As a retina-only practice back in the days before injections for vascular macula diseases, I was on the hunt for a technology to treat diabetic macular edema (DME) and macular drusen. After striking up a conversation with an Iridex representative at a Vitreous Society meeting 16 years ago, I became an early adopter of 810-nm MicroPulse technology. Later, I switched to 577-nm MicroPulse when it became available as a treatment mode in the Iridex IQ 577 laser system. The technology is a low-energy, selective intraretinal pigment epithelium (intra-RPE) microsurgery that allows surgeons to create subtle, well-defined, sublethal intra-RPE injury within pre-determined limits; the injury is reversible by endogenous repair mechanisms, such as the upregulation of beneficial biological factors (HSP70,1 PEDF,2 TSP1,3 SDF4 and ß-actin4).
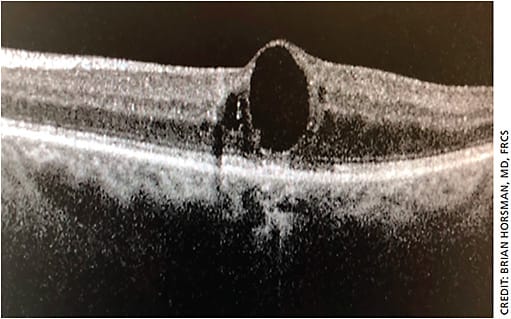
MicroPulse spares the retina and choroid from collateral heat damage and does not leave any visible lesions when viewed ophthalmoscopically with fluorescein angiography (FA), autofluorescence imaging or optical coherence tomography (OCT) imaging. Randomized studies have demonstrated the therapy’s safety and efficacy for the treatment of DME.5-8 It has proven effective, efficient and good for my patients, as well as for my practice’s bottom line.
REDUCING PATIENT BURDEN
First, the data
A recent retrospective study conducted at the University of California, Davis, compared 19 eyes with DME treated with 577-nm MicroPulse laser therapy and ranibizumab to a matched control group of 19 eyes treated with ranibizumab injections alone.9 At 12 months, improvement in visual acuity was comparable in both groups, while those treated with laser had significantly fewer ranibizumab injections (1.7+2.3 vs. 5.6+2.1, respectively). At the end of follow-up, the MicroPulse-treated group maintained a significantly lighter injection burden of 2.6+3.3 vs. 9.3+5.1 (P<.001 for both). The researchers demonstrated that this laser therapy is a safe and effective treatment for DME that may achieve comparable improvement in visual acuity along with a significant reduction in the burden of anti-VEGF injections.
In another study, 46 patients with treatment-naïve cystoid macular edema (CME) due to branch retinal vein occlusion (BRVO) were treated with either 577 nm MicroPulse laser and intravitreal ranibizumab (IVR) (22 patients) or IVR monotherapy (24 patients). At six months, BCVA and central retinal thickness improved in both groups and were not significantly different between the two groups. However, the number of injections during the initial six months in the IVR monotherapy group (2.3±0.9) was significantly greater (P=.034) than that in the IVR and MicroPulse group (1.9±0.8).
In my clinic
Prior to implementing MicroPulse, I performed approximately 50 anti-VEGF injections each day on patients with central DME, retinal vein occlusion (RVO), wet AMD, central serous retinopathy (CSR) and proliferative diabetic retinopathy (PDR). Once I began utilizing this therapy, my rate of injection dropped to roughly five times daily.
With an estimated 70% success rate, my wet AMD laser patients continue to do well with few recurrences of leaking choroidal vessels. Adding MicroPulse laser therapy reduced my patients’ injection burden, which meant less cost, fewer office visits and less anxiety over the anticipation of a needle in their eye. Further, the therapy is well tolerated and requires only approximately two minutes. By adding in MicroPulse laser therapy, I increase the period of time between injections, thus putting off atrophy and potentially prolonging vision. The main benefit of this therapy is a “dry” macula and preservation of vision.
DIAGNOSTICS AND TREATMENT
First steps
Initial and follow-up retinal angiography using the Heidelberg Retina Angiogram (HRA) is required to monitor the activity of all vascular macular diseases. After obtaining initial fluorescein and indocyanine green (ICG) angiograms and OCT, I start treatment with anti-VEGF injection for new patients or for new recurrence of choroidal neovascular membranes (CNVM) and add MicroPulse within one to two weeks.
Next, I follow with a new FA. Depending on the level of CNVM activity after six to eight weeks, I perform a fluorescein angiogram and ICG angiography and OCT.
The FA and ICG angiograms and OCT imaging are essential for this to work. To make rational decisions on what type, if any, treatment to consider, one must have real-time blood flow imagery. In my practice, I see 35 to 42 patients and do 20 to 30 angiograms per day (some patients receive bilateral injections). Angiograms are vital for the success of this treatment to assess essential information about activity of the CNVM.
Beyond edema
In addition to treating DME and macular edema due to BRVO, I use MicroPulse laser therapy to treat both wet and dry AMD as well as PDR and CSR. I do not perform it on retinal tears or holes because I want the thermal effects achieved by continuous wave laser. The success of this laser therapy, in terms of less edema, is least effective in ischemic RVO due to ischemia of the retinal circulation. For both RVO and DME, if the response to anti-VEGF is suboptimal, I proceed to implant Ozurdex (Allergan) into the vitreous plus conduct MicroPulse laser grid treatments, which have proven very effective at decreasing macula edema in both RVO and DME. Typically, I see choroidal neovascularization dry up with one or two initial anti-VEGF injections and MicroPulse laser treatments. I perform this laser over the fovea for all macular grids, and I repeat it at four-to-six-month intervals to prevent CNVM recurrence.
