Here’s another reason why dry eye disease (DED) deserves our attention: The tear film-air interface provides 75% of the refractive power of the eye.1 Align that with the other reasons DED requires treatment — its presence affects preoperative planning, surgical outcomes and patient satisfaction2 — and that requirement could be called a mandate.
DED has been divided into four subtypes: aqueous tear deficiency (ATD); blepharitis/meibomian gland dysfunction (MGD), also known as evaporative; goblet cell/mucin deficiency; and exposure-related dysfunctional tear syndrome. There are also masqueraders, or coconspirators, of DED such as: superior limbic keratoconjunctivitis, topical medication toxicity, Thygeson’s superficial punctate keratitis, mucous fishing syndrome, contact lens-related toxicity, allergic conjunctivitis, conjunctivochalasis, chemical toxicity and floppy eyelid syndrome.3 Nonobvious or obvious anterior basement membrane dystrophy can become more clinically relevant after cataract surgery, and other mechanical diseases like Salzmann’s nodular degeneration should be carefully evaluated for upon slit lamp examination.
The Prospective Health Assessment of the Cataract Patient’s Ocular Surface (PHACO) study found that 87% of patients scheduled for cataract surgery had clinical findings of dry eye but were asymptomatic.4
WHAT DED DOES
DED can impact the preoperative planning of your cataract surgery. An irregular ocular surface can result in topographical aberrations, such as irregular mires, that create artificially steeper Ks and irregular astigmatism. Treating seemingly higher levels of astigmatism can cause an overcorrection and possibly lead to flipping the axis postoperatively.
Cataract surgery itself can exacerbate pre-existing dry eye. Inciting factors include: prolonged intraoperative microscopic light exposure, grooved corneal tunnel incisions, denervation of the cornea, topical anesthesia and drops containing preservatives, such as benzalkonium chloride.5-7 Also, femtosecond-assisted limbal relaxing incisions (LRIs) create intrastromal incisions without disturbing the epithelium, preserving tear film stability and offering patient comfort, unlike penetrating limbal relaxing incisions.8 In a study by Kasetsuwan et al., which analyzed the incidence of postoperative dry eye one week following phacoemulsification, 68.4% had reduced TBUT, 11.9% had a diminished Schirmer 1 score without anesthesia, and 9.8% had dry eye based on the Ocular Surface Disease Index (OSDI) score.9
ESTABLISHING AND MANAGING DED
There are myriad methods to assess dry eye subjectively. Visual-function questionnaires are useful tools. The OSDI is a 12-item questionnaire that rapidly assesses and categorizes DED severity into normal, mild, moderate and severe, based on a scoring algorithm. The score is scaled from 0-100 with higher values indicating more severe disease; values ≥ 13 indicate DED.10 (For more DED diagnostics, see page 24.)
After establishing the diagnosis of dry eye and classifying the subtype(s), the next step is to outline its management (Table 1, page 22).3 Artificial tears are indicated for all subtypes of DED. They lubricate the surface, remove debris, reduce elevated pro-inflammatory mediators, dilute a hyperosmolar tear film and supplement deficient components of the tear film.3 For those with moderate to severe dry eye, it is recommended to use preservative-free artificial tears at least four times per day. While artificial tears provide improvement of subjective symptoms and objective findings, they will not resolve dry eye on their own for the majority of patients.
