgery: phacoemulsification versus manual small-incision cataract surgery. Middle East Afr J Ophthalmol. 2014;21(1):56-60.
- Hwang HB, Lyu B, Yim HB, Lee NY. Endothelial Cell Loss after Phacoemulsification according to Different Anterior Chamber Depths. J Ophthalmol. 2015;2015:210716.
- O’Brien PD, Fitzpatrick P, Kilmartin DJ, Beatty S. Risk factors for endothelial cell loss after phacoemulsification surgery by a junior resident. J Cataract Refract Surg. 2004;30(4):839-843.
- Krarup T, Ejstrup R, Mortensen A, la Cour M, Holm LM. Comparison of refractive predictability and endothelial cell loss in femtosecond laser-assisted cataract surgery and conventional phaco surgery: prospective randomised trial with 6 months of follow-up. BMJ Open Ophthalmol. 2019;4(1):e000233.
- Conrad-Hengerer I, Al Juburi M, Schultz T, Hengerer FH, Dick HB. Corneal endothelial cell loss and corneal thickness in conventional compared with femtosecond laser-assisted cataract surgery: three-month follow-up. J Cataract Refract Surg. 2013;39(9):1307-1313.
- Ye Z, Li Z, He S. A Meta-Analysis Comparing Postoperative Complications and Outcomes of Femtosecond Laser-Assisted Cataract Surgery versus Conventional Phacoemulsification for Cataract. J Ophthalmol. 2017;2017:3849152.
- Abell RG, Kerr NM, Howie AR, Mustaffa Kamal MA, Allen PL, Vote BJ. Effect of femtosecond laser-assisted cataract surgery on the corneal endothelium. J Cataract Refract Surg. 2014;40(11):1777-1783.
- Takacs AI, Kovacs I, Mihaltz K, Filkorn T, Knorz MC, Nagy ZZ. Central corneal volume and endothelial cell count following femtosecond laser-assisted refractive cataract surgery compared to conventional phacoemulsification. J Refract Surg. 2012;28(6):387-391.
- Walkow T, Anders N, Klebe S. Endothelial cell loss after phacoemulsification: relation to preoperative and intraoperative parameters. J Cataract Refract Surg. 2000;26(5):727-732.
- Teshigawara T, Meguro A, Sanjo S, Hata S, Mizuki N. The advantages of femtosecond laser-assisted cataract surgery for zonulopathy. Int Med Case Rep J. 2019;12:109-116.
- Dryjski O, Awidi A, Daoud YJ. Femtosecond laser-assisted cataract surgery in patients with zonular weakness. Am J Ophthalmol Case Rep. 2019;15:100483.
- McKee Y, “Barrett Integrated K method for toric IOL calculations and femtosecond laser-assisted capsular marks for toric IOL alignment,” presented at the ASCRS.ASOA annual meeting, San Diego, California, USA, May 2019.
- Weinstock JR, “Accuracy and stability of Iris registered femtosecond laser-assisted anterior capsule axis markings for toric IOL placement,” presented at the ASCRS.ASOA annual meeting, San Diego, California, USA, May 2019.
- Mihaltz K, Knorz MC, Alio JL, et al. Internal aberrations and optical quality after femtosecond laser anterior capsulotomy in cataract surgery. J Refract Surg. 2011;27(10):711-716.
- Abell RG, Kerr NM, Vote BJ. Femtosecond laser-assisted cataract surgery compared with conventional cataract surgery. Clin Exp Ophthalmol. 2013;41(5):455-462.
- Conrad-Hengerer I, Hengerer FH, Schultz T, Dick HB. Effect of femtosecond laser fragmentation on effective phacoemulsification time in cataract surgery. J Refract Surg. 2012;28(12):879-883.
- Abell RG, Allen PL, Vote BJ. Anterior chamber flare after femtosecond laser-assisted cataract surgery. J Cataract Refract Surg. 2013;39(9):1321-1326.
- Dick HB, Schultz T. A Review of Laser-Assisted Versus Traditional Phacoemulsification Cataract Surgery. Ophthalmol Ther. 2017;6(1):7-18.
