Get proactive, and learn to accentuate the positive.
Not everyone who reads this column will agree with me, but I am honestly blown away by the plethora of articles, e-mails and news stories about physician burnout.
After working hard as a pre-med in college, then medical school, internship, residency and sometimes fellowship, what were people expecting the practice of medicine to be? Have you read the articles about burnout in medical school? Residency? Do laborers have a platform from which to complain to their bosses and foremen that they are burned out? Come on.

NOW THE FACTS
Though a smaller percentage than our colleagues in other specialties, 43% of ophthalmologists report being burned out, according to the Medscape Ophthalmologist Lifestyle Report 2017: Race and Ethnicity, Bias and Burnout (tinyurl.com/y3vo8mdw ).
Of course, we work long hours and are responsible for the medical and surgical wellbeing of our patients. Also, many of us are deeply involved in the management of our practices. Even with a chain of command and the buffer of middle management, we are frequently at least aware of (if not involved in) issues of compliance, implementing regulation changes and matters of HR (always the most stressful). Some ophthalmologists pursue other activities in health care, such as clinical research, lecturing, publishing, adjunctive medical school teaching, KOL activities with industry or leadership roles with city, state and federal government as physician advocates.
But isn’t this what we trained for? The practice of medicine has never been static or status quo.
WHAT LEADS TO BURNOUT?
According to another Medscape report, its Ophthalmologist Lifestyle, Happiness & Burnout Report 2019 (tinyurl.com/yxunjzfs ) — these are the chief culprits:
- Bureaucratic tasks (charting, paperwork)
- Government regulations
- EHR
- Insufficient compensation
- Long hours
- Loss of control/autonomy
- Lack of respect from patients
- Lack of respect from employees/colleagues, staff
- Emphasis on profits over patients
- Feeling like just a cog in a wheel
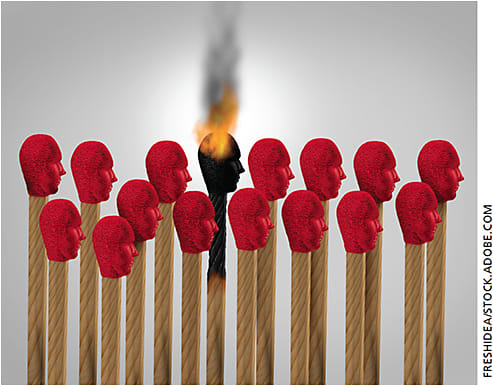
Physicians who report feeling burned out describe themselves as exhausted, depressed, short-tempered, less motivated and less attentive to charting and patient care, making more mistakes than expected. They become exasperated in front of patients and peers. Lateness to work and absenteeism are common.
Sadly, those feelings carry over into physician’s personal lives as well: Medscape’s report found that displacing frustration onto children and spouses occurs frequently, and some respondents admit to feeling suicidal at times (11%).
Most ophthalmologists have not sought help for their feelings of depression or suicidal tendencies, and most are unlikely to participate in workplace programs that seek to alleviate feelings of depression and burnout. Interestingly, Medscape found that 67% of ophthalmologists still report high or very high self-esteem, and 52% describe their marriages as “very good.”
WHAT CAN BE DONE?
Much has been written about what is necessary to reduce or prevent physician burnout, which of course impacts the mood and efficiencies of the staff and workplace.
Here are some of the most commonly suggested remedies for overcoming burnout:
- Follow the “80/20 rule.” Psychologists who study this phenomenon recommend that 20% of a physician’s time be spent on activities of personal interest and enjoyment.
- Create fun functions outside the practice for physicians and staff, and include families sometimes.
- Exercise
- Bring music into the workplace
- Be open about your feelings with practice leadership and family
- Read. Recapturing Joy in Medicine, by Amaryllis Sanchez Wohlever, MD, offers nine steps to creating the organizational foundation for finding joy in medicine; these steps are focused on what the author calls a culture of wellness, efficiency of practice and personal resilience.
FINAL THOUGHTS
I love what I do as an ophthalmologist. Sure, I have “those days” … hostile patients, difficult surgery days, HR issues, full moons, etc. But isn’t this so in every field?
Examining other medical specialties, I feel particularly grateful that I am in ophthalmology — the regulatory burden in primary care, for instance, can be considerably onerous. Now in practice for 29 years, I am more excited than ever about the advances in surgical and clinical care. I consider the practice of medicine in general, and ophthalmology in particular, to be a privilege, and I find complaints of burnout to be annoying. So, in the words of one of my technicians, “Suck it up, Buttercup!” OM









