The ongoing SARS-CoV-2 pandemic has created increasing stressors in the medical practice worldwide. New, complex challenges continue to arise due to increased safety demands, decreasing medical supplies and the secondary global economic downturn. To continue to provide outstanding service, it is important to understand the intricacies of your retina practice. The AAO (www.aao.org/coronavirus ) and the American Society of Retina Specialists (www.asrs.org/practice/asrs-member-alert-regarding-covid-19-pandemic ) have quickly adapted to the ongoing challenges and are regularly updating the guidelines with the current evidence-based strategies regarding transmission and containment.
The following article will provide current clinical management pearls that may optimize your practice during the SARS-CoV-2 pandemic.
Prioritize safety
The United States Surgeon General, the AAO and the ASRS recommend restricting the clinic to patients with urgent or emergent needs to minimize bringing SARS-CoV-2 into our facilities, save personal protective equipment (PPE) and decrease the exposure to medical personnel who may be needed later during the pandemic. Essential encounters include patients receiving intravitreal injections therapy, acute postoperative follow-ups and emergency evaluations.
Telephone triage
New and follow-up patients should undergo telephone triage to ensure that a face-to-face evaluation is appropriate and to ensure that the patient is not at high risk of SARS-CoV-2 infection or has not had contact with any known or suspected SARS-CoV-2 patient. Specific questions regarding fever, shortness of breath, cough and malaise during the last 14 days should be asked. Also, description of the new clinic flow should be explained prior to check-in. Pre-population of the EMR by the technicians may be reasonable to minimize sustained contact with patients during the clinic encounter.
In the clinic
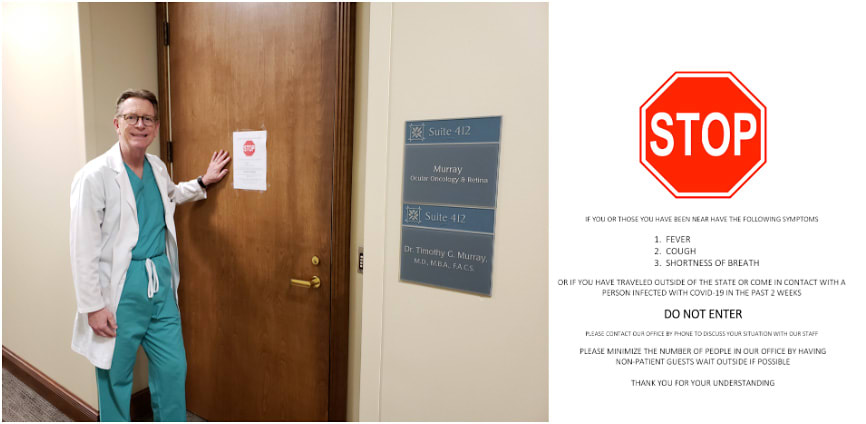
Specific signage (https://www.asrs.org/content/documents/covid-sign-v2-3.20.20.pdf ) should be posted outside of the clinic, asking patients not to enter if they have SARS-CoV-2 symptoms or have been exposed (Figure 1). Patients should be encouraged to enter the clinic alone and for all companions to wait outside whenever possible. The patient clinic time should be minimized and social distancing measures should be in place to allow extra space between patients in the waiting room. Have patients check into the clinic via telephone and wait in their car until their presence is required to optimize the social distancing measures and minimize sustained exposure.
Practices with multiple physicians should consider alternating clinic days to decrease exposure risk and the possibility of having two or more physicians infected by SARS-CoV-2 at a similar time. Clinical and administrative staff should also employ social distancing measures whenever possible.
Intravitreal injections
Patients who typically undergo intravitreal injection therapy are at higher risk of morbidity and mortality if they develop SARS-CoV-2 infection, especially diabetic patients. Special attention should be placed on these encounters.
Switching to a longer-acting intravitreal agent may provide additional safety. Patients receiving treatment on a scheduled basis who have no interval changes in symptoms or visual acuity may undergo intravitreal therapy without dilation or extensive testing. However, patients getting treatment with brolucizumab should continue to be monitored for intraocular inflammation, including anterior segment examination, posterior segment and OCT prior to injection.
High-risk or SARS-CoV-2 patients
Encourage all symptomatic or high-risk patients (ie, high-risk of infection through exposure or travel) for SARS-CoV-2 to stay home, and follow the standard medical recommendations by the Centers for Disease Control and Prevention (CDC) (https://www.cdc.gov/coronavirus/2019-nCoV/index.html ). In the event that a high-risk patient enters the clinic, immediately perform isolation of the patient and undertake further assessment by the physician to determine appropriate management.
Evaluate patients known to have SARS-CoV-2 or deemed to be high-risk in a controlled hospital setting with PPE for the mouth, nose and eyes. All high-risk patients should wear a surgical mask at all times to minimize aerosolization of the virus. Clinical staff should use an N-95 mask, gown, gloves and eye protection (face shield or goggles) to evaluate and perform procedures in patients considered high-risk. The examination room should be thoroughly cleaned after the encounter.
Low-risk patients
To reduce asymptomatic and presymptomatic transmission, all patients, companions and clinic personnel should wear surgical masks (Figure 2). If available, eye protection should also be used by the clinician. Slit lamp shields and not speaking during slit-lamp biomicroscopic examinations are appropriate. The optimal level of PPE and standard guidelines may continue to change depending on the prevalence of SARS-CoV-2 in the community and availability of PPE resources.

Surgery
The ASRS, American College of Surgeons and the CDC recommend that all elective surgery be postponed. However, diseases that carry risk of permanent vision loss without early intervention should be definitively and promptly managed with surgery
Examples of emergent and urgent vitreoretinal pathology include:
- Acute retinal detachment – macula attached
- Acute retinal detachment – macula detached in a monocular patient
- Retained lens fragments with elevated IOP not controlled medically
- Acute endophthalmitis with severe vision loss
- Open globe injury with or without an intraocular foreign body
- Expulsive choroidal hemorrhage
- Dense vitreous hemorrhage in monocular patient
- Exposed/infected scleral buckle or other ocular implant
- Retinal detachment – macula detached
- Retained lens fragment with medically controlled IOP
- Vitreous hemorrhage in which a retinal tear or detachment is suspected
- Malignant intraocular tumors
Telemedicine
The Centers for Medicare & Medicaid Services and other local providers have recently relaxed regulations regarding telemedicine, telephone evaluations and interprofessional consults. Due to the ongoing pandemic, HIPAA compliance has been waved as long as the platform is not public facing. The AAO published guidelines for visual acuity testing at home (https://www.aao.org/eye-health/tips-prevention/home-eye-test-children-adults ) for children and adults that may allow approximation of visual function.
Adopting telehealth consultations could allow retina specialists to better determine who needs face-to-face consultation, review testing, refill medications, provide vital reassurance to patients and minimize the risks associated to exposure. For additional ongoing discussion regarding telemedicine and other SARS-CoV-2 related topics visit the ASRS COVID-19 Corner (https://www.asrs.org/forum/forum15-covid19-corner.aspx ).
Conclusion
It is of outmost importance that retina specialists be conscious about the risks associated to SARS-CoV-2 exposure and to minimize the risk of disease transmission. It is our responsibility as leaders to provide a safe environment to our patients, our staff and our families while treating and preventing visual loss. During these unprecedented times, the optimization of the retina practice to prioritize exposure safety will undoubtedly continue to evolve as the prevalence of SARS-CoV-2 continue to change in our local communities. OM