- Chen X, Xiao W, Ye S, Chen W, Liu Y. Efficacy and safety of femtosecond laser-assisted cataract surgery versus conventional phacoemulsification for cataract: a meta-analysis of randomized controlled trials. Sci Rep. 2015;5:13123.
About the Author
Has this pivotal innovation arrived?
By Samantha L. Schockman, MD, and Michael E. Snyder, MD
Charles D. Kelman’s invention of phacoemulsification in 1967 and Sir Nicholas Harold Lloyd Ridley’s introduction of IOLs in the mid 1900s were pivotal innovations that catapulted cataract surgery into the modern era. It is instructive to remember that both innovations were widely scorned before they were lauded. We must remind ourselves to neither scorn nor laud prematurely, but instead to use the principles of evidence-based medicine to advance innovation toward improved patient outcomes, safety and cost in cataract surgery.
Femtosecond laser-assisted cataract surgery (FLACS) was first introduced in 2009 and seemed to promise the next evolution in our surgical field. Now, a decade later, we have the opportunity to review large data series and critically evaluate the FLACS technology regarding patient outcomes, safety and cost.
OUTCOMES DATA
When FLACS was introduced, many believed this new technological advancement would allow for more accurate and reproducible surgical incisions, capsulotomies and IOL centration, while decreasing complications. In essence, FLACS promised better outcomes and fewer complications.
By now, many large studies have analyzed FLACS outcomes. Berk et al. reviewed 883 eyes with MCS compared to 955 eyes with FLACS and found no statistically significant difference in refractive or visual outcomes.1 Manning et al found “Femtosecond laser-assisted cataract surgery did not yield better visual or refractive outcomes than conventional phacoemulsification cataract surgery.”2 Also, a meta analysis involving more than 14,000 eyes, 15 randomized controlled trials and 22 observational cohort studies confirmed that FLACS does not result in clinically meaningful improvements in visual or refractive outcomes compared to conventional MCS.3
SAFETY COMPARISON
When comparing the safety of FLACS vs. MCS, we find it advantageous to focus on separate steps of cataract surgery independently. A critical early step involves creating a clear corneal incision (CCI). Zhu et al found that CCIs created using FLACS cause more surgically induced astigmatism compared to manually created CCIs.6 In addition, their data showed that FLACS CCI is thinner and more anteriorly located when compared to manual CCIs, suggesting less structural integrity.6
CREATING THE CAPSULORHEXIS
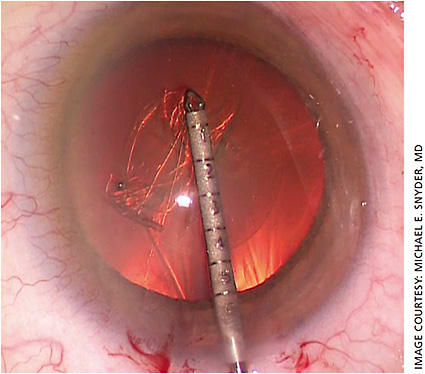
Currently, FLACS is most routinely used in creating the capsulorhexis, so it seems imperative to look at this step closely. Data in a study by Abell et al showed FLACS to have an increased rate of anterior capsule tears (1.87%) compared to MCS (0.12%),4 the result of compromised capsulotomy integrity and strength directly due to use of the laser. This was illustrated with scanning electron microscopy images that demonstrate irregularity at the capsule margin with multiple aberrantly misplaced laser pits in normal parts of the tissue in FLACS-created capsulotomies.4 Although pre-dating FLACS by nearly 20 years, Krag et al’s paper on the finite element method analysis of capsulotomy anticipated the weaker FLACS capsulotomy, demonstrating that a manual capsulorhexis’ strength results from its continuous edge, resulting in low and uniform stress distribution.5 The irregularity of a FLACS capsulorhexis edge cultivates an inherent weakness that results in increased anterior capsular tears and complications.
