For every patient who chooses a premium IOL option, surgeons experience a simultaneous sense of excitement and anxiety. Offering best-in-class treatment options is not enough. The patient expects to be given exactly the vision he/she asks for with the advanced and more expensive IOL selection, but can the surgeon really ever deliver on that expectation?
Below, I give my approach to reducing enhancement rates in premium IOL surgery and ultimately achieving the best possible outcomes. Just as importantly, these outcomes produce the happiest patients, delivering more word-of-mouth advertising and more referrals after their surgery. My approach is the same, covering the preoperative or postoperative stages of the premium process: setting patient expectations, presenting appropriate lifestyle options, diagnostic testing and — again — setting patient expectations throughout.
SETTING PATIENT EXPECTATIONS: IN THE BEGINNING
The phrase “under promise and over deliver” may seem a tired one to some, but as surgeons setting patient expectations throughout the entire surgical experience, it will never get old to me. From preoperative to intraoperative to postoperative, it is in my opinion the single most important part of reducing enhancement rates in premium IOL surgery.
At Jacksoneye, we begin addressing patient expectations before a patient even has a single diagnostic test or vision test. All of our cataract evaluation patients receive a modified Dell questionnaire, which is instrumental for how I decide what options to present to a patient before we even meet face to face (Figure 1).

This lifestyle questionnaire reveals factors about the patient that are critical to understand for the cataract surgery to be successful; for instance, the patient’s desire to wear glasses or not postoperatively, and his or her lifestyle activities, as no two patients are ever the same in occupation and hobbies. The questionnaire also forces a patient to self-grade his or her personality, from easy-going to perfectionist. One of my patients circled “perfectionist” with a pen so many times it tore the paper — as you might expect, I did not upgrade this patient to a premium IOL.
Intel from a preoperative questionnaire can be life-saving in the premium process. When checking a patient’s daily living activities on this form, I frequently see responses that they care only about driving day and night postoperatively. This type of patient is perfect for our driving vision option, “Legal to Drive (LTD)” (developed by James Loden, MD, in Nashville, Tenn.).
Lastly, if a patient indicates he or she has no issue with wearing glasses postoperatively, I typically will save chair time and offer our Basic LENSAR option — which is our femtosecond laser option that provides minimal astigmatic correction but offers no guarantee that they will be free of glasses postoperatively. Instead, this option specifies that the patient will still need glasses full time for all activities distance, intermediate and near, 100% of the time. These patients will just need a prescription for glasses postoperatively.
Another critical expectation to address: Most patients expect to be free of glasses postoperatively and come in believing that insurance and Medicare will pay for this. Educating the patient as to the reality of the situation and then providing the best customized options for each patient reduces and/or eliminates both chair time and enhancement postoperatively.
One last point on patient expectations: Intel received from a referring primary care physician or optometrist can also be invaluable, so always have them send a tracking form regarding the patient ahead of time. Many of our referring ODs know our lifestyle options already and will recommend to our surgeons the best option for that individual patient, assuming diagnostic testing allows. This further helps reduce chair time.
The referring ODs have treated many of our cataract patients for years and know their lifestyle needs better than we can in one surgical evaluation visit.
THE LIFESTYLE OPTION MENU
Exam lanes are much easier when you minimize ocular terminology verbiage with cataract patients. Tossing the jargon has resulted in higher conversions, reduced enhancement rates and fewer unhappy patients postoperatively.
First and most importantly, never give patients more than two options. Otherwise, you typically send them into a spiral of confusion to the point that they may not even proceed with cataract surgery. With all the intel described above and the appropriate diagnostic objective data (to be discussed below), our doctors enter an exam lane with one or two options to present to a patient. Patients never have to choose on the day of their cataract evaluation; instead, they receive an informational packet on the option proposed, including associated costs and financing options. They can take this packet home and share with significant others/family/friends before returning to their scheduling visit with our surgery coordinator.
