Since the FDA approved the first ring-shaped corneal inlay two years ago, early adopters of these near-vision correction devices have found that implanting them can substantially boost your practice.
GOOD POINTS TO MAKE
Inlays are typically implanted as an add-on to laser vision correction surgery. So far, two have received FDA approval: AcuFocus’ Kamra, in April 2015 and almost a year later ReVision Optics’ Raindrop.
Ophthalmic surgeons say these inlays offer several patient benefits, including:
- Fast results — some patients read better a few minutes post-procedure than they did preprocedure, while others gradually improve up to 12 weeks.
- The inlay is undetectable so it doesn’t change the patient’s appearance. “The Raindrop inlay requires just a small flap,” says Shilpa D. Rose, MD, of Whitten Laser Eye in Washington, D.C., whose firm offers both inlays.
- Once it’s healed, even an ophthalmologist can barely see the inlay. “I show my [ophthalmologist] partners … and they have a hard time finding it,” she says.
- Stereopsis is maintained.“There’s extensive gain without losing anything,” says Luke Rebenitsch, MD, of ClearSight LASIK in Oklahoma City. “With previous technologies like monovision, patients had to give something up in order to gain near vision.”
NOT-SO-GOOD POINTS TO MAKE
Corneal inlays have small downsides. Patients have to remain on lubricating eye drops typically for a minimum of three months after the procedure. William Wiley, MD, of the Cleveland Eye Clinic, uses dissolvable punctual plugs during the inlay placement to help. There’s also a small risk of rejection and the subsequent need to remove the inlay.
FINDING YOUR PERFECT (PATIENT) MATCH
As with other procedures, patient selection is key to success. The ideal candidate is the emmetropic presbyope with great distance vision but who is starting to have difficulty with reading vision, says Shamik Bafna, MD, of the Cleveland Eye Clinic.
“Initially, we thought that these were the patients we were going to cater to,” he explains, but he and his colleagues soon realized that these patients don’t come to the office. Instead, they buy inexpensive pairs of reading glasses at the local drugstore.
Now his practice targets LASIK patient-consults who also are presbyopic. “We already have a pool of patients who come in for laser eye surgery,” Dr. Bafna says.
If the patients are in their 40s or 50s and presbyopic, Dr. Bafna tells them he can correct for distance vision in both eyes. But, they will trade their existing pair of glasses for reading glasses. Once they understand how inlays work, Dr. Bafna says, patients gravitate to them.
For Dr. Rose, “Someone who [says], ‘I want to be completely independent of glasses and [then] adds, ‘I don’t want glasses for anything’ is probably not your ideal patient.” She refers to inlay placement as more of a lifestyle procedure. If patients want to decrease dependency on glasses for activities like looking at their watch, cell phone or food, “this is where the inlay comes to be very beneficial.”
Dr. Rose also advises her peers to look for patients who are excited about new technology in general and those who are motivated to continue with follow-up appointments and use artificial tears as prescribed.
STEPS TO PRACTICE SUCCESS
Incorporating inlays is a definite practice-builder, say Drs. Rose and Rebenitsch. Since adding Kamra, Dr. Rebenitsch says practice revenue from presbyopia patients has increased from 5% to 35%. When a practice adds inlays, he says, it is enlarging an entire market segment along with refractive lens exchange and monovision.
Patients who are not appropriate inlay candidates could still sign on for clear lens extraction or LASIK alone.
Surgeons interviewed for this story offered the following tips to build a successful corneal inlay practice:
Set appropriate patient expectations.
Unlike LASIK, where patients may get a “wow” effect the next day, inlays may have a gradual journey to improved vision, Dr. Bafna says.
“It may take patients two to three months to get to their final best vision, but every week that goes by it keeps getting better and better.”
“I tell patients, ‘I can’t make you 20 again, but I can make life better for you,’ ” adds Dr. Rose. “Then the patients are really satisfied because they knew what they were going to get.”
James Kelly, MD, of Kelly Vision Center in New York, N.Y., tells his patients that their near vision “will start off close, maybe within 12 inches of their eyes, but then over the first few months will gravitate toward the normal reading vision distance of around 18 to 20 inches.”
Also, while the procedure helps patients to read text messages, it’s not designed to help them read tiny print such as that on the back of an eye-drop bottle. Be sure to warn your patients that for that task, they might still need their reading glasses.
