Maintaining and monitoring a large IOL inventory has always been a challenge for our ASC. Now that many of the 17 cataract surgeons in our busy center (Figure 1) are implanting a variety of toric and presbyopia-correcting IOLs, it has become an even more complex endeavor. To better manage the complexities, we have created some new policies and procedures designed to ensure IOL availability and simplify the selection process.

IOL Availability
Ensuring the ASC has the correct lens for every patient is crucial for smooth patient flow and a successful surgical outcome. We recently implemented a new policy in our ASC, mandating a 6-day window between adding a case to the surgery schedule and the actual day of surgery to allow time to ensure the correct IOL is available.
My colleagues and I frequently perform intraoperative wavefront aberrometry with the ORA System (Alcon). If there’s a chance a patient may need a toric lens, both the toric and non-toric versions of that lens power will be ordered, as well as IOLs at least two power steps above and below the anticipated lens implant, just in case the ORA indicates a need for a different lens power intraoperatively.
We also order enough IOLs so that we have backup lenses for all powers we need in a given week, just in case an IOL is torn or dropped. This is especially important when we have cases outside the normal ranges, such as low- or high-power IOLs outside the typical 17.0- to 23.0-D range. We want to avoid discovering on the day of surgery — or worse, when the patient is already in the OR — that the correct IOL isn’t available.
Because space is always an issue, our ASC limits stock of IOLs that are used less often, and, whenever possible, stocks IOL platforms with a full complement of spherical monofocal, toric, and presbyopia-correcting lenses. We primarily use the Tecnis platform (Abbott) and Bausch + Lomb lenses (Crystalens, Trulign, and enVista). This helps to streamline our inventory and maintain efficiency when ordering lenses. Our ASC keeps lenses in a centrally located corridor that is easily accessible from the operating room (Figure 2). We have tried some automation systems for IOL restocking and did not find them satisfactory. Instead, each day, the staff places an IOL label from each IOL that is used onto a document. At the end of the day, that document is faxed to the IOL company so the necessary lenses can be restocked.
IOL Selection
Many factors should be taken into consideration when selecting the right IOL for a patient. I perform wavefront aberrometry on all refractive cataract patients preoperatively to select a lens that best matches the patient’s spherical aberration (SA) profile and degree of angle kappa.
My patient population is above the average SA of +0.27 µm, so if a patient of mine desires spectacle independence, I typically use a lens with negative asphericity, such as the -0.27µm Tecnis IOLs, or, less frequently, the -0.17 µm Acrysof IOLs (Alcon) for maximum depth of focus. If a patient doesn’t mind wearing eyeglasses, I might choose a forgiving lens with neutral asphericity, such as the enVista. I also implant asphericity-neutral lenses in patients who have had hyperopic LASIK, as that procedure can induce negative SA. Magnifying that with a lens with negative asphericity often makes patients feel that their vision is out of focus even if they achieve 20/20 Snellen acuity.