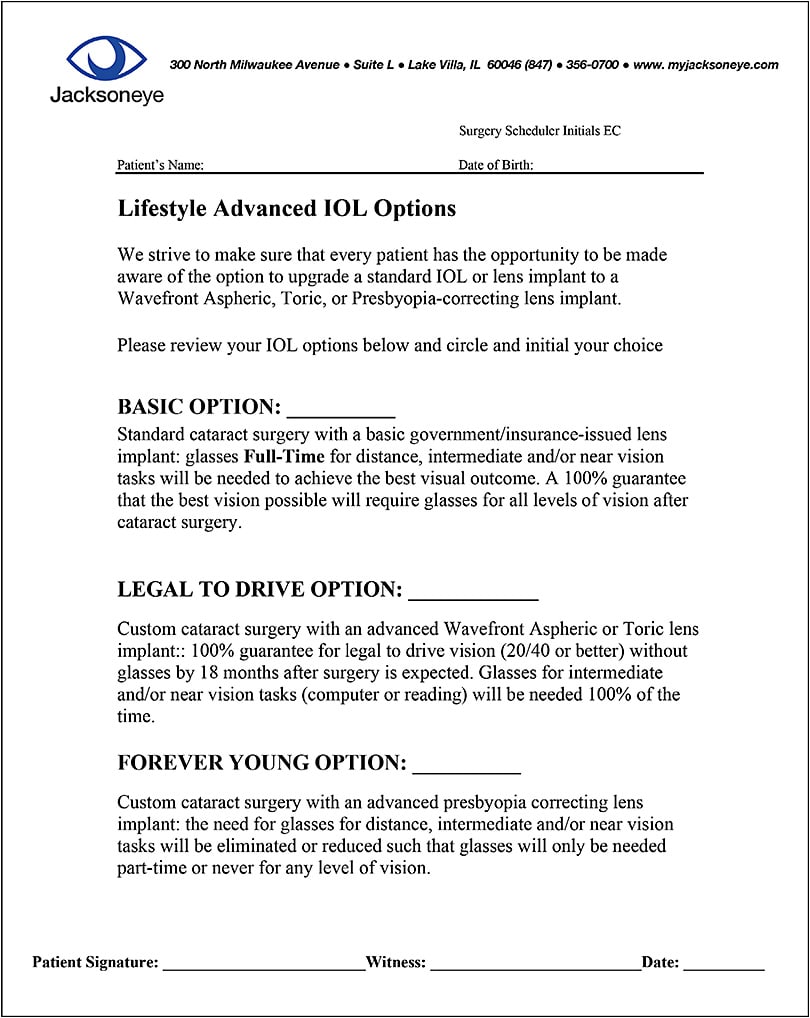
Our scheduling visit is when our surgery coordinator closes on an option presented at the preoperative evaluation. Payments, billing statements, insurance questions, financing, consent forms and repeat diagnostic testing, if necessary, are all done at this visit — the latter especially if ocular surface is being treated to get better diagnostic data prior to surgery. Our surgical options are Basic Basic, Basic LENSAR, Legal to Drive (LTD) and Forever Young (FY), with the last having a nontoric (femtosecond AI) or toric (toric IOL version) option (Figure 2).
Basic LENSAR patients receive astigmatic correction and use of advanced imaging with our LENSAR femtosecond laser per CMS guidelines for collection purposes. Basic Basic (in which the femtosecond laser is not used) and Basic LENSAR patients will still need glasses full time for all levels of activities (distance, intermediate and near) with no promise of any spectacle independence.
The LTD option is our driving-vision option. It aims to give spectacle independence for distance-related activities such that the patient can pass a driver’s vision test for day and/or night vision postoperatively. For monovision patients, we call it LTD monovision and they pay for LTD pricing since we are guaranteeing a refractive outcome.
The FY option is our presbyopia-correcting option, but we always set the expectation that patients will need reading glasses part-time for near-vision tasks in low-light conditions, such as restaurants and for print smaller than J3. More than once, we demonstrate preoperatively to patients what J3 print is. That helps to preempt any postoperative “amnesia” on the subject.
The good news: With this lifestyle approach, 70% to 85% of patients in any given surgical week upgrade to at least Basic LENSAR femtosecond technology.
Lastly, our LTD and FY options also include LENSAR femtosecond treatment (toric IOL alignment with capsular tabs — especially helpful with outcomes) and ORA (Alcon) intraoperative aberrometry (especially helpful with aphakic power selection in postrefractive surgery patients) as part of their packages.
APPROPRIATE DIAGNOSTIC TESTING
Like any other surgical procedure, nothing can go as planned without proper diagnostic objective testing. Not only does objective testing give information to select the correct IOL technology for each patient, but it also protects the surgeon in the exam lane from secondary gainer personalities (those who look to potentially sue a doctor due to subjective complaints that are unfounded, even though they obtained the benefit of the IOL).