| SUBTYPE | AQUEOUS TEAR DEFICIENCY | BLEPHARITIS/MGD | EXPOSURE-RELATED | GOBLET CELL/MUCIN DEFICIENCY |
|---|---|---|---|---|
| Clinical findings |
|
|
|
|
| First line |
|
|
|
|
| Second line |
|
|
|
|
| Procedures |
|
|
|
|
| Adapted from: Milner MS, Beckman KA, Luchs JI, et al. Dysfunctional tear syndrome: dry eye disease and associated tear film disorders – new strategies for diagnosis and treatment. Curr Opin Ophthalmol. 2017;28:3-47. | ||||
The first-line treatments for DED (ATD, MGD and goblet/mucin deficiency) are artificial tear supplements and topical anti-inflammatories (Table 1).3 Anti-inflammatory therapies have been proven to be efficacious for moderate to severe evaporative dry eye and ATD. Topical cyclosporine A (Restasis, Allergan) 0.05% works by inhibiting cytokine production from activated T lymphocytes, reducing conjunctival goblet cell loss and epithelial apoptosis. An early response can be observed at six weeks; however, it may take at least six months to see an improvement. Donnenfeld et al. studied the effects of cyclosporine compared to preservative-free artificial tears (PFAT) following phacoemulsification and implantation of multifocal IOLs. They found that the cyclosporine group had an improved mean uncorrected distance visual acuity (UCDVA) of 20/25 compared to the artificial tear group with mean UCDVA of 20/30 (P=0.45). Mean best-corrected distance visual acuities (CDVA) were 20/20 in the cyclosporine group compared to 20/25 in the PFAT group (P=0.005). They also noted improved contrast sensitivity, conjunctival staining and TBUT.11
Because it takes time to reap the full benefits of cyclosporine, several clinicians have found using an NSAID or topical steroid helps with the burning and stinging12 of cyclosporine until the induction period is complete. Topical loteprednol QID can be used for two weeks to begin subjectively and objectively improving the ocular surface for preoperative measurements while waiting for anti-inflammatory medications to take effect.13
Lifitegrast (Xiidra, Shire) 5.0% is the newest FDA- approved medication for DED. It is an intracellular adhesion molecule-1 (ICAM) decoy that blocks the binding interaction of lymphocyte function-associated antigen-1 (LFA-1). This inhibits T-cell recruitment, activation and proinflammatory cytokine release associated with DED. Studies involving lifitegrast have shown improvement in dry eye symptoms by day 14.14 Irritation and discomfort can occur with application; the most common nonocular side effect is dysgeusia.
