TrueTear encourages higher performance from the lacrimal functional unit in DED patients.
We all have dry eye disease (DED) patients who, despite being compliant with your recommendations, are only somewhat better and still complain about dryness and visual compromise. For these patients, we now have a new approach that is drug free, drop free and puts control back into the patients’ hands. TrueTear (Allergan) is the first FDA-approved device for uniquely addressing the neurosensory component of DED. The prescription device’s tip sends tiny pulses of energy to the nasociliary nerve along the nasal septum, causing the eyes to temporarily increase complete tear production.
AT THE HEART OF DED
The TFOS DEWS II definition of DED1 reflects an expanded understanding of the underlying issues with chronic DED: “Dry Eye is a multifactorial disease of the ocular surface characterized by a loss of homeostasis of the tear film and accompanied by ocular symptoms, in which tear film instability and hyperosmolarity, ocular surface inflammation and damage and neurosensory abnormalities play etiologic roles.”
The components underlined above help me organize my thinking and approach to both the simple and complex DED patient. With this in mind, it is clear where TrueTear, a neural stimulation device, fits into your DED armamentarium.
- Discomfort and blurred vision. Tear film instability and ocular symptoms are considerations in patients with complaints of discomfort and blurred vision. The 20/20 unhappy patient is more than likely experiencing optical aberrations from an unstable tear film and/or irregularities in the corneal epithelium (e.g. superficial punctate keratitis [SPK]). Shizuka Koh, MD, PhD, described how subjective visual symptoms of dry eye correlate well with objective optical quality measures.2 For example, blurred vision is related to increases in higher order aberrations (HOA) and backward light scatter from SPK. Glare is related to forward light scatter from tear film instability. Fluctuating vision with blinking is from stability of post-blink HOA.
- Hyperosmolarity and inflammation. DED is a Double Vicious Circle:3 As the lacrimal fluid production begins to decline due to inflammation and/or the evaporative load increases as a cause or consequence to inflammation, the osmolarity of the tear film increases. The Double Vicious Circle also works in the reverse. The point is that inflammation begets inflammation, and, whether you start with aqueous deficiency or evaporative dry eye, pathophysiologically speaking, it is an endless chicken-and-the-egg debate.
- Loss of homeostasis and neurosensory abnormalities. The lacrimal functional unit (LFU) is comprised of the corneal nerves, corneal nociceptors, afferent nerves, central nervous system relays as well as efferent command signals to the lacrimal gland, meibomian glands and goblet cells. The system is designed to maintain perfect homeostatic control of the pre-corneal tear film for maximal environmental protection, stability, defense and visual performance. The system suffers under the pressures of chronic, self-perpetuating inflammation found in DED. Acute phase cytokines IL-1 and TNF induce an increase in nerve growth factor (NGF) from the limbal cells in response to injury, which quickly promotes healing after acute injury. The problem with chronic inflammation of DED is that NGF is constantly upregulated and the low affinity and high affinity NGF receptors have apoptotic effects on the corneal epithelium and the corneal sub-basal plexus, respectively.4 The result is a damaged front-line epithelial barrier and neurosensory abnormalities (sub-basal plexus dysmorphology as seen in confocal studies).
A UNIQUE APPROACH
Until recently, we corrected this chronic inflammation-induced epithelial and subbasal plexus damage with topical immunomodulators.4 Alternatively, the TrueTear neural stimulation device provides a method of orchestrating a complete tear letdown via the normal neuroanatomic loop of the nasociliary nerve to the brainstem and the resultant command impulses to the LFU components — sort of like entering the house through the back door. This method requires that the neural pathways and complete tear producing subcomponents (lacrimal glands, meibomian glands and goblet cells) be intact. Clinically, I find the neural stimulation effect is enhanced by optimizing the tear producing apparatus as much as possible via traditional therapeutics and procedures.
The neural stimulation approach is unique in our armamentarium. Patients report, “It’s the first tears I’ve had in years!” as I see an increased tear meniscus appear in in-office demos.
PATIENT SELECTION
I find this approach is appreciated in patients with any known or predicted insult to the front line of the LFU: the corneal sub-basal plexus.4 I have used TrueTear in clinical categories of damaged sub-basal plexus situations, such as postsurgical changes (LASIK, PRK, cataract surgery), neuropathic changes (diabetes, neurotrophic corneas), chronic inflammation and/or hyperosmolarity changes (dry eye, Sjogren’s) and more.
Also, I don’t hold back offering this technology to the younger, healthier patients. Patients who want a drug-free, drop-free approach to dry eye management readily accept TrueTear. The device allows patients to stimulate physiologically complete tear production in environmental stresses, such as walking the dog in the wind, going for a run, long computer sessions, long flights or poor air quality conditions. The healthy patient with an intact LFU can effortlessly adjust tear production and composition under all of these conditions. TrueTear uniquely allows patients an active method for addressing the neurosensory abnormalities of the LFU in DED.
RESULTS
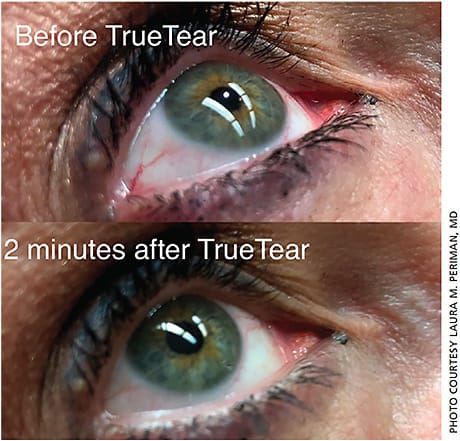
The approximately 50 or so patients to which I’ve prescribed TrueTear have reported high satisfaction as well as some interesting observations. Also, I’ve observed several examples of 1-2 lines of improved VA after in-office demonstration of TrueTear. Other observations include immediate improvements in dryness, improvements in eye redness (Figure 1, page 56), decreased need for artificial tears, improved visual performance (and in some cases improved BCVA), improved sensitivity to light, long-lasting tears with prolonged relief and even improvements in nasal congestion (helpful for allergic conjunctivitis and allergic rhinitis dry eye cases).
This new strategy along with continued optimization of the lacrimal glands, meibomian glands and goblet cells has enhanced my clinical successes with DED patients of varying levels of severity. OM
REFERENCES
- Craig JP, et al. TFOS DEWSII Definition and Classification. Ocul Surf. 2017;15(3):276-283.
- Koh, S. Mechanisms of Visual Disturbance in Dry Eye. Cornea 2016 Nov;35:S83-S88.
- Baudoin C, Messmer EM, Aragona P, et al. Revisiting the vicious circle of dry eye disease: a focus on the pathophysiology of meibomian gland dysfunction. BJO 2016 100:300-306.
- Laccheri B, Torroni G, Cagini C, et al. Corneal confocal scanner laser microscopy in patients with dry eye disease treated with topical cyclosporine. EyeNature. 2017;31(5):788-794.