Our preoperative diagnostic process is extensive, and we are fortunate to have many technologies at our disposal; however, not all are necessary to be successful. At minimum, corneal topography and tomography (if possible), OCT imaging of the macula, biometry with modern-day IOL formula and some type of ocular surface analysis are critical to reduce enhancements postoperatively.
In our practice, we have corneal topography in the form of OPD-Scan III (Marco). It gives a breakdown of corneal vs. lenticular astigmatism, angle kappa/angle alpha data, mesopic/scotopic pupil size and placido disk mire imaging of the ocular surface. We also have corneal tomography in the form of Cassini (i-Optics) and Pentacam HR (Oculus), both of which give anterior, posterior and total corneal astigmatic values so we approach astigmatism management correctly. Our IOLMaster 700, with its swept-source technology, can read through very dense cataracts and has current IOL formulae (Barrett Universal, Barrett True-K, Haigis-L). It also provides insight into anterior vs. total corneal astigmatism power like the Cassini and Pentacam.
The OPD-Scan III, Cassini and Pentacam all streamline with our femtosecond laser platform LENSAR, using iris registration measured preoperatively and adjust for cyclorotation errors intraoperatively, for more precise astigmatic correction with AIs or toric IOL alignment. Images obtained with any of these three devices preoperatively are placed into the LENSAR either wirelessly or via USB, then astigmatic steep axis alignment for either arcuate incisions or toric IOL alignment are adjusted for cyclorotation errors intraoperatively. Ink marking on the OR table is avoided and more accurate alignment is obtained in this manner. OCT macular imagining is critical to avoid placing a presbyopia-correcting IOL in a patient with macular degeneration, epiretinal membrane or other macular pathology not detectable at the fundus exam. The latter has been controversial, but my approach avoiding these patients with my FY option has led to happier patients, less chair time and less enhancements.
We utilize ocular scatter analysis with our HD Analyzer (Keeler), which can be performed with iTrace (Tracey Technology) as well. Ocular scatter analysis is helpful in assessing when a patient needs a Yag capsulotomy postoperatively, especially in upgraded LTD and FY options before rushing to a laser vision or LRI correction first. I prefer to do Yag capsulotomy before any refractive enhancement, as the refractions can change slightly post-Yag laser treatment. And just doing a simple Yag capsulotomy in a majority of cases eliminates the need for an additional, unnecessary refractive enhancement procedure. I wait a minimum of 4 to 6 weeks post-Yag capsulotomy before deciding on whether additional refractive enhancement is needed.
Also, our Pentacam technology performed preoperatively gives the information necessary to make sure a patient can even undergo a PRK, SMILE or LASIK postoperatively if needed. We have epithelial mapping technology (Zeiss, ArcScan) for the few esoteric, more borderline cases with thinner corneas to make the determination for refractive enhancement, should that situation arise.
Lastly, our practice’s ocular surface assessment includes tear osmolarity (TearLab), MMP-9 (Quidel), dynamic meibomian gland imaging (Keeler, Johnson & Johnson Vision), OPD-Scan III mire imaging, vital dye staining and VBUT scoring (HD Analyzer); the latter is a quantitative measurement of tear break-up time that correlates with visual quality. If we find abnormalities in the ocular surface, we treat the patient and repeat the appropriate tests at scheduled visits before proceeding with surgery — another key step to reducing enhancements postoperatively. This also sets the expectation that the patient had ocular surface disease preoperatively and that the cataract surgery didn’t cause their condition.
One last trick we like to do with our patients in the FY option category is at the 1-week second-eye postoperative exam (so both eyes are at least 1 week postoperative). Whether the patients are happy or not, we show them that their IOL technology is truly working by placing -2.50 sphere “purple” glasses on them to show what their near vision uncorrected would be if they had opted for a monofocal IOL option. It’s a true practice builder and helps patients dissatisfied early in the postoperative process understand that their IOL technology is actually working and that their ocular surface and lighting conditions maybe be affecting their dynamic, not static, near vision needs.
SUMMARY
Setting patient expectations, minimizing and providing proper premium IOL options and utilizing appropriated diagnostic testing typically leads to lower enhancement rates postoperatively, less chair time and happier patients with more referrals. OM