Warm compresses and eyelid scrubs such as Avenova (NovaBay Pharmaceuticals) or OcuSoft scrubs (OCuSOFT) are also first-line therapies for MGD. Other options include LipiFlow (J&J Vision), which uses thermal pulsation to liquefy and express meibum; it works well preoperatively. Clinical studies have shown improvements in OSDI scores and meibomian secretion scores. However, LipiFlow is not for everyone, including patients who do not have sufficient glands to perform a lid expression; at least six lower lid glands, open to some degree, are generally required.15
More DED diagnostics
Objective data include:
- TBUT≤ 10s
- positive ocular surface staining with fluorescein or lissamine green (Figure 1, page 22)
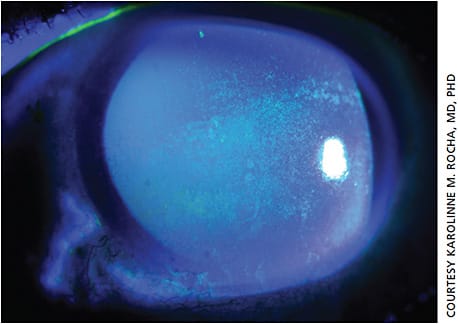
Figure 1. Slit lamp photo of diffuse punctate fluorescein stain consistent with severe keratoconjunctivitis sicca. - Schirmer test I ≤10 mm after five minutes
- tear film meniscus height ≤0.3 mm
- lagophthalmos
- eyelid laxity
- MGD
- ocular scatter, a property of light as it travels through the optical media of the eye that is heterogenous, results in localized deviations of light due to a combination of diffraction, reflection and refraction. The HD Analyzer (Visiometrics) uses double-pass wavefront aberrometry to measure the Objective Scattering Index (OSI) and higher-order aberrations. It achieves this by analyzing information from the retinal image point-spread function. An OSI >1 indicates light scatter due to conditions such as tear film instability or early cataract, which can be diagnosed preclinically (Figures 2 and 3, page 42).1
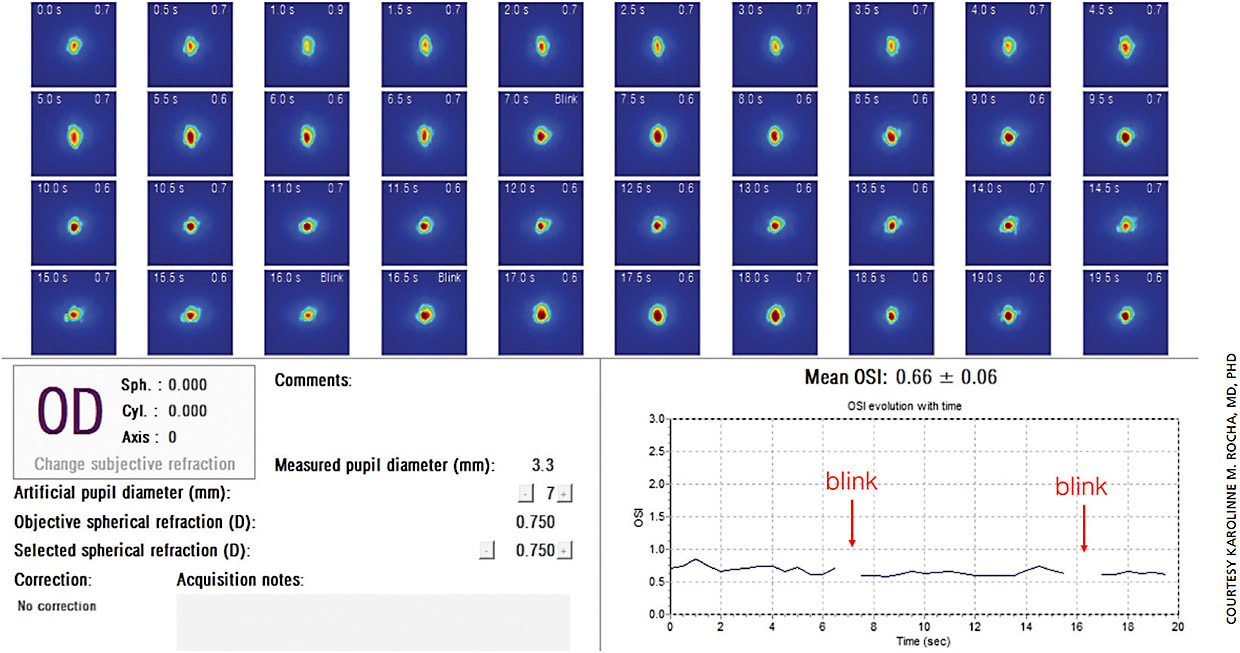
Figure 2. Post-LASIK patient is a 35-year-old female. Shown is the dynamic measurement of the point-spread function that spans a 20-second interval. 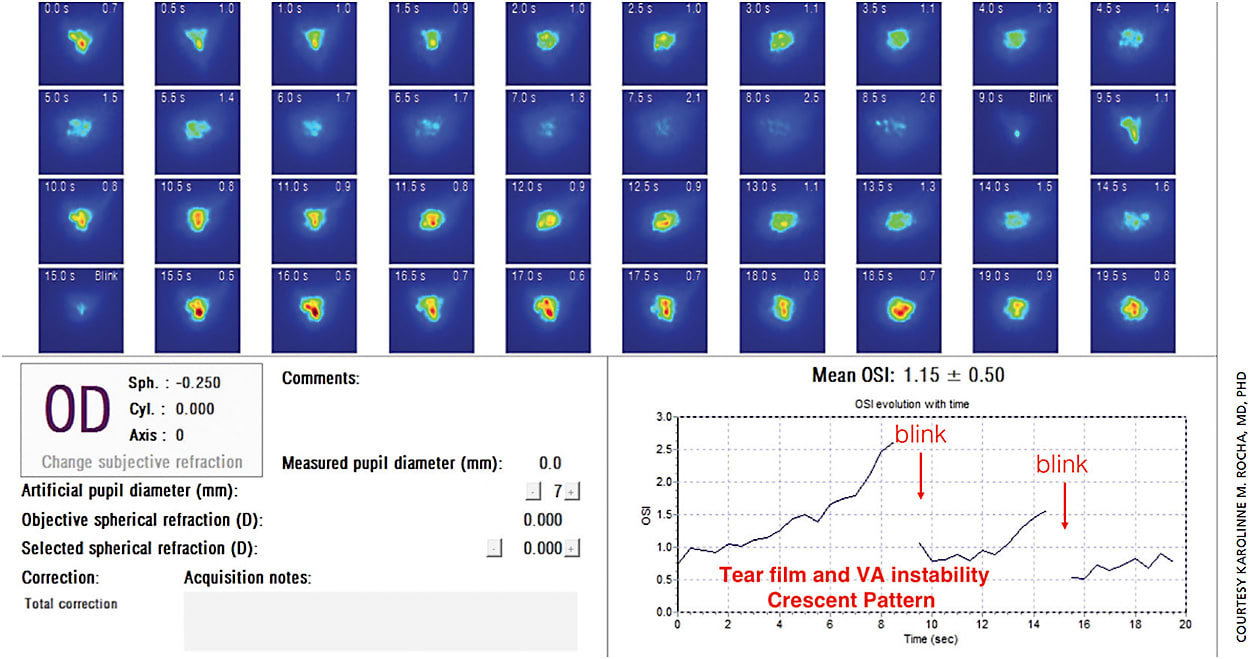
Figure 3. Tear film instability in this unhappy multifocal IOL patient is shown in the dynamic measurement of a point-spread function spanning a 20-second interval. - tear osmolarity: values ≥ 308 mOsm/L or asymmetry of 8 mOsm/L or more are indicative of hyperosmolarity.2
REFERENCES
- Piñero DP, Ortiz D, Alio JL. Ocular scattering. Optom Vis Sci Off Publ Am Acad Optom. 2010;87:E682-696.
- Schallhorn S. Quality of vision and life following LASIK. Paper presented at: The American Academy of Ophthalmology Annual Meeting; Nov. 11, 2012; Chicago.