Some FLACS advocates may argue that the increased risks described above are outweighed in specific scenarios in which FLACS theoretically can be advantageous, such as in a Fuchs’ dystrophy patient. Some postulate that FLACS decreases phacoemulsification time, perhaps resulting in less corneal decompensation in Fuchs’ endothelial corneal dystrophy. But, data from Zhu et al showed that FLACS did not lower the rate of corneal decompensation in patients with Fuchs’ compared to MCS.8 In addition, the meta-analysis done by Popovic et al showed that FLACS was associated with higher rates of posterior capsular tears compared to MCS.3 Others have demonstrated the rate of unplanned vitrectomy between FLACS and MCS to be comparable.7 The current data regarding posterior capsule tears and unplanned vitrectomies in FLACS vs. MCS is equivocal.
COST AND TIME
Lubahn et al found FLACS cases take 11.6-13.4 minutes longer compared to MCS in both hospital and eye hospital-based settings,9,10 which would substantially limit the surgeon’s efficiency when multiple cases are scheduled per day. This is an important consideration in a medical landscape in which efficiency and smart cost-effectiveness are key to success. Investing in a FLACS system results in extra cost for the surgeon and for the patient to receive such services. Utilizing FLACS means spending more money and time. We also wonder how much of this information is or should be included in an informed consent process.
CONCLUSION
When investigating new technologies and devices to advance our surgical practices, it is imperative to query if it is beneficial for our patients: does it improve outcomes, safety or cost-burden ratio? According to the data above, FLACS has not fulfilled these requirements when compared to MCS.
As our predecessors once did, we should continue to investigate and grow our ideas and technologies to improve our surgeries and care for our patients. While FLACS may one day lead to a technology that fulfills our requirements to improve cataract surgery, after 10 years, that day has not yet arrived. OM
REFERENCES
- Berk TA, Schlenker MB, Campos-Möller X, Pereira AM, Ahmed IIK. Visual and Refractive Outcomes in Manual versus Femtosecond Laser-Assisted Cataract Surgery: A Single-Center Retrospective Cohort Analysis of 1838 Eyes. Ophthalmology. 2018;125:1172-1180.
- Manning S, Barry P, Henry Y, et al. Femtosecond laser-assisted cataract surgery versus standard phacoemulsification cataract surgery: Study from the European Registry of Quality Outcomes for Cataract and Refractive Surgery. J Cataract Refract Surg. 2016;42:1779-1790
- Popovic M, Campos-Möller X, Schlenker MB, Ahmed II. Efficacy and Safety of Femtosecond Laser-Assisted Cataract Surgery Compared with Manual Cataract Surgery: A Meta-Analysis of 14,567 Eyes. Ophthalmology. 2016;123:2113-2126.
- Abell RG, Vote BJ. Cost-effectiveness of femtosecond laser-assisted cataract surgery versus phacoemulsification cataract surgery. Ophthalmology. 2014;121:10-16.
- Krag S, Thim K, Corydon L, Kyster B. Biomechanical aspects of the anterior capsulotomy. J Cataract Refract Surg. 1994;20:410-416.
- Zhu S, Qu N, Wang W, et al. Morphologic features and surgically induced astigmatism of femtosecond laser versus manual clear corneal incisions. J Cataract Refract Surg. 2017;43:1430-1435.
- Song C, Baharozian CJ, Hatch KM, Grassett GC, Talamo JH. Rate of Unplanned Vitrectomies in Femtosecond Laser-Assisted Cataract Surgery Compared to Conventional Phacoemulsification. J Cataract Refract Surg. 2018;34:610-614.
- Zhu DC, Shah P, Feuer WJ, Shi W, Koo EH. Outcomes of conventional phacoemulsification versus femtosecond laser-assisted cataract surgery in eyes with Fuchs endothelial corneal dystrophy. J Cataract Refract Surg. 2018;44:534-540.
- Lubahn JG, Donaldson KE, Culbertson WW, Yoo SH. Operating times of experienced cataract surgeons beginning femtosecond laser-assisted cataract surgery. J Cataract Refract Surg. 2014;40:1773-1776.
- Day AC, Smith PR, Tang HL, et al. Surgical efficiency in femtosecond laser cataract surgery compared with phacoemulsification cataract surgery: a case controlled study. BMJ Open. 2018;8:e018478.