Inlay specs
Kamra is designed for the surgical treatment of presbyopia in patients 45 to 60 years old who do not require distance correction, have not undergone cataract surgery and require a near correction of +1.00 D to +2.50 D.1 The device, acting like a pinhole, has a central aperture of 1.6 mm that blocks bending rays of light, thereby increasing depth of field while minimizing the impact on distance vision.2
In June 2016, the FDA approved ReVision Optics’ Raindrop, which aims to alter the shape of the cornea to modify its refractive power. Raindrop is a clear device made of a hydrogel material and is indicated for use in patients 41 to 65 years old. In addition to not having had cataract surgery, potential candidates for this inlay include those who cannot focus clearly on near objects or small print and who need reading glasses in strengths of +1.50 D to +2.50 D, but do not need glasses or contacts for clear distance vision.3
Let patients see a glimpse of the future.
To simulate sight with the Raindrop inlay, Dr. Rose places a multifocal contact lens in the prospective patient’s nondominant eye. This demonstration allows patients to experience what their vision will be like with the inlay. “The wow factor is when we take it out, and patients realize what they had for a few minutes and is now gone. Then they want the procedure even more.”
Consider various methods of marketing.
Dr. Rose participated in two television news stories about the inlays through her local NBC and CBS affiliates and an Associated Press story sent to national media outlets. Drs. Bafna and Wiley market the inlays during patient consults for LASIK. Dr. Rebenitsch’s practice takes a different approach, marketing various solutions for reading glasses and bifocals, not just inlays.
Learn appropriate surgical techniques.
To incorporate these into your practice, you have to be an experienced LASIK surgeon, say those interviewed. Beyond any support offered by the device manufacturers, touch base with another ophthalmologist who has implanted a fair number of the inlays.
“Most surgeons think of it as being LASIK, and it’s almost a different animal in the sense that you have to create a pocket for Kamra as opposed to a flap,” Dr. Bafna says. “The technology works extremely well, but you have to understand the nuances so that you can be successful with it.”
Results can depend on the depth of the inlay placement, Dr. Bafna adds. He shoots for a depth of 250 μm to 300 μm for the Kamra inlay and 150 μm to 200 μm for Raindrop, which can yield less inflammation and quicker vision recovery.
Make sure patients understand pricing.
Patients tend to think the inlays will be expensive, but the pricing is similar to LASIK at around $4,000, says Dr. Kelly. (He points out that that price is for the Raindrop eye alone; if he performs LASIK on the fellow eye, the charge to the patient is $5,000.)
For the ophthalmologist who already has and is proficient with a femtosecond laser, the only expense is the inlays themselves.
Build in extra time for consults.
When patients see this new technology on the news or hear about it on the radio, “they don’t want to wait three months for their consultation,” Dr. Rose says. “We opened our schedule immediately when the TV pieces came out” and scheduled all interested patients as quickly as possible.
Dr. Rebenitsch’s group has added several presbyopia consults to the schedule, “because we know that they’re going to take longer.”
Until these corneal inlays’ approval, presbyopes had no real options. I was either LASIK and reading glasses, or monovision LASIK, says Dr. Rose. “We’ve really never had any good options for presbyopes in terms of laser vision correction. We had been looking and looking for a solution for many, many years.” OM
REFERENCES
- Moussa K, Jehangir N, Mannis T, et al. Corneal refractive procedures for the treatment of presbyopia. Open Opthalmol J. 2017 Apr 27;11:59-75.
- Moarefi MA, Bafna S, Wiley W. A review of presbyopia treatment with corneal inlays. Ophthalmol Ther. 2017 Jun;6:55-65.
- FDA press release. FDA approves implantable device that changes the shape of the cornea to correct near vision. https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm509315.htm . Accessed July 26, 2017.
Disclosures:
Dr. Bafna and Dr. Wiley are consultants for AcuFocus and ReVision Optics.
Dr. Rose is a consultant for ReVision Optics.
Dr. Rebenitsch has received speaking honoraria from AcuFocus.
Dr. Kelly reported no relevant financial disclosures.
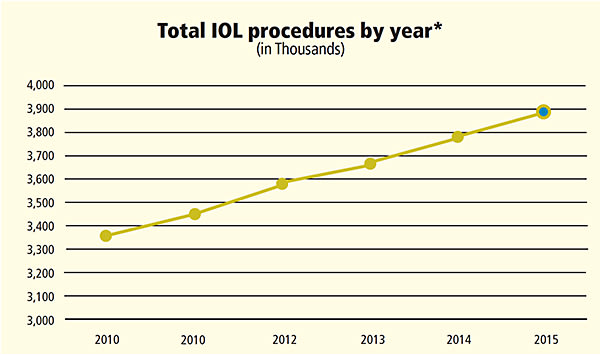
*Data courtesy Market Scope January 2015 survey with 261 cataract surgeons. https://tinyurl.com/y6vcp2s7