Punctal plugs are another useful tool with improved corneal staining, prolonged TBUT, decrease in tear osmolarity and increase in goblet cell density. Contraindications include allergies to plug material, nasolacrimal duct obstruction and canaliculitis or dacryoadenitis. It has been suggested that clinical ocular surface inflammation is a contraindication because it can cause prolonged contact of abnormal tears containing proinflammatory cytokines with the ocular surface.16 However, it is reasonable to treat your patient with an anti-inflammatory for several weeks prior to inserting a punctal plug.
Tetracyclines, such as doxycycline, are used for their anti-inflammatory properties. They inhibit matrix metalloproteinases and collagenases. Clinical studies of oral tetracycline agents found a significant improvement of reported symptoms and ocular inflammation/irritation. However, a five-day course of azithromycin (500 mg for day one, then 250 mg for the remaining four days) showed greater improvements in ocular surface staining, redness and shorter duration of treatment compared to doxycycline 200 mg once a day.17,18
Omega-3 fatty acids and other nutritional supplements have been found to be useful in ATD and MGD. There were significant improvements in OSDI scores and objective evaluations of corneal smoothness in those taking supplements of gamma-linolenic acid and omega-3 fatty acids in patients with moderate to severe dry eye compared to placebo. Studies regarding optimal dosage and formulation are ongoing.3,19
CONCLUSION
DED is a critical component of patient satisfaction and optimal surgical outcomes. It consists of multiple subtypes that overlap with each other. DED is often overlooked due to many patients being asymptomatic and will likely worsen following cataract surgery. After implementation of your initial treatment plan, it is a good idea to wait four to six weeks before reassessing and augmenting the plan. If the patient is still symptomatic, you can continue to expand upon the plan with additional therapies until the right combination is found. When dealing with an unhappy postoperative patient, remember the “big three” — DED, residual refractive error and posterior capsule opacification.20 It is important to diagnose and treat DED preoperatively while it’s still “the patient’s problem.” If diagnosed postoperatively, then it becomes the doctor’s problem. Treating DED can be challenging, but thankfully there are many diagnostic and therapeutic tools to help our patients. OM
REFERENCES
- Rolando M, Zierhut M. The ocular surface and tear film and their dysfunction in dry eye disease. Surv Ophthalmol. 2001;45:S203-S210.