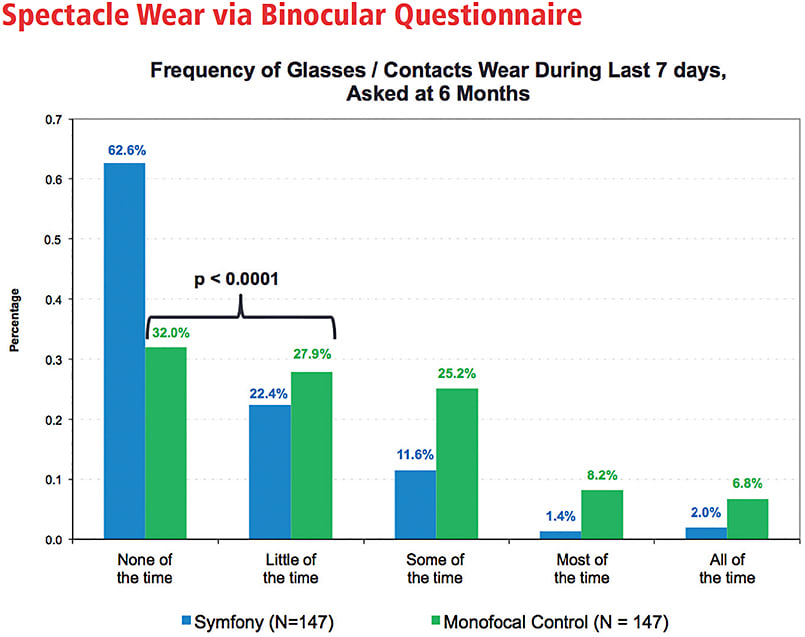
I also take into account angle kappa, or the difference between the center of the pupil and the center of the visual axis where the patient actually fixates. Angle kappa readings from a wavefront aberrometer can reveal whether or not a patient is a good candidate for a multifocal lens. In a patient who has a large degree of angle kappa, minor decentration of the lens (>0.4 mm) increases the risk of higher-order aberrations that aren’t correctable with eyeglasses or contact lenses. Such patients are better candidates for an accommodating IOL or an extended-depth-of-focus lens, such as the Tecnis Symfony (Abbott), which allows for up to 0.75 mm of decentration and has been shown to offer very high rates of spectacle independence (Figure 3).
The presence, degree, and type of astigmatism also can influence IOL selection. I’m much more likely to choose a toric lens when presented with a large amount of astigmatism or against-the-rule (ATR) astigmatism. Posterior corneal astigmatism can decrease total corneal astigmatism in eyes accompanied by with-the-rule (WTR) astigmatism and increase it in eyes with ATR astigmatism, so it is important that we compensate for the posterior contribution in our cylinder power calculations.1
We also have a number of options to give patients with astigmatism a chance to reduce spectacle dependence at near. In the past, I’ve chosen to implant a multifocal or accommodating IOL with limbal relaxing incisions or the Trulign toric. Now, I can also consider the Tecnis Symfony lens, which comes in four toric powers and has a high tolerance for residual astigmatism. A patient with 1.0 or even 1.5 D of cylinder can still maintain very good distance vision with this lens.
Patient desires and lifestyles also factor heavily into lens choice, especially in discussions of add power in multifocal lenses. For example, a male patient recently came in seeking spectacle independence after lens surgery. He is a makeup artist who needs to see fine details at a very close near point of about 14 inches. This is an unusual situation in which a conventional, high-add multifocal IOL might be ideal. Most patients, however, will be more comfortable in the 18- to 20-inch range, and thus do well with mid- and low-add multifocal IOLs. Asking patients about activities, such as night driving or those that require up-close vision, can narrow the selection of suitable presbyopia-correcting IOLs.
Incorporating a New IOL
ASC owners and staff must also keep up with the latest technology and developments in IOLs. The Symfony lens was recently added to our ASC; that implementation went smoothly because it is so similar to other IOLs within the Tecnis platform and because we were able to incorporate both spherical and toric versions of the lens at the same time. Its versatility made it a good choice for an ASC, and we expect the patient base for this lens to broaden with experience and time, especially with regard to astigmatic patients. Assessing how a lens may fit into an ASC before beginning to implant it provides a higher chance for success.
Advance Planning = Success
Identifying the ideal IOL type and power for each patient is half the battle; the other half is putting in place systems to ensure that the ASC has all the IOLs that will potentially be needed for each surgical day. Stocking an ASC with a range of versatile IOLs makes it easier to maintain inventory and meet patient needs. Keeping lenses accessible, ordering them well in advance, and making sure the inventory is up-to-date takes pressure off the ASC staff, minimizes the potential for error, and maximizes opportunities for exceeding patient expectations. ■
Reference
- Koch DD, Ali SF, Weikert MP, Shirayama M, Jenkins R, Wang L. Contribution of posterior corneal astigmatism to total corneal astigmatism. J Cataract Refract Surg. 2012;38(12):2080-2087.