Treatment parameters for all indications
My treatment plan initiated at patient presentation begins with intravitreal injection of anti-VEGF drug followed by macular grid MicroPulse laser treatments with the IQ 577 yellow laser within two to four weeks.
My laser parameters are as follows: 500-µ spot size, 300 milliseconds duration, and 500 mw power; 450 laser applications given. My duty cycle is set to 5%, and I do not titrate power. These parameters are safe and effective for macular treatments. In my experience, titration of power leads to overtreatment and RPE or macular damage. Additionally, I use an Area Centralis HD lens (Volk Optical), topical anesthesia and gel tear coupling agent.
RETINAL PATHOLOGY PROTOCOLS
CNVM
CNVM includes patients with wet AMD and myopic macular degeneration, including idiopathic presentations. I perform a dilated exam, FA, ICG and OCT and inject the anti-VEGF drug.
I perform MicroPulse laser within two to four weeks (while the anti-VEGF drug is at peak effectivity). Patient follow-up exam at six to eight weeks includes new FA, ICG and OCT diagnostics. About 70% of these patients require no further injections of anti-VEGF. I continue laser therapy maintenance every two to six months; most patients require maintenance laser every four to six months, while few need laser every two months.
RVO
First, I perform FA and OCT to map the vascular injury. For mild to moderate ischemia and CME, I proceed with an anti-VEGF injection. For severe ischemia or CME, I administer Ozurdex injection (Allergan). Two to four weeks later, I follow with MicroPulse laser therapy.
DME
I begin with MicroPulse laser and a follow-up FA and OCT six to eight weeks later. Many of my DME patients respond poorly to anti-VEGF; however, I continue MicroPulse laser to dry the macula on both FA and OCT. If the laser therapy does not resolve the edema, I add anti-VEGF injection. Ozurdex injection plus MicroPulse effectively controls DME. MicroPulse laser for exudates may take six to 12 months to see a response after two to three laser treatments.
PDR
I perform panretinal photocoagulation by indirect ophthalmoscopy with the IQ 577 laser in its MicroPulse treatment mode. Patients receive a topical anesthesia and 800 to 1,000 applications in one session. At the follow-up appointment, I obtain a wide-field FA and OCT. For rubeosis or vitreous hemorrhage, I forego MicroPulse laser and use continuous-wave laser with peribulbar block 2% lidocaine.
CONCLUSION
I consistently witness good outcomes for my patients when employing MicroPulse laser therapy. Patients with sight-threatening pathology see the benefit of an extended vision timeline, fewer injections and less time in the office. OM
REFERENCES
- Inagaki K, Shuo T, Katakura K, Ebihara N, Murakami A, Ohkoshi K. Sublethal photothermal stimulation with a micropulse laser induces heat shock protein expression in ARPE-19 cells. Journal of ophthalmology. 2015;6:1-9.
- Ogata N, Tombran-Tink J, Jo N, Mrazek D, Matsumura M. Upregulation of pigment epithelium-derived factor after laser photocoagulation. Am J Ophthalmol. 2001;132:427-429.
- Binz N, Graham CE, Simpson K, Lai YK, Shen WY, Lai CM, Speed TP, Rakoczy PE. Long-term effect of therapeutic laser photocoagulation on gene expression in the eye. FASEB J. 2006;20:383-385.
- Yu AK, Merrill KD, Truong SN, Forward KM, Morse LS, Telander DG. The comparative histologic effects of subthreshold 532- and 810-nm diode micropulse laser on the retina. Investigative Ophthalmology & Visual Science. 2013;54:2216-2224.
- Vujosevic S, Bottega E, Casciano M, Pilotto E, Convento E, Midena E. Microperimetry and fundus autofluorescence in diabetic macular edema: Subthreshold micropulse diode laser versus modified early treatment diabetic retinopathy study laser photocoagulation. Retina. 2010;30:908-916.
- Lavinsky D, Cardillo JA, Melo LA Jr., Dare A, Farah ME, Belfort R Jr. Randomized clinical trial evaluating mETDRS versus normal or high-density micropulse photocoagulation for diabetic macular edema. Invest Ophthalmol Vis Sci. 2011;52:4314-4323.
- Vujosevic S, Martini F, Longhin E, Convento E, Cavarzeran F, Midena E. Subthreshold micropulse yellow laser versus subthreshold micropulse infrared laser in center-involving diabetic macular edema: Morphologic and functional safety. Retina. 2015; 35:1594-1603.
- Venkatesh P, Ramanjulu R, Azad R, Vohra R, Garg S. Subthreshold micropulse diode laser and double frequency neodymium: Yag laser in treatment of diabetic macular edema: A prospective, randomized study using multifocal electroretinography. Photomed Laser Surg. 2011;29:727–733.
- Moisseiev E, Abbassi S, Thinda S, Yoon J, Yiu G, Morse LS. Subthreshold micropulse laser reduces anti-VEGF injection burden in patients with diabetic macular edema. European journal of ophthalmology. 2018;28:68-73.