- Xie C, Garg S. Cataract surgery and dry eye update. Ophthalmology Management. 2017; 21: 28-30.
- Milner MS, Beckman KA, Luchs JI, et al. Dysfunctional tear syndrome: dry eye disease and associated tear film disorders – new strategies for diagnosis and treatment. Curr Opin Ophthalmol. 2017;28:3-47.
- Trattler WB, Majmudar PA, Eric D Donnenfeld ED, et al. The prospective health assessment of cataract patients’ ocular surface (PHACO) study: the effect of dry eye. Clin Ophthalmol. 2017;11:1423-1430.
- Cho YK, Kim MS. Dry Eye After Cataract Surgery and Associated Intraoperative Risk Factors. Korean J Ophthalmol. 2009;23:65.
- Hiroko B. Cataract Surgery in the Presence of other ocular comorbidities. In: Cataract Surgery: Technique, Complication and Management. 1st ed. Saunders; 2004.
- Fine IH, Hoffman RS, Packer M. Profile of clear corneal cataract incisions demonstrated by ocular coherence tomography. J Cataract Refract Surg. 2007;33:94-97.
- Donnenfeld E, Rosenberg E. Assisting femto incisions with nomograms: Treat corneal astigmatism during cataract surgery. Ophthalmology Management. 2015. June; 19: 48-52.
- Kasetsuwan N, Satitpitakul V, Changul T, Jariyakosol S. Incidence and pattern of dry eye after cataract surgery. PLoS One. 2013 Nov 12;8:e78657. Accessed Mar. 10, 2018.
- Schiffman RM, Christianson MD, Jacobsen G, Hirsch JD, Reis BL. Reliability and validity of the Ocular Surface Disease Index. Arch Ophthalmol. 2000;118:615-621.
- Donnenfeld ED, Solomon R, Roberts CW, et al. Cyclosporine 0.05% to improve visual outcomes after multifocal intraocular lens implantation. J Cataract Refract Surg. 2010 Jul;36(7):1095-100.
- Schultz C. Safety and efficacy of cyclosporine in the treatment of chronic dry eye. Ophthalmol Eye Dis. 2014; 6:37-42.
- Sheppard JD, Donnenfeld ED, Holland EJ, et al. Effect of loteprednol etabonate 0.5% on initiation of dry eye treatment with topical cyclosporine 0.05%. Eye Contact Lens. 2014;40:289-296.
- Holland EJ, Luchs J, Karpecki PM, et al. Lifitegrast for the treatment of dry eye disease: results of a phase III, randomized, double-masked, placebo-controlled trial (OPUS-3). Ophthalmology. 2017 Jan;124:53-60.
- Greiner JV. Long-term (3 year) effects of a single thermal pulsation system treatment on meibomian gland function and dry-eye symptoms. Eye Contact Lens 2015 Jul 28.
- Management and Therapy of Dry Eye Disease: Report of the Management and Therapy Subcommittee of the International Dry Eye WorkShop (2007). Ocul Surf. 2007;5:163-178.
- Kashkouli MB, Fazel AJ, Kiavash V, Nojomi M, Ghiasian L. Oral azithromycin versus doxycycline in meibomian gland dysfunction: a randomised double-masked open-label clinical trial. Br J Ophthalmol. 2015;99:199-204.
- Frucht-Pery J, Sagi E, Hemo I, Ever-Hadani P. Efficacy of doxycycline and tetracycline in ocular rosacea. Am J Ophthalmol. 1993;116:88-92.
- Ji J. Omega-3 essential fatty acids therapy for dry eye syndrome: A meta-analysis of randomized controlled studies. Med Sci Monit. 2014;20:1583-1589.
- Woodward MA, Randleman JB, Stulting RD. Dissatisfaction after multifocal intraocular lens implantation. J Cataract Refract Surg. 2009;35:992-997.










