Treating ocular surface disease takes more than physician experience. It takes a positive attitude on the part of staff, as well as the patient. The reason: A physician’s time is limited. Most ophthalmologists see 30 to 60 patients a day, which curbs their face time with the patient.
When addressing a messy, multifactorial disease state like OSD, limited time with patients leaves a vacuous space between patient presentation and diagnosis/treatment. This space is filled by their under-celebrated right hands: technicians and staff.
I have had the good fortune of visiting a fair number of clinics wanting to improve their Dry Eye Center of Excellence (DECOE). The common denominator of the successful clinics (patient outcomes) appears to be the staff. There must be a champion in every DECOE to lead the way.

STAY EVEN KEEL IN A SEA OF CHANGE
The most successful OSD-treating clinics I have seen share a positive “growth mentality.” These clinics react as a team, they share a comfort level with change while remaining upbeat, flexible and creative. Like a champion sailing crew, they distribute the workload, navigate the waves and sail the winds of change to smooth the overall ride. In the process, they create something meaningful and effective for everyone involved.
Like the youngsters in my daughter’s elementary school class, they strive for the three Cs and three Rs: courage, curiosity and confidence, while being respectful, resourceful and responsible.

SURVEY STAFF
I wanted to explore the underpinnings of positive attributes of successful staff, while remaining mindful of the increasing workload involved in DECOEs. While I always knew that technicians were the unsung heroes of a successful clinic, the depth of feeling we uncovered revealed a previously underestimated level of interest, engagement and altruism.
Among the 50 respondents,* who came from a variety of clinic sizes across the country, half reported having dry eye themselves; 35% said they didn’t, while 15% reported possibly having dry eye. When asked how they felt about OSD, only 7% felt it distracted them from their other work or that it took too much time. Approximately 33% of respondents felt that it was rewarding to help educate patients, and 65% said it is rewarding to help patients get better.
Among the diagnostic and therapeutic offerings, 96% reported using vital dyes (fluorescein, lissamine green, rose Bengal), 75% use tear osmolarity testing (TearLab), 75% use MMP-9 testing (InflammaDry, RPS), 75% offer LipiFlow (TearScience), 73% offer BlephEx, 55% use meibomian gland imaging (LipiScan, TearScience or other imaging system), 35% offer IPL (Lumenis M22) and 0.5% offer radiofrequency treatments (ThermiEyes).
Technician respondents reported a high level of interest in learning and incorporating new tests and therapeutics (on average four of five stars on the survey, with five stars being the highest level of interest). In a ranking question asking technicians how they prefer to learn about a new OSD diagnostic or therapeutic, the highly preferred method was “from the clinic doctor” followed by “from the representative.” This response shows that we may underappreciate the importance that physician engagement brings to technician education — they want to hear from the physician. It stands to reason that the physician’s attitude with respect to ocular surface disease, be it a fun challenge, a nuisance, a way to enhance refractive and cataract surgery outcomes, will set the tone in the practice. In other words: Captain, lead your sailing crew.
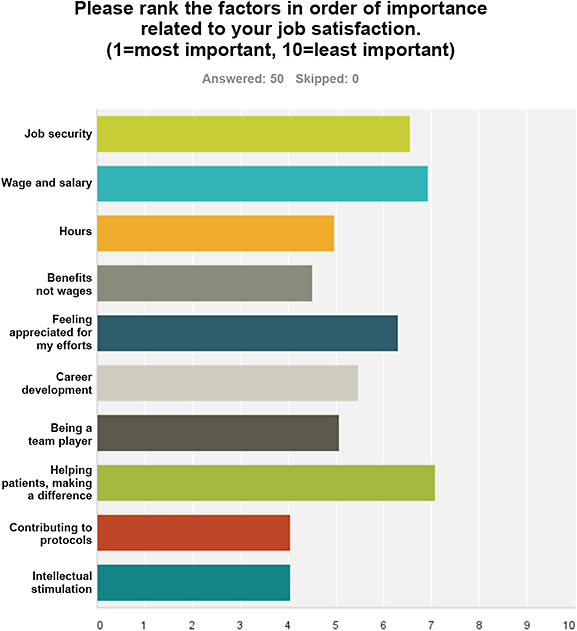
A four- out of five-star job satisfaction rating in helping dry eye patients suggests a deeper level of technician engagement. Techs again demonstrated their buy-in by ranking “learning new information” as the top appreciation of new technology and therapeutics. “Helping patients and making a difference for them” led the pack among job satisfaction factors, followed by “feeling appreciated.”
FIND JOY
When asked about feelings toward their current job, positive comments such as “I often see how my work helps patients” or “I have moments of insight into the difference I make” dramatically outweighed negative comments such as “It’s a job.” Clearly, technicians are responsible, respectful and resourceful. The open comments included overwhelmingly positive entries, such as “Our work is an integral part of the patient care model that helps the doctors to work more effectively and make an impact on patient experiences and outcomes” and “I work closely with patients and insurance so a lot of the process is frustrating when medications get denied; however, the reward and education I get to offer is exciting and ever-changing.”
Regarding technicians’ methods to increase job satisfaction, “earn new certificates,” “learning the science and importance of new technologies and therapeutics” and “I hear how it has enhanced or improved my patient’s life” significantly outranked “compensation,” “flexibility and autonomy” and “protected administration time.”
We hypothesized that compensation would rank highest among motivational factors. Interestingly, it was smack in the middle. Our curious, confident and courageous techs ranked intrinsic motivation above extrinsic motivation. This is further evidence of their substantial value as part of the dry eye team. And that deserves … compensation.
Lastly, feeling appreciated is an important component of job satisfaction among the technician respondents. This question explored the five most common modes of appreciation: words, deeds, gifts, time, touch. “Words of appreciation” topped the list and “time” was second. “Raises” (technically deeds or gifts) was the most common topic in the open comments section.
A “pat on the back” received the bottom rank across the board (as anticipated, given workplace considerations) but technicians noted that they enjoy “notes, cookies or hugs from happy patients.” The open comments again revealed their positive attitudes, such as, “What I get to do every day is very rewarding. I am privileged to be part of this team.”

A JOB WELL DONE
Physician attitudes toward OSD are complex and varied. I’ve witnessed virtually every spectrum and combination of physician and technician attitude toward OSD models, from altruistic to apathetic. In exploring the technicians’ perspectives, I am most impressed by our staff’s depth of commitment and engagement. We did not explore whether this is unique to a messy, rapidly evolving, diagnostic-heavy and patient education-dependent field like OSD or if this is common to all ophthalmic subspecialties.
This survey cemented for me how critical technicians are to the clinic; I have an even higher appreciation for their contribution to the positive outcome of the OSD patient. Appreciating, acknowledging and perhaps even leaning on the contributions and talents of these compassionate and engaged helpers are powerful ways to enhance their satisfaction. Perhaps this has a carryover effect to patient satisfaction — and perhaps even physicians’ job satisfaction. Reach for the gold star. OM
*The survey remained open as of the writing of this article.









